Inflammatory Bowel Disease Treatment
Unfortunately, there currently is no cure for ulcerative colitis or Crohns disease. However, those living with IBD can live full and healthy lives. And with ongoing research, improved treatments are constantly being tested and approved for use.
Treatment for IBD generally focuses on relieving the associated inflammation. This often begins with dietary changes. There is no single diet or eating pattern that helps people with IBD, so working with a registered dietitian at Beaufort Memorial can help patients identify the foods that trigger IBD symptoms and develop a nutrition plan that fits with their tastes and lifestyle. Understanding how the body responds to certain foods helps fend off flare-ups and ensures optimal overall health.
Anti-inflammatory drugs are also helpful in calming inflammation and bringing relief. When used appropriately, medication can lead to long-term remission of symptoms. Finding the best medical treatment may require patients to go through a series of medications until determining which one works best and causes the fewest side effects.
In cases when medication and changes to diet arent sufficient, surgical intervention may become necessary. In surgery for Crohns disease, for example, the diseased part of the GI tract is removed and the healthy parts are reconnected. This offers long-term symptomatic relief but may have to be repeated in the future as the disease progresses.
Diagnosis And Assessment Of Disease Activity
The diagnoses of Crohns disease and ulcerative colitis are made on clinical grounds supplemented with objective findings of radiological, endoscopic, and histological examination. In some cases, the diagnostic evaluation must be repeated after a certain period of time has passed. There is no gold standard for diagnosis . When establishing the diagnosis, one must exclude other inflammatory, toxic, vascular, neoplastic, and infectious etiologies of enteritis and/or colitis .
Ulcerative Colitis Complications Vs Crohns Disease Complications
When it comes to potential complications due to ulcerative colitis or Crohns disease, there are some that these two diseases share, and others that are more likely to occur in one versus the other, according to a 2017 study published in the Journal of Gastroenterology.6
- Colon cancer: People with ulcerative colitis, we well as people who have Crohns disease that affects most of their colon, do have a slightly increased risk of developing colon cancer.Screenings will typically be recommended 810 years after an IBD diagnosis, and your doctor will let you know how frequently youll need screening.
- Primary sclerosing cholangitis: Inflammation can cause scarring of the bile ducts . This can lead to liver damage.
- Blood clots: Both people with ulcerative colitis and Crohns have a greater risk of blood clots, though it isnt entirely clear why. It may be due to genetic predispositions coupled with severe inflammation in the GI tract, according to Cedars Sinai.
- Medication side effects: The medications used to treat both conditions can potentially increase the risk for certain cancers, like lymphoma, when used long-term. Consistent corticosteroid use is also associated with things like high blood pressure and osteoporosis.
Don’t Miss: How Do You Know If You Have A Stomach Ulcer
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Research And Clinical Trials: Advancing Care Of Crohns Disease And Ulcerative Colitis Through Cutting
At the Mass General Crohns and Colitis Center, we believe in integrating outstanding clinical care with cutting-edge research to offer answers that address the needs of our patients and advance scientific understanding of these complex diseases. We believe that every patient can significantly improve our knowledge of Crohns disease and ulcerative colitis, contribute understanding the factors that influence the development of these diseases, behavior of the disease and response to treatments. All of our physicians at the Crohns and Colitis Center are actively involved in research programs aimed at understanding the underlying cause of Crohns disease and ulcerative colitis, with the goal of developing more effective therapies and improve in our quality of life.
Interested patients can participate in research through enrollment in our ongoing patient registries, enroll in clinical trials of novel therapies, or participate in studies aimed at developing new treatment strategies including harnessing the dietary, lifestyle, and behavioral changes in the management of these diseases.
Don’t Miss: Off Loading Shoe For Heel Ulcer
How Can I Prevent Inflammatory Bowel Disease
While there isnt anything you can do to prevent IBD, certain dietary and lifestyle changes may control the symptoms. You can:
- Eat smaller meals every two to four hours.
- Find healthy ways to manage stress, such as meditation, movement like tai chi, listening to music or going for a walk.
- Get plenty of sleep and stay physically active.
- Keep a food diary to identify foods that trigger IBD flares. You may find you have a food intolerance, such as lactose intolerance. If so, your body has a harder time digesting certain foods, which causes stomach upset.
- Reduce foods that irritate the intestines, such as those that are fibrous, spicy, greasy or made with milk. During flares, choose soft, bland foods that are less inflammatory.
- Cut back on caffeinated, carbonated and alcoholic beverages. Drink more water to prevent dehydration.
Dont Miss: Best Dressing For Decubitus Ulcers
Ulcerative Colitis Treatments Vs Crohns Disease Treatments
While there is no cure for ulcerative colitis or Crohns disease at the moment, dont despair, research is moving quickly. There has been such a rapid advancement in the different options that are available now compared to 10 or 20 years ago, says Dr. Blazora.
Those advancements include things like anti-inflammatory medications, immunosuppressants , and biologicsthese are injected or received via infusionwhich are the newest class of medications that work to neutralize certain proteins that activate inflammation, according to the Mayo Clinic.
If medications arent doing the trick, surgery is always a treatment option in more severe cases. This is where things differ a bit between ulcerative colitis treatment and Crohns disease treatment. That could mean getting your entire colon removed if you have ulcerative colitis, which can signal the end of symptoms for some folks. Some people call the colectomy a cure, but technically, the disease is really systemic because it affects the whole body, so people can still have complications after the surgery, says Dr. Blazora.
Also Check: Bentonite Clay For Ulcerative Colitis
The 3 Key Goals Of Uc Treatment
There are treatments available that can help control excess inflammation in order to help you:
Controlling inflammation can help relieve UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain.
Controlling inflammation can also help you achieve and maintain remission. This means you have achieved ongoing symptom relief and are able to prevent flares.
Controlling inflammation over time allows the lining of the colon to heal and can help you maintain remission.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
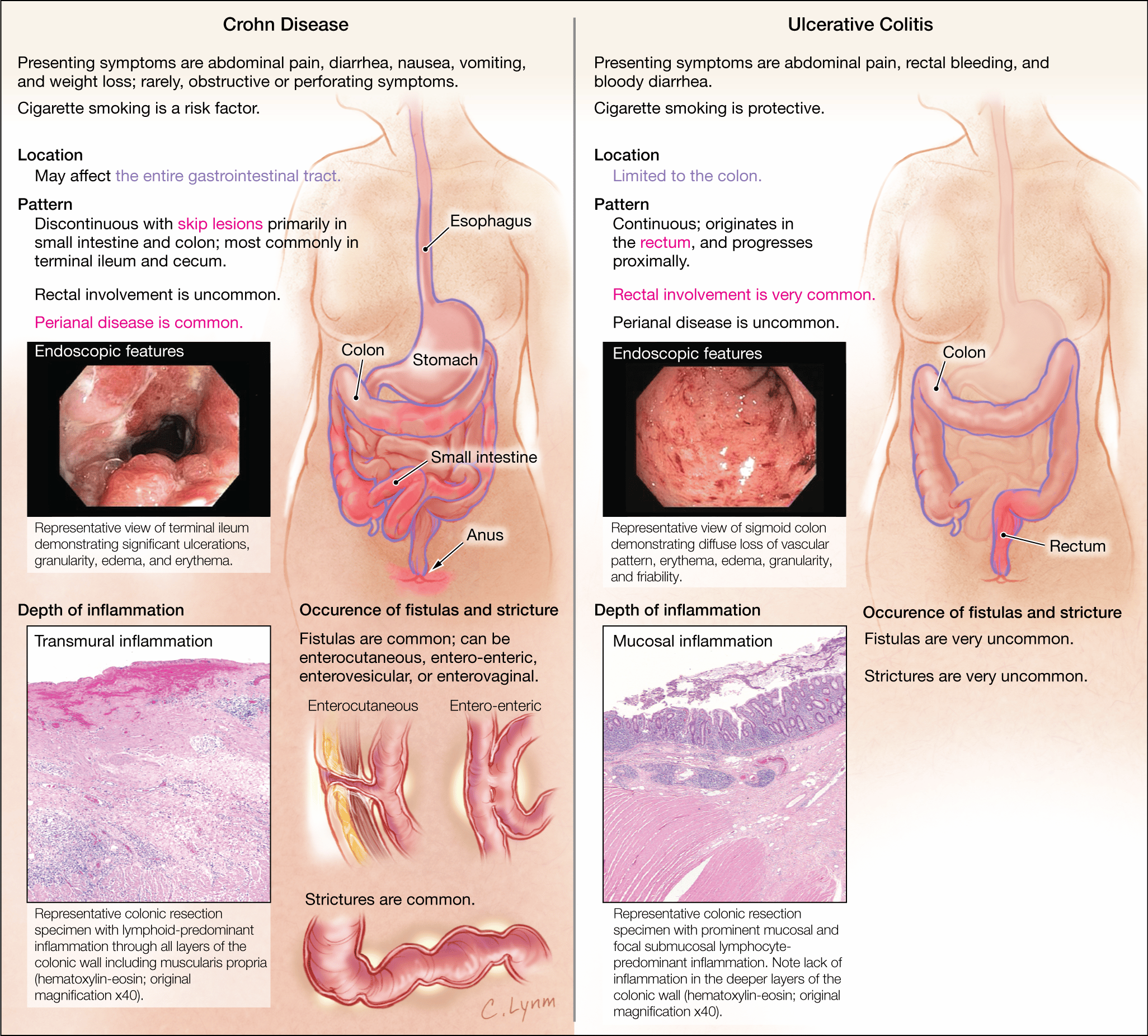
There are three key differences:
1. Location.
Ulcerative colitis affects only the large intestine.
But in Crohnâs disease, inflammation can appear anywhere in the digestive tract, from the mouth to the .
2. Continuous inflammation.
People with Crohnâs disease often have healthy areas in between inflamed spots. But with ulcerative colitis, there are no healthy areas in between inflamed spots.
3. Which layers are affected.
Because Crohnâs disease affects more of the GI tract, it can cause some problems that doctors dont usually see in people who have ulcerative colitis. For instance:
Recommended Reading: How To Heal Stomach Ulcers Naturally
What Causes Crohns Disease And Who Gets It
Like all types of IBD, experts still dont know what causes Crohns disease. It might be in response to an autoimmune reaction where your immune system attacks healthy cells in your body but doctors dont know for sure.
According to the National Institute of Diabetes and Digestive and Kidney Diseases you may be more at risk based on:
Digestive System Parts: A Brief Anatomy Overview
Now that we got that out of the way, lets take a deeper look at each of these conditions of the digestive tract.
Read Also: Foods That Irritate Stomach Ulcers
Ibd And Changing Your Diet
Some dietary changes that may help a person with IBD include:
- Low-fibre diet when IBD is active, most people find a bland , low-fibre diet helps to ease diarrhoea and abdominal cramping. People with Crohns disease who have a narrowed small intestine may need to eat a low-fibre diet most of the time.
- Low-fat diet people with Crohns disease who experience steatorrhoea may benefit from a low-fat diet.
- Low-lactose diet the milk sugar lactose is broken down by the enzyme lactase, commonly found in the lining of the small intestine. Some people with Crohns disease lack this enzyme, so should avoid milk and other dairy products. Lactose intolerance can be diagnosed with a simple test ask your doctor.
- Liquid diet a person with severe Crohns disease may need a nutritionally balanced liquid diet.
- Plenty of water people with IBD need to drink plenty of fluids to prevent dehydration.
Is There Such A Thing As An Ulcerative Colitis Diet Or A Crohns Disease Diet
What kind of food should I eat for ulcerative colitis? Should I follow a Crohns disease diet? These are questions that Dr. Blazora hears often from people with IBD. Diet is always a hot topic thats probably one of the first questions people ask me about after theyve been diagnosed, she says.
In short, diet mattersbut it depends on your personal triggers. If youre experiencing a Crohns or ulcerative colitis flare-up, dietary changes may help. We may tell you to take on a low-fiber diet or avoid lactose or caffeinated beverages or anything that can stimulate the bowel to produce more bowel movements, but its not going to change the course of the disease itself, Dr. Balzora says. That said, a 2021 study published in the journal Gastroenterology found that eating a Mediterranean style diet , and avoiding processed foods and foods high in sugar could be beneficial.7
However, while tweaking your diet may help you feel more comfortable, it may not get to the root of the issue. Its the medications that turn the tide, Dr. Balzora stresses. They really decrease the inflammation as opposed to diet.
Read Also: What Foods Should I Avoid With A Stomach Ulcer
When Surgery Is Needed
If medication isn’t reducing the inflammation and IBD progresses, surgery may be needed. This is where people with ulcerative colitis tend to fare better.
If the colon gets bad enough in ulcerative colitis, its removed and replaced with an internal pouch, which functions like a colon, says Cohen. According to the Mayo Clinic, colectomy surgery whether partial or full usually requires additional procedures that reconnect the remaining portions of the digestive system so they can still rid the body of waste.
However, things are looking up. A study published in December 2019 in the Journal of Gastrointestinal Surgery found that due to advances in medicine and medical care for IBD patients over the past decade, the number of hospitalized patients with ulcerative colitis who require a colectomy decreased by nearly 50 percent between 2007 and 2016.
According to the Crohns and Colitis Foundation, proctocolectomy with ileal pouchanal anastomosis usually called J-pouch surgery is the most common surgery performed on people with UC who have not responded to medication. Surgeons remove the rectum and colon and then create a temporary opening in the abdomen, called a loop ileostomy, which will allow waste to move from the small intestine into an ostomy bag that sits outside the body while the digestive system heals from the surgery. In some cases a stoma, or permanent opening in the abdomen that funnels waste into an external bag, is required, notes the Mayo Clinic.
Inflammatory Bowel Disease Conditions Require Long
Both Crohns disease and ulcerative colitis are conditions that fall under the umbrella term of Inflammatory Bowel Disease and both require management, and sometimes treatment, for a lifetime. However, with proper care from a facility that specializes in these diseases, you can expect to have a good quality of life. The University of Michigan Inflammatory Bowel Disease program is dedicated to the comprehensive medical and surgical treatment of adult patients with Crohns disease and ulcerative colitis. Our dedicated inflammatory bowel disease specialists exclusively treat IBD.
What you should know about Crohns and ulcerative colitis:
- Inflammatory Bowel Disease is an umbrella term that Crohns disease and ulcerative colitis fall under.
- Crohn’s disease and colitis are easily confused because both have similar symptoms and treatments, but also distinct differences. With a series of tests, your doctor can usually tell ulcerative colitis from Crohns disease however, in some cases the two diseases cant be distinguished from each other.
- The diseases affect men and women about equally.
- While the diseases can occur at any age, they often start between the ages of 15 and 25 and last a lifetime.
- Crohns disease is more common in people with a family history of the disease.
- Ulcerative colitis affects about 600,000 people in the U.S, while Crohns disease affects about 700,000 people.
Recommended Reading: What Is Moderate Ulcerative Colitis
What Is Celiac Disease
Celiac disease, sometimes also referred to as gluten-sensitive enteropathy or celiac sprue, is by far the most well-understood among these three inflammatory bowel conditions. Celiac disease is an excessive immune response to the ingestion of a protein known as gluten.
Gluten is a protein naturally found in certain grains like wheat, rye, and barley. Its also often added to countless processed foods and even products like supplements or lip balm. Most people can ingest gluten without any issues. But if you have celiac disease, consuming gluten can trigger a massive immune response.
As your immune system fights to neutralize and eliminate the gluten in your digestive tract, your own tissues can accidentally end up in the line of fire. This can lead to massive inflammation and damage to the lining of your upper small intestines .8
So what exactly causes the immune system to go haywire over gluten in celiac disease?
Keep Up With Your Checkups
If you have either condition, you’ll need to keep up with your checkups, even if your symptoms start to ease up.
You may also need to get colonoscopies more often and start them at a younger age. A colonoscopy can check for cancer or polyps that need to come out. Experts recommend that you start these tests within 8 to 10 years of developing UC or Crohnâs symptoms, and then typically every 1 to 3 years after that. Your doctor will tell you a schedule that is best for you.
Show Sources
You May Like: What Foods Not To Eat If You Have An Ulcer
Are You Struggling With Crohns Disease Ulcerative Colitis Or Celiac Disease
Are you or a loved one struggling with an inflammatory bowel condition? If so, the good news is, youre not at the mercy of your diagnosis. While we may not be able to cure these conditions, you have so much power over your own health. I cant overemphasize the importance and influence your diet, supplements, and lifestyle factors can have on your inflammation levels and symptoms.
So if youre ready to take your power and health back from one of these inflammatory bowel conditions, I recommend starting with the steps outlined in this article and seeking out the guidance of an experienced Integrative and Functional Medicine Practitioner. Theyll help you identify the root cause of your condition and come up with a personalized plan of action to begin healing.
And if youre hungry for more practical and research-backed tips on optimizing your health, you can head over to my blog and catch up on hundreds of articles that simplify healthy living.
What Symptoms Do Colitis And Ulcerative Colitis Share
Colitis can cause similar belly and bowel issues no matter the cause. Some symptoms are mild while others are more serious.
General signs of colitis and UC include:
- Stomach cramps that come and go
- Constant belly pain
- Mucus or blood in your poop
- Weight loss without trying
- An urgent need to poop
- A feeling like you didnât get all your poop out
If you have periods, you may have:
- Worsening diarrhea during your period
Recommended Reading: How Would You Know If You Have An Ulcer