What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Food As Trigger Of Flare
Participants frequently discussed the possibility that certain foods could trigger flares, but had great difficulty in identifying common themes across participants.
I never could figure out what triggers it. When Ive got a flareup going, I mean, its always, I eat, and then half an hour later Im in the bathroom.
I know until I kept a food journal, I had no concept of what would or wouldnt trigger it. I just its hard to isolate.
Many Disease Activity Indices Exist For Ulcerative Colitis But None Have Been Developed With Formal Patient Input
There is no consensus gold standard for the evaluation of disease activity in ulcerative colitis. This is illustrated in numerous recent clinical trials, in which investigators measured several different indices of disease activity, as no one index is considered sufficient. There are many indices for the measurement of ulcerative colitis disease activity, including Truelove and Witts classification of mild, moderate, and severe disease the St Marks Index, which empirically added endoscopy in 1978 simplified versions of the St Marks Index, including the Ulcerative Colitis Disease Activity Index and the Mayo Score and noninvasive versions, including the Seo Index and the Simple Clinical Colitis Activity Index .
The diversity of indices suggests that none of these has proven satisfactory, and none was developed with patient input. In addition, it has never been established that any of these indices actually measures all of the important symptoms of ulcerative colitis.
Ulcerative colitis lacks a validated measurement instrument such as the Crohns Disease Activity Index in Crohns disease . Furthermore, the indices that do exist for ulcerative colitis were not constructed in a patient-centered manner to attempt to capture the symptoms experienced by patients. Therefore, our study group aimed to investigate through focus groups that what symptoms does patients with ulcerative colitis experience during their disease process.
Recommended Reading: What Is The Treatment For Diabetic Foot Ulcers
Moderate Or Extensive Disease
Patients with inflammation proximal to the sigmoid colon or left-sided disease unresponsive to topical agents should receive an oral 5-ASA 5-Aminosalicylic Acid Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder or corticosteroid therapy as well as those who are corticosteroid-dependent. Moreover, a combination of immunomodulator and anti-TNF therapy Anti-TNF drugs Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder (see Crohn disease treatment and ulcerative colitis read more is sometimes helpful. Finally, in some patients who fail to respond to corticosteroids, immunosuppressants, or biologics, a trial of the Janus kinase inhibitor tofacitinib, or a trial of sphingosine 1-phosphate receptor modulator ozanimod can be considered.
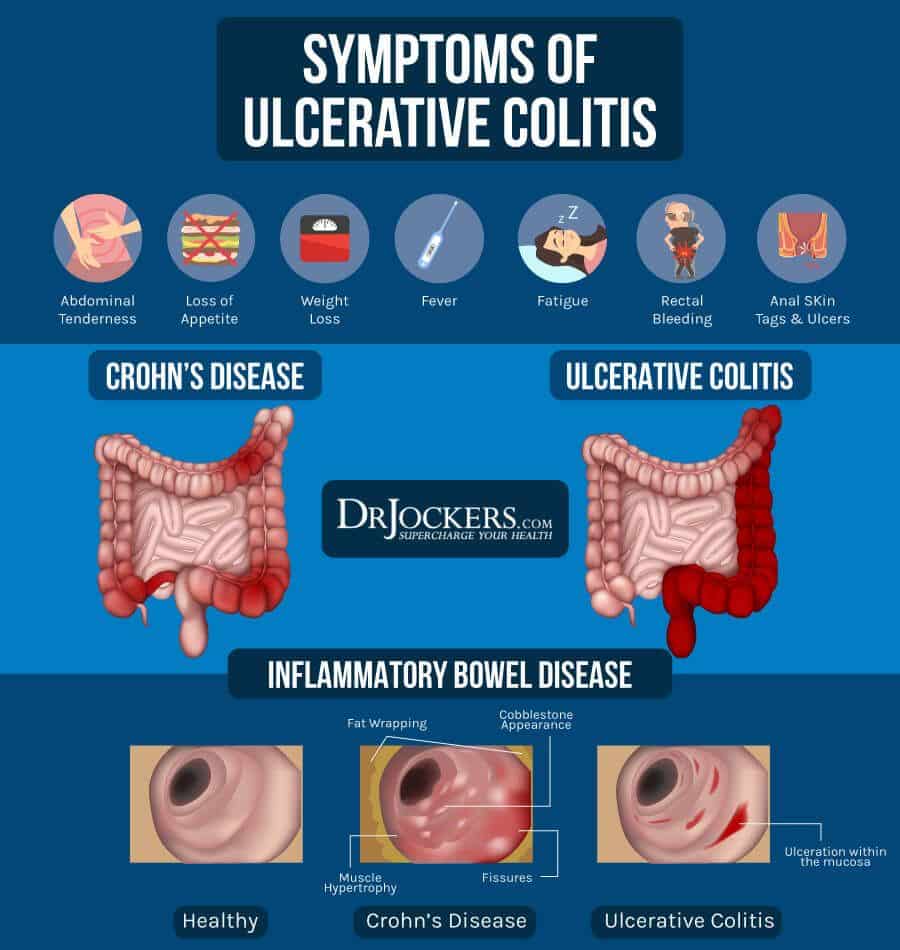
Ulcerative Colitis Is A Type Of Ibd
There are two main types ofinflammatory bowel diseases ulcerative colitis andCrohns disease. Ulcerative colitis is more common worldwide than Crohns disease.
It causes inflammation and sores in the large intestine and may affect part or all of the large intestine.
Ulcerative colitis can happen at any age, but it is more likely to develop in people between the ages of 15 and 30, or older than 60 years of age.
Ulcerative colitis needs to be diagnosed by a health care provider. While there are no cures, there are treatments.
You May Like: Can You Donate Plasma If You Have Ulcerative Colitis
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Questions To Ask Your Health Care Provider
- How often do I need to see a gastroenterologist?
- How often do I need to undergo testing?
- What are my risks for colon cancer?
- Are there symptoms that should cause worry? If so, what are they?
If you dont know something at any point, ask for more information! For some, hearing that they have ulcerative colitis is a relief, a reason for symptoms and a light at the end of the tunnel. For others, it can be scary and daunting. Many will have a mix of feelings.All of this is completely normal.
You May Like: Natural Remedies For Stomach Ulcers In Humans
Ischemic Causes Of Colitis
The colon can be thought of as a hollow muscle. It requires a normal blood supply to deliver oxygen and nutrients for the muscle to function normally. When the colon loses its supply of blood and becomes ischemic , it may become inflamed. Ischemia or lack of blood supply causes inflammation of the colon leading to pain, fever, and diarrhea .
- As a person ages, the arteries that supply blood to the colon gradually narrow and can cause ischemic colitis. Risk factors for narrowed arteries are the same as atheroscleroticheart disease, stroke, and peripheral artery disease . These include diabetes, high blood pressure, high cholesterol, and smoking.
Read Also: How Would You Know If You Had A Bleeding Ulcer
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Don’t Miss: What Do Diabetic Ulcers On The Feet Look Like
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
You May Like: Can Tylenol Cause Stomach Ulcers
Mild To Moderate Disease
First-line therapy in mild to moderate disease is the 5-ASA drugs, which can be administered as suppositories, enemas, or oral formulations . There does not appear to be any difference in efficacy or safety between different 5-ASA formulations.119 Sulfasalazine, which is metabolised to 5-ASA, appears to have similar efficacy to 5-ASA drugs, but tends to be less well tolerated.114 Patients with proctitis should be treated initially with 5-ASA suppositories since they directly target the site of inflammation and appear to be more effective than oral 5-ASA.114,118,120 In left-sided colitis, 5-ASA should be administered as an enema instead of a suppository in order to reach the splenic flexure. For patients with left-sided or extensive disease, it is recommended that oral 5-ASA be used in combination with topical 5-ASA to induce remission.114,118 Oral 5-ASA doses of 2 g or higher per day are more effective than lower doses at inducing and maintaining remission.121123 5-ASA can be started at a dose of 2.02.4 g per day and increased up to 4.8 g, if needed.114,123 Dosing of 5-ASA once a day has similar efficacy to divided doses and could increase adherence.114,123 Patients typically see a response within 14 days, but this response might take up to 8 weeks for symptomatic remission.114 5-ASA drugs have also been shown to be effective at maintaining remission, and patients who achieve remission with 5-ASA should continue on the same medication.114
Most Symptoms Of Ulcerative Colitis Relate To Bowel Movements
The symptoms of ulcerative colitis can vary from person to person, based on where the disease is in the body and how bad the inflammation is.
Most common symptoms:
- Diarrhea , which is often the first symptom.
- Blood in the stool.
- Urgency, or immediate need, to go to the bathroom.
- Increased number of bowel movements.
- Belly pain and cramping.
Ulcerative colitis can cause symptoms throughout your body.
You might have weight loss or other symptoms that affect the entire body. The inflammation of ulcerative colitis can also affect your joints or skin, leading to painful joints and skin rashes. During a flare-up, symptoms may go beyond those that affect the digestive system, including:
- Rashes or patches of red, swollen skin.
- Painful or swollen joints.
- Red, irritated eyes.
Keep of track of any symptoms, how often you have them, and how bad they are to talk about with your health care provider.
Also Check: When Does Ulcerative Colitis Develop
How We Care For Ulcerative Colitis
At the Boston Childrens Inflammatory Bowel Disease Center, our team believes that, with proper management, all children and teens with ulcerative colitis can live comfortably. We partner with you and your child to effectively manage IBD and provide support through all life stages, from school and relationships to work.
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
Rectal preparations are particularly good at treating urgency and bleeding, symptoms that often are very bothersome. A positive response often occurs within days of treatment.
Also Check: Is Ulcerative Colitis The Same As Diverticulitis
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
You May Like: Icd 10 Stage 3 Pressure Ulcer Sacrum
Moderate To Severe Disease
Patients with moderate to severe colitis should be managed with thiopurines or biological drugs, or both . Thiopurines can be used in patients with steroid-dependent moderate to severe disease to maintain remission. Several small studies129,130 reported the modest efficacy of methotrexate in ulcerative colitis, but results of a clinical trial131 were mixed therefore, its role in ulcerative colitis treatment is still being investigated.
Suggested treatment approach algorithm for moderate to severe ulcerative colitis
Based on Toronto Consensus and European Crohns and Colitis Organisation guidelines.114,118 5-ASA=5-aminosalicylic acid. IV=intravenous. DI=dose intensification.
Anti-TNF- drugs, such as infliximab, adalimumab, and golimumab, are effective at inducing and maintaining remission in moderate to severe disease.132135 Infliximab can also be used in patients admitted to hospital with severe ulcerative colitis and remains the most widely used biological for ulcerative colitis.132,133 Azathioprine alone is less effective than in combination with infliximab to achieve both clinical remission and endoscopic healing, while the difference is statistically significant only for endoscopic healing between azathioprine alone and infliximab monotherapy .136
Read Also: Booties To Prevent Pressure Ulcers
What Are The Risk Factors Of Ulcerative Colitis
The cause of ulcerative colitis is unclear, but its thought that a combination of genetics and environmental factors are at play. Up to 20 percent of people with ulcerative colitis have a parent, sibling or child with the disease.
Ulcerative colitis is more common for people living in urban, industrialized areas compared to undeveloped countries, which indicates that highly refined diets may play a role. Although all ethnic groups are affected, the problem is most common among Caucasians and people of Eastern European Jewish descent.
Lastly, there appears to be a connection to nonsteroidal anti-inflammatory medications. Its not that these medications cause the disease but, because they inflame the bowel, they can worsen symptoms. This category of medication includes ibuprofen , naproxen sodium and diclofenac sodium .
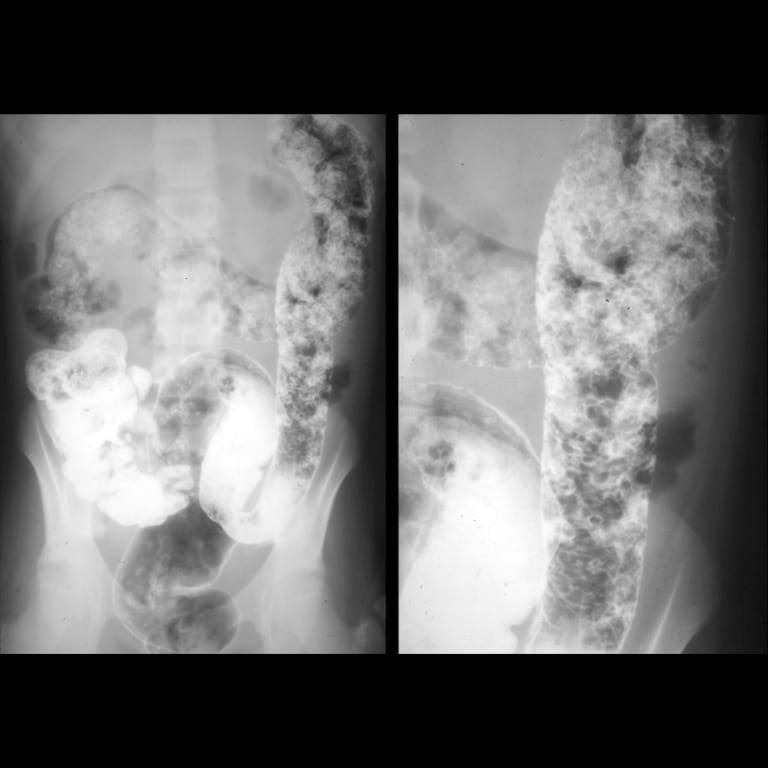
Getting Tested For Ulcerative Colitis
There are many tests your gastroenterologist can do to find out if you have ulcerative colitis. First, he or she will take your past health and family health info, listen to your symptoms, and do an exam to feel and listen to your belly. No one test makes the diagnosis, but testing is used to confirm the gastroenterologists clinical suspicion that ulcerative colitis is causing symptoms.
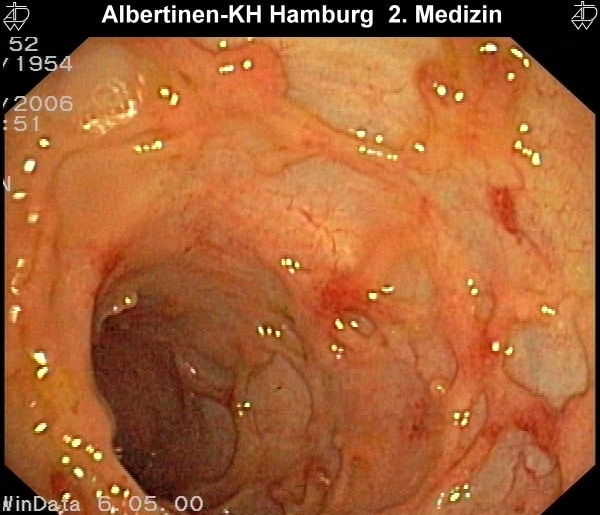
Ulcerative colitis is diagnosed by the presence of the common symptoms and endoscopic and biopsy findings of long-term inflammation in the large intestine.
Talk to your doctor about which test is best for you. Your doctor will tell you how to get ready for your test for ulcerative colitis.
This testcan be done in a doctors officeand does not need anesthesia or sedation .
Sigmoidoscopy is a test during which a doctor uses a short, thin , flexible tube with a tiny camera on the end tocheck the rectum and the lower end of the colon for polyps and cancer. Only the final two feet of the colons six feet are examined.
Introduction of the flexible tube may be somewhat uncomfortable, and some cramping may happen during the test.
You will need to take a couple of cleansing enemas before the testand/or a gentle oral prep.
You may be given medicine to make you relaxed and sleepy during this test.
After the test, there may be some mild belly-gas pains.
Don’t Miss: Nursing Assessment For Ulcerative Colitis
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Recommended Reading: Can Ulcerative Colitis Cause Heart Problems