What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
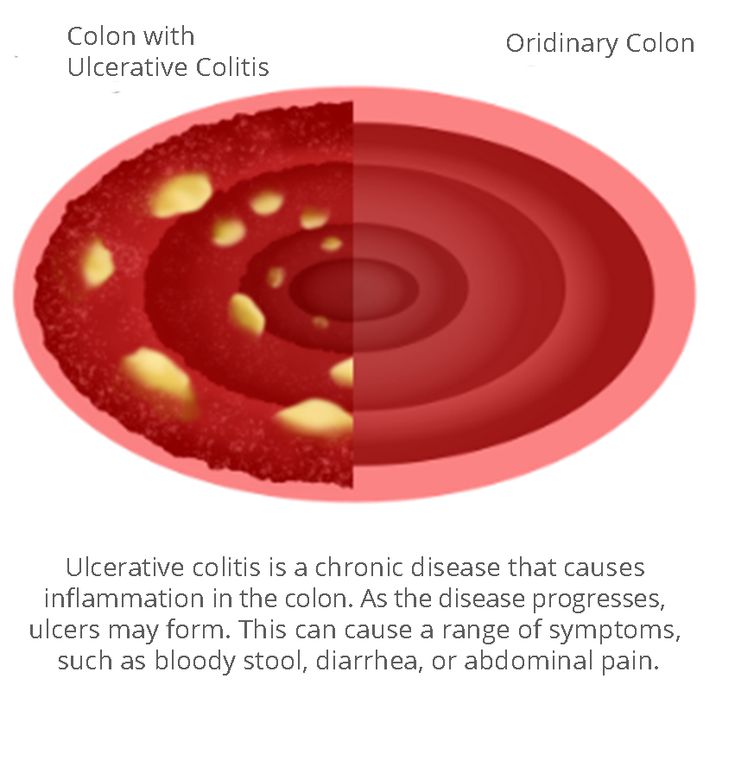
Is Colitis A Serious Disease
There are different types of colitis, with different causes. Some are short-lived and easy to treat, like when you have a bacterial infection from food poisoning. Other types called inflammatory bowel diseases are more chronic and difficult to treat. Colitis is more serious when it doesnt go away. A severe case can do serious damage to your colon over time. It also affects your quality of life.
Soins De La Colite Ulcreuse Pour Les Patients Du Nj Du Ct Et Du Md
Chez Regional Cancer Care Associates, les patients trouveront un environnement calme et accueillant où ils pourront recevoir des traitements de perfusion sous la supervision d’un professionnel de la santé agréé. Avec plusieurs pratiques emplacements, Regional Cancer Care Associates sert des patients dans tout le New Jersey, le Connecticut, le Maryland et la région de Washington, DC. Pour en savoir plus sur les services de perfusion chez Regional Cancer Care Associates, Contactez-nous dès aujourdhui.
Read Also: How To Fix A Stomach Ulcer
Its Not Irritable Bowel Syndrome
IBD and irritable bowel syndrome are confused a lot because their abbreviations are so similar, said Dr. Streett, noting that irritable bowel syndrome is much more common.
In people who have irritable bowel syndrome, they have symptoms that are linked to digestive function, but they do not have objective findings such as inflammation in the GI tract, she explained.
Inflammatory bowel diseases are disorders where there is inappropriate inflammation in different segments of the GI tract, Dr. Streett said. It is diagnosed by doing a colonoscopy to look for and biopsy areas that are inflamed.
Some of the symptoms overlap, but they’re really completely two different diseases and syndromes, said Dr. Gruss. Additionally, if you have IBS, it is not a precursor of IBD.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
You May Like: Ulcerative Colitis Prednisone Not Working
Alternative Medicine / Treatments
Itâs important to discuss any alternative medicines you may be taking with your doctor, as some may negatively impact your bodyâs response to traditional therapies.
- Herbal supplements â Most alternative therapies and supplements are not regulated by the FDA, which means they may not be safe or effective.
- Probiotics â Research is limited and results have not been proved, but researchers suspect that adding more good bacteria to the digestive tract may have a positive effect in people with ulcerative colitis.
Testimonial
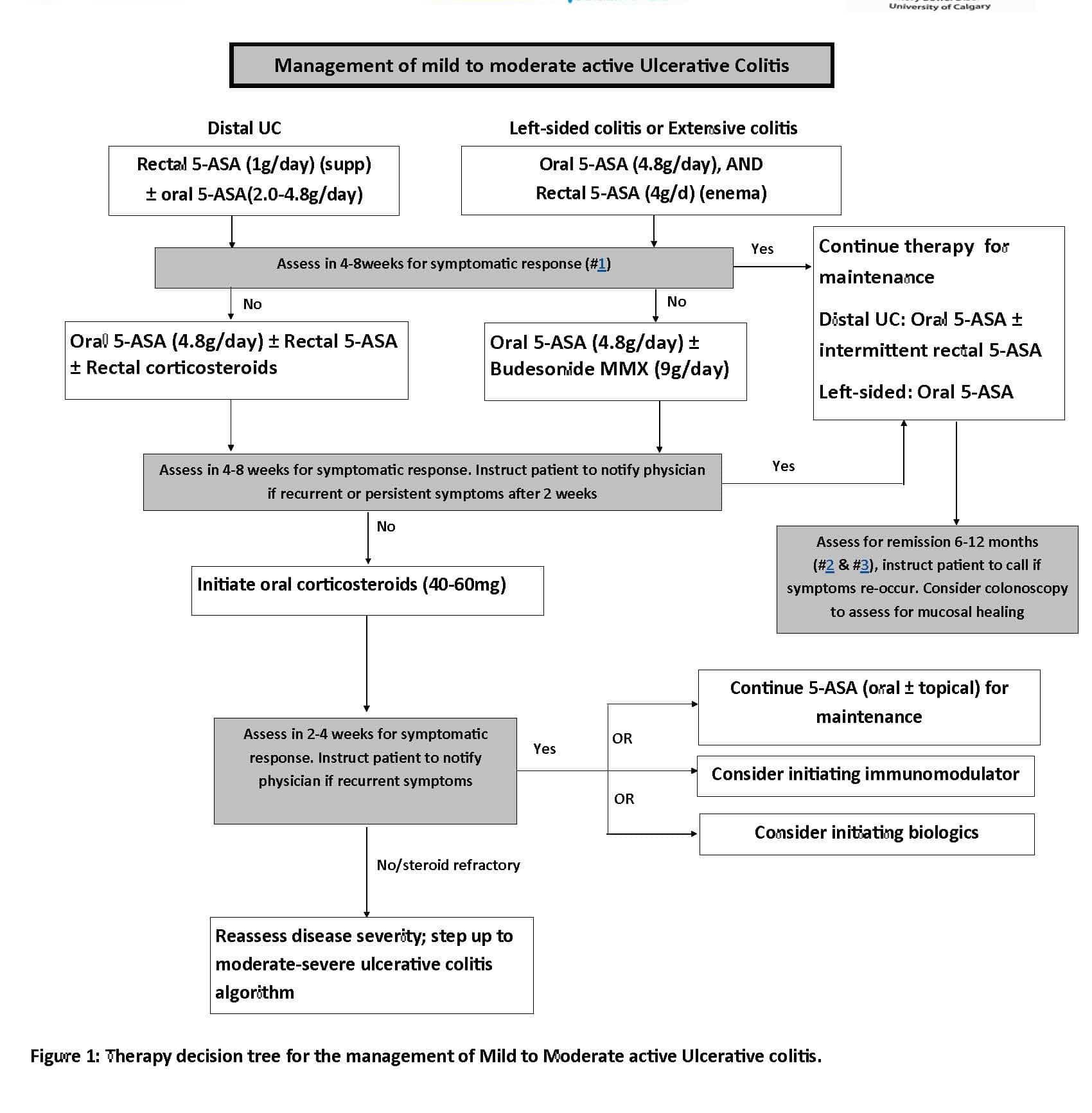
What Are The Treatment Options For A Flare
When you first develop ulcerative colitis it is usual to take medication for a few weeks until symptoms clear. A course of medication is then usually taken each time symptoms flare up. The medicine advised may depend on the severity of the symptoms and the main site of the inflammation in the colon and the rectum .
Topical treatments applied locally by an enema or suppository are widely used for treating ulcerative colitis, particularly aminosalicylate and steroid medicines – see below. They are a treatment option if ulcerative colitis affects only the lower part of the bowel .
Medication options include the following:
Read Also: Where Is Ulcerative Colitis Pain
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Some Foods Worsen Ibd Symptoms
As we start to understand how important the gut microbiome isthe community of bacteria, viruses and fungus that live in our gutwe know that the microbiome or the microbial communities are important to our digestive health and in other areas of our systems, said Dr. Streett.
Its highly individualized as to what foods irritate and make symptoms worse. In inflammatory bowel disease, we note that caffeine may cause anyone to run to the bathroom, said Dr. Gruss. And with somebody with inflammatory bowel disease, that could make symptoms worse.
Also, there is a very common entity called lactose intolerance, which is due to deficiency as one gets older of the lactase enzyme, which is responsible for breaking down milk products in the gut, she added. Now, generally, IBD does not cause lactose intolerance, but if you have lactose intolerance, it can cause diarrhea and make your symptoms of IBD worse.
Additionally, in studies that look at people at more risk for developing IBD in the future, it is people who have eaten a more processed food-heavy diet, said Dr. Streett, noting that IBD doesnt appear to be a food allergy the way celiac disease is an allergy to gluten.
Related Coverage
You May Like: How Can You Get Ulcers In Your Stomach
How Does Ulcerative Colitis Progress
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
Subjective Evaluation Of The Patient Education Program
After the patient education, participants were asked to evaluate their satisfaction with the program. The large majority rated the course very positive 92% were very satisfied with it, 83% reported that the seminar provided support in coping with their IBD, for 84% it provided new knowledge, 84% would take part in such a seminar again, and 95% would recommend it to others.
You May Like: How Does It Feel When You Have An Ulcer
Age Of Onset Is Between 15 And 35
The cause of IBD is one of the great medical mysteries, said Dr. Streett. We know that IBD tends to affect otherwise healthy, younger people about one-quarter to somewhere between a quarter and one-third of people get IBD when theyre under the age of 18, so as children.
But the peak age of onset overall is somewhere between 15 and 35 years old, she said. Once youre diagnosed with IBD, we dont know yet how to turn the process off at a fundamental level. In other words, we dont know how to reverse the underlying process.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Also Check: Stage 1 Vs Stage 2 Pressure Ulcer
Facteurs De Risque De Colite Ulcreuse
Bien que la cause exacte de la colite ulcéreuse soit inconnue, certains facteurs peuvent jouer un rôle. Ceux-ci inclus:
- Histoire de famille: Les patients qui ont un parent proche atteint de colite ulcéreuse courent un risque plus élevé de développer eux-mêmes la maladie.
- Âge: Bien que la colite ulcéreuse puisse survenir à tout âge, elle débute généralement avant l’âge de 30 ans.
- Race et origine ethnique: Les taux de colite ulcéreuse sont les plus élevés chez les patients blancs et/ou d’origine juive ashkénaze.
- Antécédents de tabagisme : Les patients qui fument ou avaient l’habitude de fumer ont des taux plus élevés de colite ulcéreuse que les non-fumeurs.
- Géographie: Selon le Centre national d’information sur la biotechnologie, les taux de colite ulcéreuse sont les plus élevés en Europe du Nord et en Amérique du Nord.
L’alimentation et le stress ne sont pas nécessairement des facteurs de risque de colite ulcéreuse, mais ils peuvent exacerber les symptômes. Le sexe ne semble pas être un facteur de risque les taux de colite ulcéreuse sont similaires chez les hommes et les femmes.
Traitement De La Colite Ulcreuse Dans Le Nj Le Ct Et Le Md
La colite ulcéreuse est une maladie chronique caractérisée par une inflammation du gros intestin. La maladie peut entraîner des symptômes persistants, tels que des douleurs abdominales, qui empêchent les patients de vaquer à leurs activités normales. Chez Regional Cancer Care Associates, les patients atteints de colite ulcéreuse et d’autres maladies chroniques peuvent recevoir services de perfusion pour la délivrance de traitements efficaces. Regional Cancer Care Associates sert des patients dans le New Jersey, le Connecticut, le Maryland et la région de Washington, DC.
Read Also: Chicken Recipes For Ulcerative Colitis
What Goes Into The Body
A healthy intestine typically has a diverse microbiome and a healthy immune response. This balance can change based on genetics, diet, exercise, and what goes into your body.
Unhealthy foods, preservatives, and certain medications can affect the intestines. For example, some antibiotics can disrupt the microbiome in the gut .
While there is no evidence that food causes ulcerative colitis, certain foods can trigger symptoms. There is evidence that a plant-based diet decreases symptoms, while processed foods increase symptoms.
Inflammatory Bowel Disease Community
The Carlino Family Inflammatory Bowel Disease Center is committed to serving its community. Through a variety of events, including educational programs, community lectures, and support groups, our providers are able to give back to the community and help to spread awareness about IBD.
To learn more about upcoming events please e-mail:
You May Like: Low Dose Naltrexone Ulcerative Colitis
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Lifestyle And Home Remedies
Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups.
There’s no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up.
It can be helpful to keep a food diary to keep track of what you’re eating, as well as how you feel. If you discover that some foods are causing your symptoms to flare, you can try eliminating them. Here are some suggestions that may help:
Foods to limit or avoid
– Limit dairy products. Many people with inflammatory bowel disease find that problems such as diarrhea, abdominal pain and gas improve by limiting or eliminating dairy products. You may be lactose intolerant that is, your body can’t digest the milk sugar in dairy foods. Using an enzyme product such as Lactaid may help as well.
– Limit fiber, if it’s a problem food. If you have inflammatory bowel disease, high-fiber foods, such as fresh fruits and vegetables and whole grains, may make your symptoms worse. If raw fruits and vegetables bother you, try steaming, baking or stewing them.
In general, you may have more problems with foods in the cabbage family, such as broccoli and cauliflower, and nuts, seeds, corn and popcorn.
– Avoid other problem foods. Spicy foods, alcohol and caffeine may make your signs and symptoms worse.
Other dietary measures
Stress
Recommended Reading: What Does An Ulcer Feel Like In Your Stomach
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
Follow Up With Your Doctor As Directed:
You may need to return for a colonoscopy or other tests. Write down how often you have a bowel movements and what they look like. Bring this to your follow-up visits. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2022 Information is for End User’s use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Don’t Miss: What Can I Drink With Ulcerative Colitis
Two Novel Jak Inhibitors Show Promise In Ulcerative Colitis
Megan Brooks
Patients with moderate to severe active ulcerative colitis who received induction therapy with either ritlecitinib or brepocitinib showed significant improvement across multiple outcome metrics in a phase 2b “umbrella” study of the two investigational agents.
The study by William J. Sandborn, MD, Division of Gastroenterology, University of California, San Diego, and colleagues was in Clinical Gastroenterology and Hepatology.
Ritlecitinib is a dual inhibitor that selectively inhibits Janus kinase 3 and the TEC family of tyrosine kinases, while brepocitinib is a dual tyrosine kinase 2 and JAK1 inhibitor.
Both agents have demonstrated efficacy and acceptable safety in the treatment of alopecia areata and rheumatoid arthritis and are being evaluated for treating vitiligo, Crohn’s disease, and UC.
The different JAK selectivity profiles of ritlecitinib and brepocitinib , compared with other JAK inhibitors, could further the understanding of the role these pathways play in UC, the investigators note.
How Can I Manage My Ulcerative Colitis
- Do not take NSAID medicines , including aspirin and ibuprofen. NSAIDs can cause flare-ups.
- Eat a variety of healthy foods to keep your colon healthy. Healthy foods include fruit, vegetables, whole-grain breads, low-fat dairy products, beans, lean meat, and fish. Do not eat foods that make your symptoms worse. Your healthcare provider may give you vitamins or minerals to improve your nutrition if you have severe ulcerative colitis.
- Drink liquids as directed. Ask how much liquid to drink each day and which liquids are best for you. For most people, water, juice, and milk are good choices. Do not drink alcohol. This can make your symptoms worse.
- Exercise regularly. Ask about the best exercise plan for you. Any activity is better than none. Even 10 minutes a few times a day would help prevent constipation and help keep your colon healthy.
- Manage stress. Stress may slow healing and cause illness. Learn new ways to relax, such as deep breathing.
You May Like: What To Eat When You Have Gastric Ulcer