Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
When Is A Colectomy Necessary
Modern medical treatments for UC have improved significantly.
According to estimates, 15 in 100 people with UC may require a colectomy 10 years after receiving a diagnosis. However, this number is reducing, as scientists are continually developing better treatments.
The need for surgery varies depending on the severity of the disease and which area of the bowel it affects.
In general, though, 10 years after diagnosis:
- About 19% of people who have extensive colitis may require a colectomy.
- Close to 8% of those with left-sided colitis may need a colectomy.
- Approximately 5% of people with proctitis, which is inflammation of the lining of the rectum, may need a colectomy.
A person may need a colectomy for a number of reasons. These include:
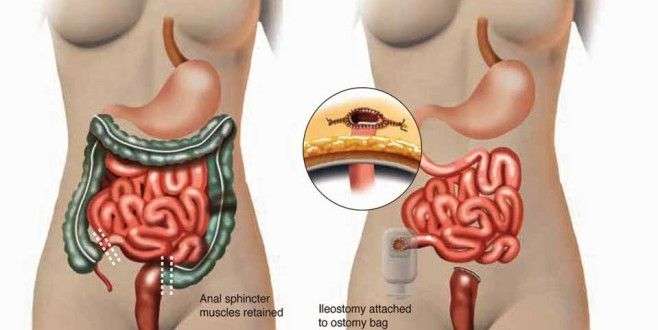
There are two forms of proctocolectomy that surgeons typically perform for people with UC.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
You May Like: What Are The Symptoms Of An Ulcer In Your Stomach
What You Should Know About Proctocolectomy
-
Your colon, rectum, and anus will be removed and an end ileostomy will be created.
-
The ileum will be brought through a hole in your abdominal wall called a stoma, which allows waste to drain out of your body.
-
The stoma will be about the size of a quarter and protrude slightly from your abdomen. A healthy stoma is pinkish in color, and appears moist and shiny.
-
An external ostomy pouching system will attach to the stoma and be worn at all times to collect waste.
-
The typical site for an ileostomy is the lower abdomen to the right of the navel, just below the belt line.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantom rectum and it is completely normal. It does not require any treatment and often subsides over time.
Are There Any Risks To An Ulcerative Colitis Colectomy
The benefits of a colectomy generally outweigh the risks.
But talk to a doctor first about possible risks that have been associated with colectomy for UC, such as:
- infections, particularly at the site of a stoma
If your UC colectomy is planned , talk with a doctor about how you can prepare for your procedure. They may make the following recommendations:
- Gain weight before surgery with a liquid diet if a doctor considers your bodyweight too low.
- Stop smoking, if you do smoke.
- Stop taking blood-thinning medications, herbs, or supplements, and tell the doctor or surgeon in advance about any over-the-counter medications you take and give a full list of prescriptions.
- Clear out your bowels the day before surgery with either a strong laxative or enema .
- Drink plenty of fluids right before your surgery or follow a liquid diet .
- Avoid eating or drinking anything after midnight before your surgery.
Don’t Miss: Best Feed For Ulcer Prone Horses
Does A Colectomy Cure Ulcerative Colitis
- One possible treatment for ulcerative colitis is a colectomy, in which all or part of the colon is removed.
- A colectomy will likely help relieve all colon-related symptoms.
- After a colectomy, people with UC may still have other health problems related to other organs, or they may experience lifestyle changes caused by the surgery.
Ulcerative colitis is a form of inflammatory bowel disease in which the immune system attacks the large intestine . UC causes inflammation and ulcers to form. If the large intestine becomes too damaged or causes severe health problems, your doctor may remove all or part of the colon and rectum in a procedure known as a colectomy, colon resection, or large bowel resection.
There are several types of colectomy procedures. For most people with UC, removing the full large intestine can resolve the majority of their symptoms. Moreover, most people who have a colectomy are able to resume their regular activities and hobbies. Still, undergoing the procedure may also require some lifestyle changes, which can take some getting used to. Understanding the options available and their potential impacts will help you engage in an informed conversation with your health care provider.
How Close Are We To A Cure
Ulcerative colitis is an inflammatory bowel disease that mainly affects the lining of the large intestine . This autoimmune disease has a relapsing-remitting course, which means that periods of flare-ups are followed by periods of remission.
Right now, theres no medical cure for UC. Current medical treatments aim to increase the amount of time between flare-ups and to make flare-ups less severe. This may include a variety of medications or surgeries.
Still, UC research continues to explore other methods to decrease the inflammation associated with this autoimmune disease. Learn more about the new UC treatments that have recently come out on the market, as well as emerging therapies that could be other options in the future.
Two new types of medications for UC have emerged in recent years: biosimilars and Janus kinase inhibitors.
Also Check: How Can You Tell If You Have An Ulcer
Ulcerative Colitis Treatment: Medication
The most common medication option is anti-inflammatory drugs. These can be used orally or topically to reduce inflammation of the colon and rectum.
Treating ulcerative colitis is a highly individualized process. At Johns Hopkins, we tailor your treatment to your specific needs and alter the medication as necessary. Your specific medication regimen will depend largely on the severity of your condition.
Other medications include:
-
Immunosuppressive medications: These drugs slow your immune system to stop the immune response that is causing the colon and rectum to swell.
-
Biologics: Like immunosuppressive medications, biologics target the immune system, but biologics act on specific immune system proteins that encourage inflammation.
Sudden Severe Ulcerative Colitis
This complication is the main cause of emergency surgery in patients with ulcerative colitis. With sudden, severe ulcerative colitis, medications and intravenous steroids, are unable to control the symptoms.
-
Uncontrolled bleeding can occur from deep ulcerations in the colon, though that is rare.
-
Severe, sudden ulcerative colitis can lead to toxic megacolon, a potentially life-threatening complication caused by severe inflammation.
-
Toxic megacolon leads to rapid enlargement of the colon. Symptoms include pain, distension or swelling of the abdomen, fever, rapid heart rate, constipation, and dehydration.
-
Toxic megacolon requires immediate treatment and surgery.
Don’t Miss: How To Treat A Diabetic Ulcer
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
Elective Colorectal Cancer Surgery
Patients with Crohns disease and ulcerative colitis have a higher risk for colorectal cancer than the general population, so elective surgery may be recommended to eliminate that risk.
Colorectal cancer risk factors
-
The risk of CRC increases after living with IBD for 8 to 10 years
-
The risk increases the longer a person lives with IBD
-
The greatest risk is for people with IBD affecting their colon
-
Patients who have a family history of primary sclerosing cholangitis are also at higher risk of developing colorectal cancer
In most cases, colorectal cancer starts as a polyp, or a small lump growing from the wall of the intestine. Polyps typically start out benign but become cancerous over time. But in patients with IBD, abnormal and potentially precancerous tissue, called dysplasia, may lay flat against the wall of the intestine and can even be found in areas of the intestinal wall that appear normal during a colonoscopy.
Read Also: What Causes Mouth Ulcers On Gums
Will I Need Additional Surgeries Or Treatments
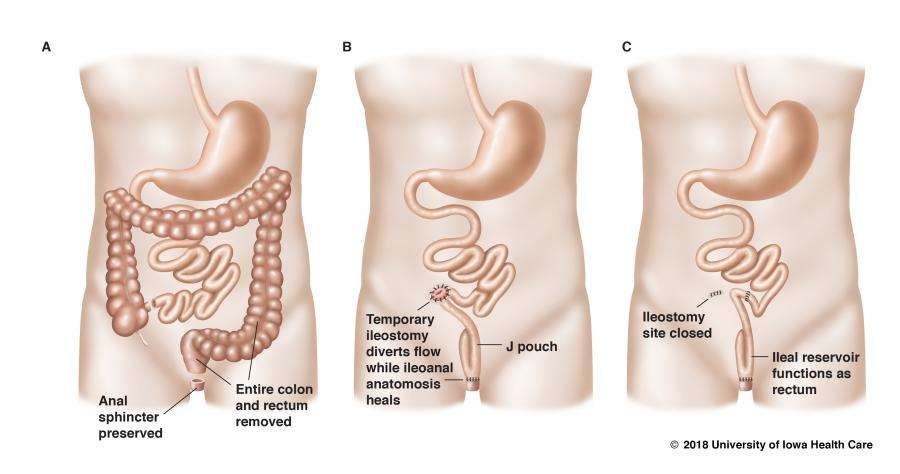
If you have an IPAA, you may have a temporary ostomy in order to give the ileoanal pouch time to heal. Another surgery may be needed about 12 weeks after the first to reconnect your intestines to the pouch.
About one-third of people with UC who get a colectomy have short- or long-term complications. Some of the most frequent are pouchitis and bowel obstructions . These conditions may require additional medical treatments, such as antibiotics or additional surgeries.
Quality Of Life And Satisfaction With Colectomy
The majority of respondents reported that they were somewhat satisfied, satisfied, or very satisfied with colectomy. Most also reported an improvement in their quality of life post-surgery, with 46 % stating that their current quality of life was very improved.
The results of the various survey tools applied are shown in Table . The median IBDQ score was 172 , with clinical remission generally scoring above 170. The mean EQ-5D index score was 0.79 and the mean EQ-5D VAS score was 77.0 .
Recommended Reading: Over The Counter Medication For Ulcerative Colitis
What Are Other Peoples Experiences With Colectomies
The idea of a colectomy can be scary, and its normal to feel emotional before surgery. One MyCrohnsAndColitisTeam member shared, Im really nervous for the moment Im fully awake after surgery as I dont know how my body will physically be feeling, and that scares me. I am basically saying goodbye to my old stomachs appearance and adjusting to a completely new way of living.
Along with its benefits, a colectomy may cause several problems. Some people find the surgery painful. I first had a total colectomy. The second surgery was to build a J-pouch, remove my rectum, and place another ostomy, wrote another member of MyCrohnsAndColitisTeam. It was so painful, and removal of the drain was terrible.
A member shared that surgery led to problems being intimate. I have an ileostomy. It does not bother my husband at all. I, on the other hand, feel a lot less sexy. And I have to be careful of the different positions because it will pop my seal, they wrote.
However, many MyCrohnsAndColitisTeam members have reported that colectomies and ostomies have greatly improved their life. It came to a point where my son was suffering almost every day, said one member. It was no way to live. Now my son has a chance at a healthy life.
A different member shared, I personally feel like I have my life back.
Do I Need An Ulcerative Colitis Colectomy
A colectomy, or large bowel resection, is a type of surgery sometimes used in the treatment of diseases of the large intestine, such as ulcerative colitis .
Surgery for UC isnt as common as it once was. However, its estimated that 1 in 4 people with this type of IBD may require surgery if medications and lifestyle changes arent enough to manage the symptoms of UC.
Learn more about the benefits and risks of a colectomy for surgery as well as what may be involved with this procedure.
A type of inflammatory bowel disease , UC affects the large intestine, which consists of three parts:
- the colon, the main digestive portion of the large intestine
- the rectum, the area between your colon and anus that holds stool
- the anus, the opening at the end of your colon
A colectomy is the surgical removal of your colon or entire large intestine. This procedure is intended to remove severely inflamed or damaged portions of your colon.
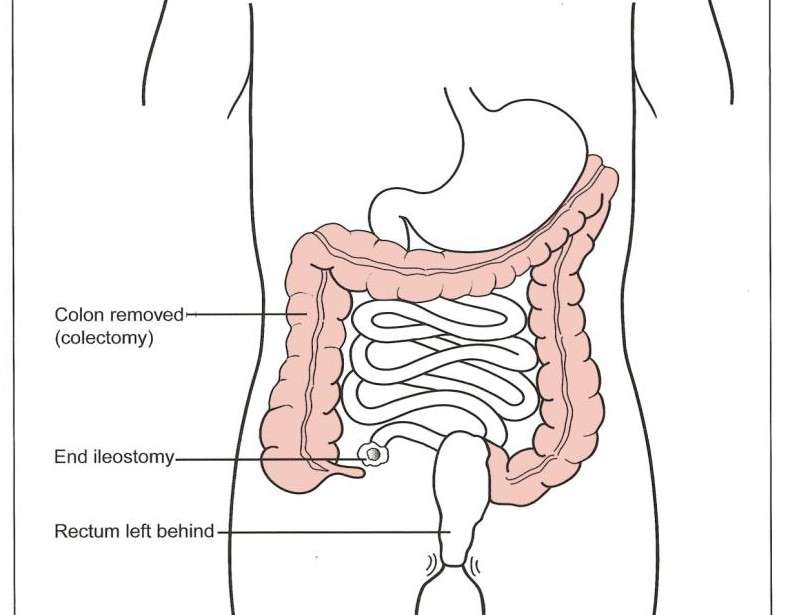
There are several types of colectomy your doctor may consider:
- Proctocolectomy. This involves removal of the colon, rectum, and anus.
- Subtotal colectomy. This involves removal of either the ascending colon or descending colon .
Which type you may require depends on:
- whether you have partial or total UC
- the extent of damage and inflammation to your large intestine
Read Also: How Long Does Ulcerative Colitis Flare Up Last
Open Vs Laparoscopic Colectomy
The terms open and laparoscopic refer to how the colectomy surgery is performed. During an open colectomy, a surgeon makes a large incision in the abdomen to remove the colon tissue. In laparoscopic surgery, the surgeon makes very small cuts and uses flexible tools and cameras to see inside the body and remove the intestine.
Whats Recovery Like From An Ulcerative Colitis Colectomy
You may notice immediate improvements in your UC symptoms following a colectomy.
But as with any major surgery, youll need to take time off to recover and reduce the risk of infections and bleeding. Youll also have pain in your abdomen due to the incisions.
A doctor may recommend a liquid or soft food diet for a few days after your procedure. They may also advise against exercising for at least 6 weeks. You may consider taking a few weeks off work or opt for a work-from-home option, if available.
It may take up to 1 year to fully recover from a proctocolectomy. You may experience multiple bowel movements per day for several months.
Recommended Reading: How To Check A Horse For Ulcers
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Refractory Course And Corticosteroid Resistance
A treatment-refractory course, despite the use of immunosuppressive drugs including biologicals, represents an absolute indication for surgery. Similarly, the patient should be operated on if corticoid dependence is obvious, i.e. the corticoid medication cannot be lowered below the Cushing threshold of 7.5 mg of prednisolone equivalent daily. From this course of the disease, which comprises weeks or months, the intractable fulminant flare must be distinguished which cannot be controlled even by high doses of corticosteroids and requires emergency surgery.
Don’t Miss: How To Cure Gastritis And Ulcers Naturally
Biologics And Beyond In Ibd
This research is part of a new era of IBD care at Cleveland Clinic combining novel medical and surgical therapies with pioneering research. The outcome is IBD care that is setting a high standard, exceeding that of traditional IBD centers of excellence.
Perhaps the most fundamental shift has been the introduction of Cleveland Clinics IBD medical home, which pairs patients with a team of colorectal surgeons, pain specialists, pharmacists, dietitians, social workers, psychologists and others, all led by a gastroenterologist.
While its still early, were seeing that our patients with ulcerative colitis and other inflammatory bowel diseases experience improved quality of life, decreased emergency department visits and hospitalizations, and reduced total cost of care thanks to the medical home model, says Dr. Regueiro, who leads the program. We plan to set the trends for treating these diseases for many years to come.
Total Colectomy Now Proctitisneed Some Help
JonWHut
5 years ago I was diagnosed ith UC completly out of the blue…had no idea I had it! 7 days later I was blue lighted to hospital and had my entire colon removed. Had a Ileostomy until a reversal a year later. I hated the Ileostomy…
Any way now a few years down the line and I’m struggling. Proctitis flare ups, had steriods and on mezasaline, bit it doesn’t seem to be making any difference. Bowel movements around 12+ per day with 3 or so at night.
So I’m knackered, down and tired of it all!
Any words of wisdom??? Diet’s that may help, anything else to try???
Waiting for an appointment with another specialist as the surgeon has passed me on…
Anything please???
Posted 6 years ago
Sorry to hear this John. Have read about aloe Vera drinks don’t know if it will help… I’ve started pro biotics too but not been on them long enough to give a verdict yet. Hope you get sorted soon. Take care & sending healing thoughts your way.
6 years ago
hi, john
I hope you dont mind me asking but I was diagnosed 2 years ago with uc then had a flare up and the removed my whole colon & gave me a illostomy bag which I have had for 3 weeks..so still all alien to me. I am 40 next year with 2 young kids, its bloody hard isnt it, you are going thro so much aswell, I just wondered if you regret having the reversal? everyone says to me oh dont worry the bag wont be forever but I am starting to have doubts obviously I have loads of time to think. what are your views?
Read Also: Best Way To Heal Stomach Ulcers
Ulcerative Colitis Surgical Procedures
The standard surgical procedure to treat ulcerative colitis is a proctocolectomy. This surgery removes both your colon and your rectum .
There are two types of proctocolectomy procedures used to treat ulcerative colitis.
-
Proctocolectomy with ileal pouch-anal anastomosis: Removal of the colon and rectum, and creation of an internal pouch that eliminates the need for a permanent external ostomy.
-
Proctocolectomy with end ileostomy: Removal of the colon, recturm, and anus and creation of an external ostomy.
It can feel overwhelming when you are recommended for one of these surgeries. We can help you understand whats involved with each surgery, and be prepared for life after your proctocolectomy.
How Can I Minimise My Risk Of Getting Bowel Cancer
Its impossible to change some of the things which put you at an increased risk of bowel cancer , but there are some lifestyle factors which are thought to place anyone at a greater risk. Making some healthy lifestyle changes can help to mitigate against these risks. They include:
- Exercising regularly
- Maintaining a healthy weight
- Maintaining a healthy diet
- Avoid alcohol
- Keeping your IBD under control
References
You May Like: Can Ulcerative Colitis Cause Blood In Urine