Treating Stage 1 Bedsores
Bedsores at stage 1 are very treatable. Although they usually could have been prevented, hopefully your loved ones caretakers will have noticed the sores by stage 1 and begin treating them immediately. At stage 1, bedsores can be treated by identifying and eliminating the cause.
Causes of bedsores include:
- Friction on skin
Bedsores are often caused by lack of movement putting pressure on a specific area. A caretaker or nurse can move the patient to relieve pressure on the place where they have developed the sore. Once the pressure is relieved, the sore should heal on its own within a few days.
One simple way that pressure can be relieved on a sore is by propping up that part of the body with a pillow. Sores can also be helped by certain types of bedding or mattresses that put less pressure on the body.
Stage 1 bedsores should also be washed with mild soap and water, then dried. Caretakers should continue to help patients move regularly and monitor their skin to make sure they dont develop new sores.
Other ways to treat bedsores include improving nutrition, increasing fluid intake and reducing friction when moving.
What Are The Potential Complications Of Bedsores
Infection is the most common of bedsores. Pressure ulcers can cause:
- cellulitis, or infection of the surrounding skin and soft tissues
- bone or joint infection, which can cause pain and difficulty with movement
- , a full-body infection that can be life threatening
Proper diagnosis and timely treatment of bedsores can prevent most of these complications.
What Are The Benefits Of This Treatment
It can take several months of bedrest for a severe wound to heal on its own. All pressure must be off the area while in bed, which can be very hard to do on an ongoing basis. If pressure is put on the area while in bed, it can delay healing or make the wound worse. Plus, there is an increased risk of infection with any open wound. The longer the wound is open, the longer the higher risk continues. If an infection develops, there is a risk that it can spread and become life-threatening.
The obvious benefit of this treatment is that the wound can heal much quicker than it would without the treatment. Your doctor can explain all your benefits, but here are a few of the benefits:
- Much less time needed for bedrest
- Lowered risk for infection
- Increased independence to enjoy meaningful activities
- Lowered healthcare costs
Don’t Miss: Cure For Peptic Ulcer By Diet
Complications From Stage 4 Bedsores
If left untreated, stage 4 ulcers can lead to a number of serious complications, such as:
Infection: Stage 4 ulcers are often open wounds that are prone to infection. If not treated promptly, an infection can spread and become life-threatening. Bone and joint damage: Pressure ulcers can damage the bones and joints underneath. This can lead to long-term problems, such as joint pain and stiffness.
Nerve damage: Stage 4 pressure ulcers can damage the nerves around the sore. This can cause numbness, tingling, and muscle weakness. In severe cases, it can lead to paralysis.
Skin grafting: In some cases, skin grafting may be necessary to treat a stage 4 pressure ulcer. Skin grafting is a surgical procedure in which skin is taken from another area of the body and transplanted to the pressure ulcer.
Death: If left untreated, stage 4 pressure ulcers can be fatal. This is why it is so important to seek treatment as soon as possible if you think you may have a pressure ulcer.
If you have a stage 4 bedsore, it is important to see a doctor or other healthcare professional right away. They will be able to provide you with the treatment you need to heal your pressure ulcer and prevent complications.
Sores On Buttocks Cheek
The buttocks cheek is prone to skin infections that may be difficult to notice. Infection of the hair follicles also called folliculitis are common. Such infection will in most cases heal on their own without treatment. They may also spread causing boils which will require antibiotics to cure.
Sores on buttock cheek are likely to affect people who are bed bound. The sores can become quite severe leading to ulceration and a significant loss of skin around the buttocks. A number of causes that could lead to sores on buttocks include:
- Skin conditions such as rashes
Below are the pictures of how sores on buttocks look like
You May Like: What To Do For Ulcerative Colitis Flare Up
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
The Available Reconstructive Options Are
Split thickness skin grafting
When the ulcer is superficial and vital tissues such as bone, vessels, nerves or tendons are not exposed, and the ulcer is not copiously discharging, skin grafting is the first option for surgical treatment. The slimy layer over the surface of ulcer is sharply debrided to get a healthy vascular bed for skin grafting.
Local flaps
Variety of local flaps can be used to reconstruct the defect created by excision of pressure ulcers. Local transposition, rotation, limberg flap are the available options .3]. Biceps femoris V-Y advancement for ischial pressure sore and perforator based V-Y advancement is another good options if the anatomy permits .
Sacral pressure sore , debridement and cover by local perforator based V-Y advancement flaps , 1-month post-operative , recurrence on the flap after 11 years due to loss of family support and subsequent improper care. Another patient with the same flap after 16-year of follow-up with a proper weight shifting and care showing stable coverage
Regional flaps
Medial planter flap for heel sore: A long-standing deep trophic ulcer of heel . The islanded medial planter flap was transposed to the defect and the resultant donor site was covered by split thickness skin graft . The 1-week and 3-month post-operative pictures showing stable coverage. Patient allowed full weight bearing from 6th week along with silicone footpad protection
Microvascular free flaps
You May Like: Ulcerative Colitis Caused By Alcohol
Recommended Reading: How Do You Cure Ulcerative Colitis
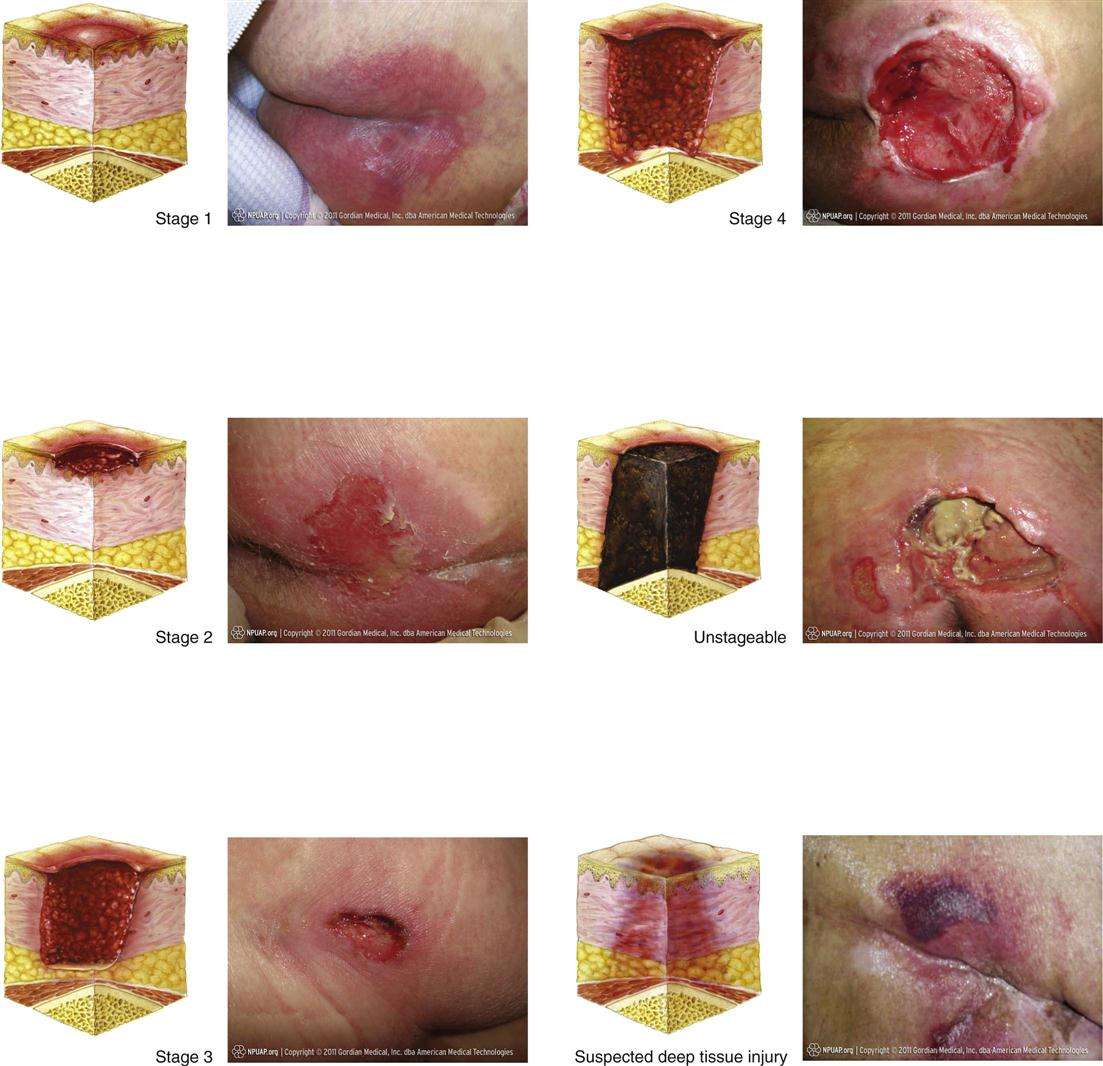
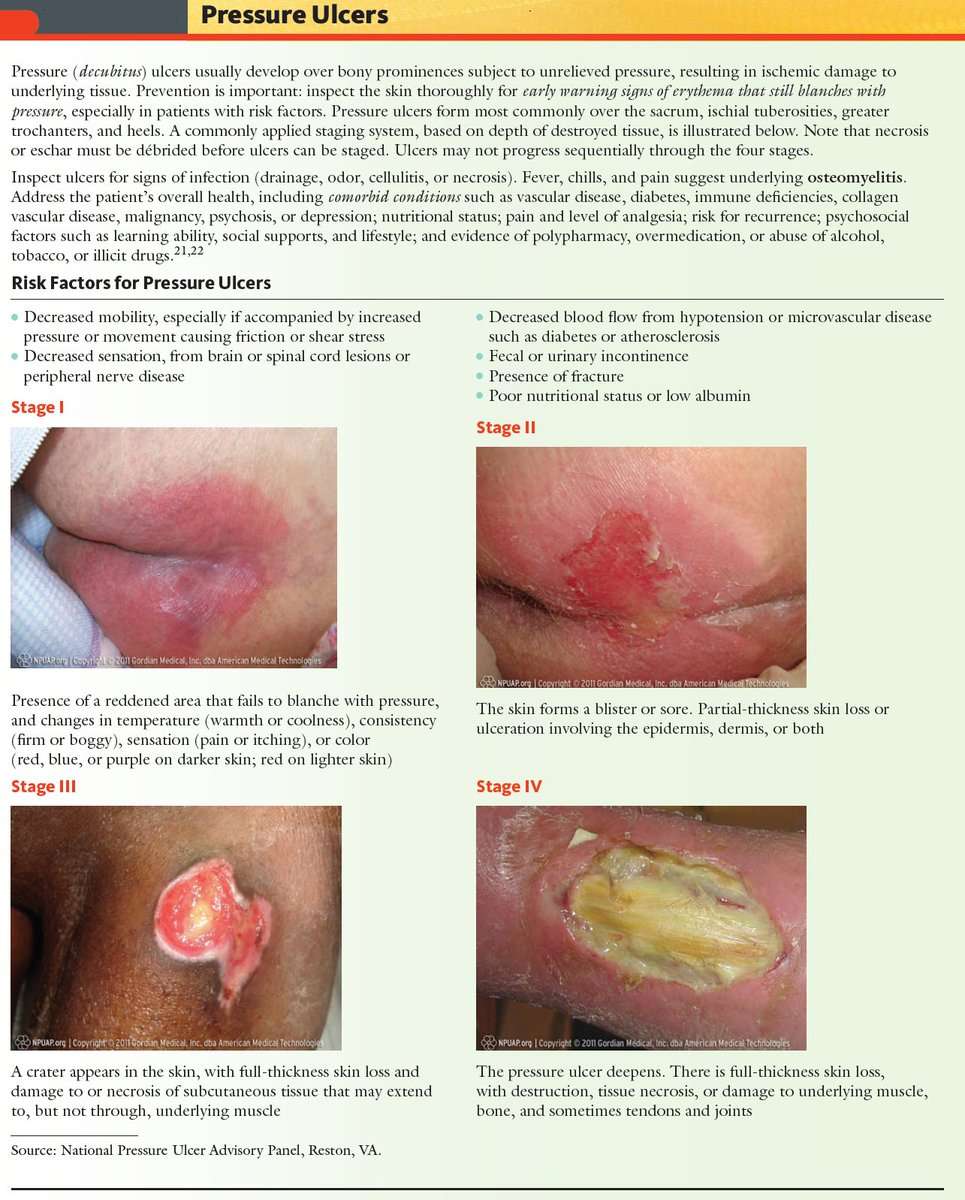
Description Of The Condition
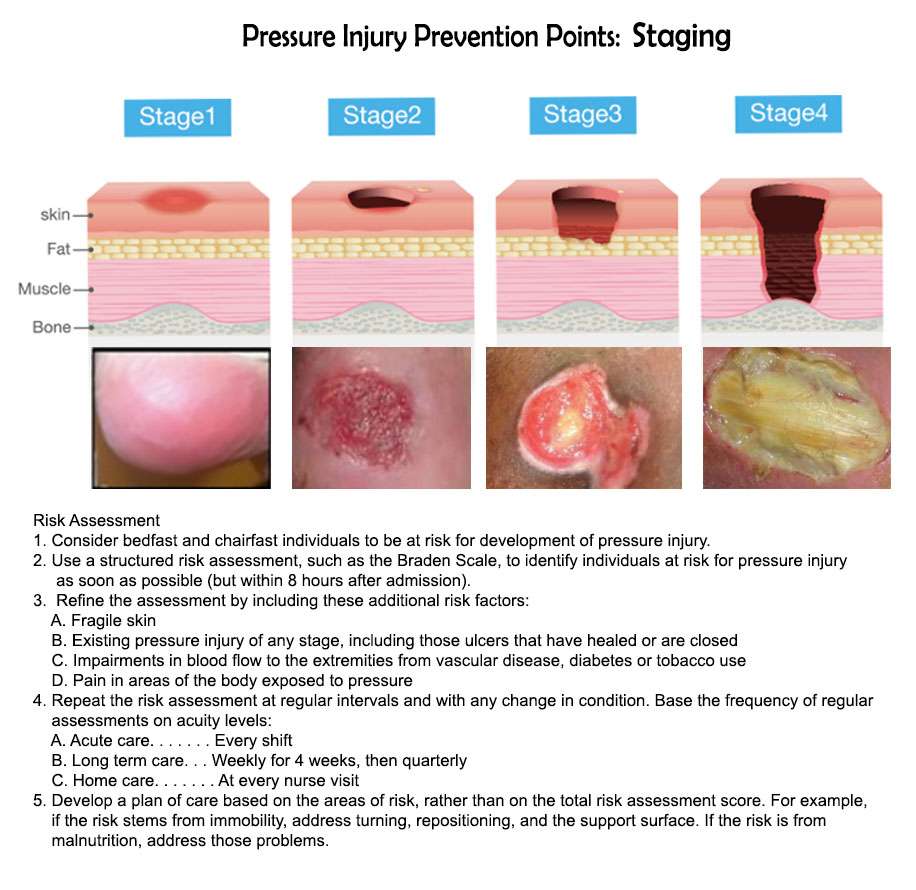
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
The Challenge To Manage Pressure Ulcers
We all want to avoid pressure ulcers. Considerable progress has been made in this area the past few years. Nevertheless, pressure ulcers remain a challenge. B. Braun offers different solutions including products for skin care, wound bed preparation and infection management, as well as exudate management. Taking action right from the start helps you to prevent the aggravation of existing pressure ulcers and to support the healing process.
You May Like: How To Cure Skin Ulcer
Keep Skin Clean And Dry
- Bathe daily with mild soap and warm water and rinse and dry thoroughly. Pay particular attention to keeping the genital area and skin folds clean and dry.
- Immediately wash and dry skin and change clothing after any leakage of stool or urine.
- Avoid harsh soaps, skin agents with alcohol, and antibacterial or antimicrobial soaps. Do not use powders. Use a moisturizer that has been approved by your health care provider.
How Do You Treat Bedsores
Stage 1 and stage 2 bedsores to protect the skin and prevent the sores from getting worse.
If the affected individual is otherwise healthy, keeping pressure off the affected area and keeping it clean and dry may be sufficient to allow the sore to heal. Special pads can cover and protect pressure points. Egg crate foam mattresses and pads can reduce pressure across a wider area. Silk-based fabrics can help reduce friction on the skin compared to cotton fabrics.
Large stage 2 and stage 3 and 4 bedsores require medical treatment. A doctor or nurse may recommend covering the sore with a protective dressing, such as a hydrocolloid dressing. Dressings can absorb drainage, keep the wound clean, and prevent additional friction to the affected area.
Some bedsores contain dead tissue that can interfere with healing. A doctor may need to remove the dead tissue.
If a bedsore is infected, the doctor may order . Antibiotics can be applied topically or administered orally or through a vein .
Read Also: Nursing Care Plan For Pressure Ulcer Prevention
Those Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but you are more at risk if you:
- have to stay in bed after surgery or because of illness
- are unable to move some or all of your body
- have urinary incontinence and bowel incontinence
- have a poor diet
- have a medical condition that affects blood supply or makes your skin more fragile
How Can Pressure Ulcers Be Treated
It is important to watch out for early signs of pressure ulcers and to contact your doctor if you notice any changes to the skin. Ulcers are best managed early on, and your doctor will assess whether your pressure ulcer can be managed at home, if you need a referral to a wound specialist or if you require treatment at hospital.
Use healthdirects Service Finder tool to locate your nearest GP or nurse clinic.
Wound dressings can enhance healing. Your healthcare team will select the most appropriate treatment and dressing, depending on your specific pressure ulcer. There are 6 classes of dressings:
- alginate absorbent fibre dressings
Depending on the type of pressure ulcer, a bandage may also be applied to keep the dressing in place or support the injured area.
To promote healing and recovery, it is important to eat a balanced diet that includes protein, carbohydrates, fats and sufficient fluids.
Other treatments may include antibiotics if the ulcer becomes infected, or debridement a procedure used to clean the wound and remove any damaged tissue.
Also Check: Home Remedies To Cure Stomach Ulcer
Spotlight On Aging: Pressure Sores
|
Aging itself does not cause pressure sores. But it causes changes in tissues that make pressure sores more likely to develop. As people age, the outer layers of the skin thin. Many older people have less fat and muscle, which help absorb pressure. The number of blood vessels decreases, and blood vessels rupture more easily. All wounds, including pressure sores, heal more slowly. Certain risk factors make pressure sores more likely to develop in older people: |
Causes that contribute to the development of pressure sores include
Pressure on skin, especially when over or between bony areas, reduces or cuts off blood flow to the skin. If blood flow is cut off for more than a few hours, the skin dies, beginning with its outer layer . The dead skin breaks down and an open sore develops. Most people do not develop pressure sores because they constantly shift position without thinking, even when they are asleep. However, some people cannot move normally and are therefore at greater risk of developing pressure sores. They include people who are paralyzed, comatose, very weak, sedated, or restrained. Paralyzed and comatose people are at particular risk because they also may be unable to move or feel pain .
Friction can lead to or worsen pressure sores. Repeated friction may wear away the top layers of skin. Such skin friction may occur, for example, if people are pulled repeatedly across a bed.
-
Assessment of nutrition status
-
Sometimes blood tests and magnetic resonance imaging
The Efficacy Of Duoderm
A study by Michel Hermans treating small partial-thickness burns found that HydroColloid Dressings provide an optimum wound environment for more rapid re-epithelialization than either allografts or SSD. The cosmetic and functional results were also excellent.1 A meta-analysis of pressure ulcers performed by Matthew Bradley comparing a hydrocolloid dressing with a traditional treatment suggested that treatment with the hydrocolloid resulted in a statistically significant improvement in the rate of healing compared to wet-to-dry dressings.2
Don’t Miss: How Do You Know If You Have A Stomach Ulcer
What Causes Bed Sores
The main reason for the formation of erosion on the hips, buttocks, lower back, shoulder blades is excessive friction and pressure on the skin as a result of maintaining the same position for a long time. The skin becomes moist and not sufficiently ventilated. Immobility leads to a decrease in blood flow to the affected areas and inflammation of these areas.
Bedsores are more common in people with such disorders as:
- incontinence, feces
- Very dry, dehydrated skin.
Risk factors include the use of long-term corticosteroids alcohol consumption smoking the presence of malignant tumors, edema, hip fractures, infections, injuries of the spinal cord.
Dont Miss: How Do You Get Ulcers In Your Mouth
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Also Check: Ulcerative Colitis And Bloody Stool
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the âcontrolâ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
How Are Pressure Sores Diagnosed
Your doctor will do a physical exam to look at the sores. They will examine the size and depth of the sore and look to see if blood or fluid is oozing from the sore. Your doctor will check to see if your sore has a bad smell. They also will check for additional sores.
Testing may help to diagnose pressure sores or their complications. These tests might include a blood test. Another test would be to take a sample of the tissue from the sore. This is done by scraping or cutting it from the sore. That sample is sent to the lab for examination.
Recommended Reading: Psc Liver Disease Ulcerative Colitis
Review Question: What Are The Most Reliable Techniques/tools To Measure The Dimensions Of A Pressure Ulcer
One systematic review looked at the performance of instruments designed for measuring the dimensions of pressure ulcers. This systematic review was included in the current evidence review and it was subsequently updated to include 1 other study . Overall 13 studies were included in the evidence review.,,,,,,,,,,,, Evidence from these is summarised in the clinical GRADE evidence profile below. The quality of these studies is outlined in .
The OMeara review looked at studies of any design which reported an evaluation of a pressure ulcer measurement instrument as the main focus of the investigation. The authors did not include assessment checklists where the focus was the performance of the tool overall rather than the measurement of pressure ulcer dimensions.
Also Check: Mouth Ulcers Treatment Home Remedies
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation |
|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Also Check: How Do I Know If I Have An Ulcer