Total Proctocolectomy With End Ileostomy
This proctocolectomy surgical procedure removes the colon, rectum, and anus, and creates an end ileostomy so that waste can exit your body into an ostomy bag.
-
This procedure is similar to the temporary ileostomy in the IPAA surgery, except the ileostomy will be permanent.
-
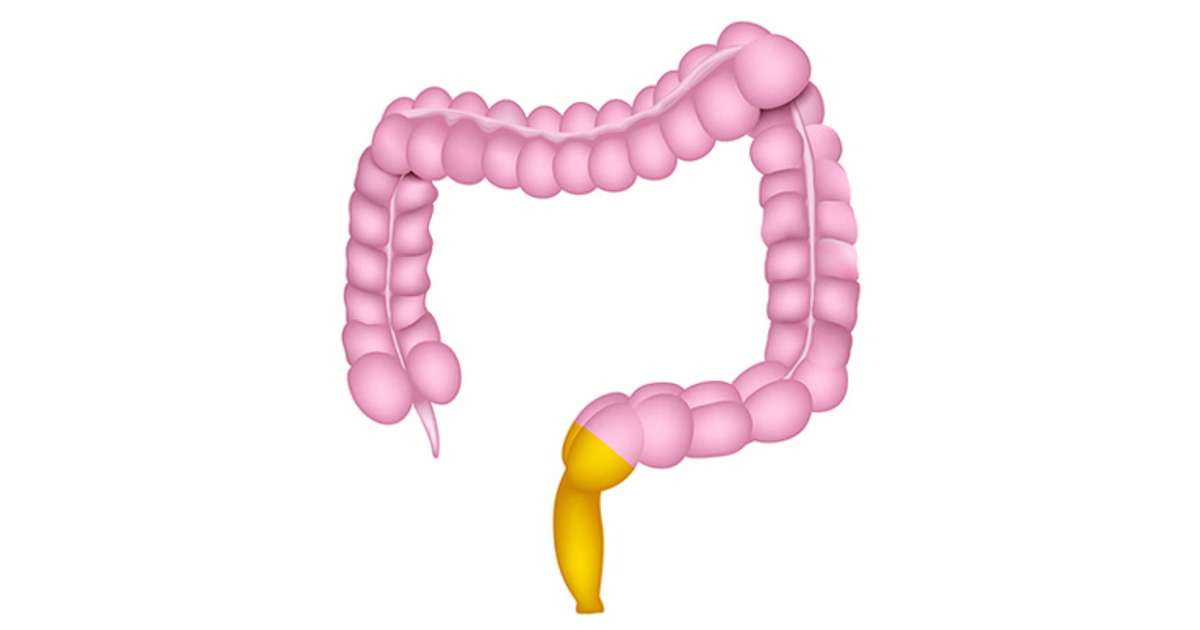
The stoma, or small hole created in the abdomen for the ileum, is about the size of a quarter, pinkish in color, and will appear moist and shiny. The stoma will protrude slightly outside of the abdomen.
-
After this surgery, you will wear an external ostomy pouch at all times to collect waste. The pouch must be emptied several times a day.
-
The ileostomy is usually placed in your lower abdomen to the right of your navel, just below the belt line.
Notify your doctor or other healthcare provider immediately if you experience these symptoms:
-
Infection from the surgery or at the site of the stoma
-
If no waste material exits the stoma for four to six hours and is accompanied by cramps and/or nausea, which could indicate a blockage
-
If your stoma is protruding more than normal outside of your abdominal wall, called prolapse, or retracting further inside your body, called retraction.
What Are The Signs And Symptoms Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Symptoms and Signs
Some individuals with colon cancer have no symptoms, and if they do have symptoms they often are minimalized and overlooked until the cancer becomes more severe. Cancer screening tests for colon cancer thus are important in individuals 50 years of age and older. Colon and rectum cancer can have many different symptoms and signs. If you have any of these symptoms, seek immediate medical help. You may notice bleeding from your rectum or blood mixed with your stool. It usually, but not always, can be detected through a fecal occult blood test, in which samples of stool are submitted to a lab for detection of blood.
People commonly attribute all rectal bleeding to hemorrhoids, thus preventing early diagnosis owing to lack of concern over “bleeding hemorrhoids.” New onset of bright red blood in the stool always deserves an evaluation. Blood in the stool may be less evident, and is sometimes invisible, or causes a black or tarry stool.
Rectal bleeding due to colon cancer may not be noticeable or chronic, and may only show up as an iron deficiency anemia, not colon cancer. Colon cancer may be associated with fatigue and pale skin due to the anemia. Changes in bowel movement frequency also is a symptom of colon cancer.
If the tumor in the colon becomes large enough, it may completely or partially block your colon. Symptoms of bowel obstruction include:
Ulcerative Colitis Symptoms and Signs
Common symptoms of ulcerative colitis include:
What Is The Difference Between Ulcerative Colitis And Pancolitis
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Read Also: What Foods Should You Avoid When You Have An Ulcer
Sudden Severe Ulcerative Colitis
This complication is the main cause of emergency surgery in patients with ulcerative colitis. With sudden, severe ulcerative colitis, medications and intravenous steroids, are unable to control the symptoms.
-
Uncontrolled bleeding can occur from deep ulcerations in the colon, though that is rare.
-
Severe, sudden ulcerative colitis can lead to toxic megacolon, a potentially life-threatening complication caused by severe inflammation.
-
Toxic megacolon leads to rapid enlargement of the colon. Symptoms include pain, distension or swelling of the abdomen, fever, rapid heart rate, constipation, and dehydration.
-
Toxic megacolon requires immediate treatment and surgery.
Do Different Types Of Ulcerative Colitis Cause Different Symptoms
Certain symptoms may point to different types of ulcerative colitis. These types, as outlined by the Mayo Clinic, are classified by location within the body:
- Ulcerative proctitis: With this form of the condition, which tends to be the mildest, a person has inflammation in the area closest to the rectum. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis: Inflammation with this form of the disease involves a persons rectum and lower end of the colon. Symptoms can include bloody diarrhea, abdominal pain, and an inability to go despite feeling like you need to let loose.
- Left-sided colitis: This involves inflammation from the rectum, through the lower colon, and into the descending colon. In addition to bloody diarrhea and abdominal pain on the left side, you may also experience weight loss. Most patients will have left-sided disease, Dr. Sinha says.
- Pancolitis: This usually impacts a persons entire colon, causing bloody diarrhea that can be severe, abdominal pain, fatigue, and rapid weight loss.
Read Also: Foam Boots For Pressure Ulcers
What To Expect After Your Surgery
Most people do very well after their surgery and are able to return to work and their normal daily activities after they recover.
-
You should expect an adjustment period of up to one year to get used to the changes in your body after your proctocolectomy.
-
You will likely be on liquid or soft food diet for the first few days after surgery. Your doctor will then have you slowly introduce bland solid foods. You should chew your food thoroughly and avoid any foods that may cause gas, diarrhea or anal irritation. Its also important to drink plenty of water. We recommend six to eight glasses a day.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantomrectum and it completely normal. It does not require any treatment and often subsides over time.
-
Your doctor may recommend a physical activity restriction for a minimum of six weeks, depending on what type of surgery you had.
-
Talk to your doctor about resuming normal sexual activity after your surgery. Some people find their sex life improves some time after surgery due to improvements in pain, inflammation, and other ulcerative colitis symptoms.
Differences Between Ulcerative Colitis And Crohn’s Disease
The differences between ulcerative colitis and Crohn’s disease are:
- Ulcerative colitis is limited to the colon while Crohn’s disease can occur anywhere between the mouth and the anus
- In Crohn’s disease, there are healthy parts of the intestine mixed in between inflamed areas. Ulcerative colitis, on the other hand, is continuous inflammation of the colon
- Ulcerative colitis only affects the inner most lining of the colon while Crohn’s disease can occur in all the layers of the bowel walls
Don’t Miss: Budesonide Vs Prednisone For Ulcerative Colitis
How Can I Find Support After An Ulcerative Colitis Diagnosis
When taking care of your physical well-being, dont forget that ulcerative colitis can take a toll on your emotional and mental well-being too. If it turns out your symptoms are ulcerative colitis, you can find a support group, or ask your doctor if they can connect you with a therapist or G.I. psychologist. Dr. Riehl, for example, works with patients on aspects of body image and even connects them with other patients who have experienced colectomy or ostomy . We talk openly about the impact that it can have on them from an intimacy perspective to how it impacts their self-identity, she says.
Since ulcerative colitis often starts at an age when people are thinking about their first job or starting a family, it can be particularly tough. One of the reasons that I and several of my colleagues went into this field is precisely because of thatso that we can hopefully make a difference in peoples lives early, and have them be able to lead productive and complete lives by putting their disease in remission, Dr. Sinha says.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
Also Check: Causes Of Ulcers In Horses
Pathogenesis Diagnosis And Management Of Ulcerative Proctitis Chronic Radiation Proctopathy And Diversion Proctitis
Reprints: Bo Shen, MD, Department of Gastroenterology & Hepatology-A31, The Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195 .
Supported in part by the Ed and Joey Story Chair and the National Natural Science Foundation of China .
The authors have no conflicts of interest to disclose.
Inflammatory Bowel Diseases
Can Lifestyle Changes Help Relieve Ulcerative Proctitis Symptoms
Remember, ulcerative proctitis is an autoimmune disease, meaning you didnt do anything to cause it. Even in remission, theres a risk of disturbing the very fine balance within the colon that can tip a flare-up, Dr. Lerrigo says. Its not the patients fault.
However, he says there are a few things you can do to try and support a healthier GI tract.
The perfect diet doesnt exist because each person has unique nutrition needs, explains Dr. Lerrigo. Thats why most of his patients work with a registered dietitian. However, experts do know that a diet that closely mimics the Mediterranean diet, one that is focused on fiber-rich whole grains, leafy vegetables, nuts, legumes, lean proteins like chicken and fish, and some dairy if you tolerate it, promotes a healthy gut ecosystem2 and reduces the risk of ulcerative proctitis flares, Dr. Lerrigo says.
He also recommends getting plenty of exercise and doing your best to manage stress, both of which can impact the immune system.
You May Like: Ulcer On Eye From Contact Lens
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
Medications Used To Treat Ulcerative Colitis
Currently, there is no cure for ulcerative colitis. The goal of medical treatment, therefore, is to modulate the inflammatory response. Several groups of drugs are used to treat ulcerative colitis. They are:
Recommended Reading: What Is Ulcer Pain Like
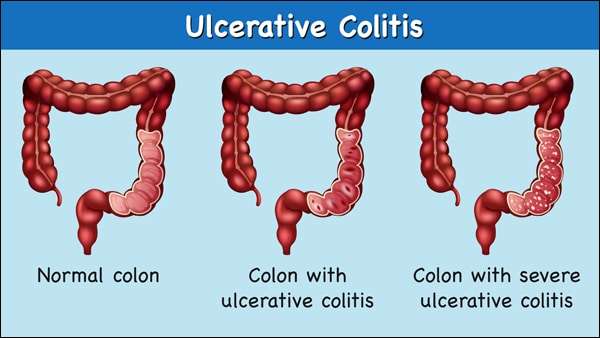
Types Of Ulcerative Colitis
Becoming well-informed about your chronic illness is a helpful part of your journey. It is important to learn all you can about your diagnosis and how it may affect you. We can help you understand the different types of ulcerative colitis, as well as the common symptoms and complications.
Ulcerative colitis is a chronic illness that can affect different parts of the colon and rectum. There is a wide array of symptoms and complications depending on the extent of your disease and the type of ulcerative colitis you have.
Getting diagnosed with a chronic, lifelong disease is overwhelming. It is important to learn all you can about your diagnosis and how it may affect you. We can help you understand the different types of ulcerative colitis, as well as the common symptoms and complications.
Complementary And Alternative Medicine
Probiotics may modestly reduce disease activity in active disease, but do not increase remission rates.34 However, Lactobacillus GG and Escherichia coli Nissle 1917 have been shown to be as effective as 5-ASA for maintenance therapy.16,17 Acupuncture has shown a small symptomatic benefit in active disease.35 Wheatgrass has also shown some effectiveness in reducing symptoms of active disease.36
Also Check: How To Reduce Stomach Ulcer
Do You Know The Different Types Of Uc
From left-sided ulcerative colitis to proctosigmoiditis, learn how the types of this condition differ and what that can mean for your symptoms.
Alamy
If you have ulcerative colitis , you know the range of symptoms the disease can cause from extremely urgent bowel movements to passing blood in your stool to pain and cramping caused by inflammation. But you may be less familiar with the different types of UC, as well as how each can impact the symptoms you experience and how the disease develops.
Ulcerative colitis can be characterized by both severity how badly inflamed the colon is at the site of disease activity and what areas of the colon it affects. These two factors in combination can explain a lot about why you experience certain symptoms.
What Are The Types Of Ulcerative Colitis
Another way to categorize ulcerative colitis is by identifying what areas of the colon it affects, as seen in a colonoscopy. According to Stein, UC always affects the rectum, the lowest section of the colon. But it may also affect higher parts of the colon.
There are four main types of UC based on how much of the rectum and the colon are affected:
Ulcerative Proctitis This form of UC usually affects less than six inches of the rectum and is found in about 30 percent of people at the time of diagnosis. Because of its limited extent, it tends to be associated with less severe disease and fewer complications.
Proctosigmoiditis This form of UC affects the rectum as well as the sigmoid colon, located just above the rectum. Proctosigmoiditis tends to be more severe than ulcerative proctitis, frequently causing symptoms such as bloody diarrhea, cramps, and tenesmus .
Left-Sided Colitis Inflammation extends even farther up the colon in this form of UC, to a point where it bends near the spleen. It tends to be even more severe, with common symptoms including diarrhea, bleeding, loss of appetite, weight loss, and severe abdominal pain on the left side.
Pan-Ulcerative Colitis This form of UC involves inflammation throughout the entire colon and tends to be the most severe variation with the greatest risk of complications that require surgery. Symptoms often include severe diarrhea, bleeding, cramps, abdominal pain, and weight loss.
Recommended Reading: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
Peptic Ulcer Vs Ulcerative Colitis
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Colitis And Chronic Ulcerative Colitis
Colitis is inflammation of the lining of the colon that causes abdominal pain, diarrhea and bloody stools. A bout of colitis that lasts for several days and then decreases may result from certain foods, medications, or an infection. Chronic ulcerative colitis, however, is a more serious immune system disorder that can last decades and require long-term medical therapy. This type of colitis is closely associated with Crohn’s disease, another inflammatory bowel disease .
For more information or to schedule an appointment with a Virginia Mason gastroenterologist, call 223-2319.
- Bloody stools
Read Also: Is Nausea A Symptom Of Ulcer
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
How Is Ulcerative Proctitis Treated
Ulcerative proctitis is usually very responsive to treatment, says Dr. Yoon. Your doctor will likely start by prescribing topical therapy, which means youll either use a suppository or an enema with an anti-inflammatory medication called mesalamine.
Dr. Yoon explains that the recommendation is to either use it every single night or at least two or three times a week just to keep the inflammation from coming back. If it works, you should ideally continue using it every night moving forward.
But in a practical sense, most people dont want to do that. People with ulcerative proctitis are usually young, in their 20s, so getting them to use a suppository for the rest of their life is wishful thinking, Dr. Yoon says. I have patients do it for four weeks and if theyre feeling fine and symptoms are mild, they can go ahead and stop. In the future, if they start bleeding again, they can do it for another four weeks.
Treatment for ulcerative proctitis can also include corticosteroids, such as prednisone or budesonide, which help reduce inflammation. Treating ulcerative colitis in general can involve immune system suppressors, like the pill azathioprine, and biologics, which are antibodies given via IV infusion or an injection that stop certain proteins from causing inflammation, according to the Crohns & Colitis Foundation.
Don’t Miss: Food To Avoid For Ulcer Patient