How To Lower Your Risk For Colitis Flare
Ulcerative colitis is an inflammatory bowel disease that affects your large intestine. More than 750,000 people in North America alone live with this condition. If youre one of them, you know that ulcerative colitis is marked by inflammation and painful ulcers.
Gastroenterologist Eric Ibegbu, MD, and our team at Atlantic Medical Group can diagnose and treat ulcerative colitis with medications and/or surgery.
If youre suffering from painful flare-ups and GI discomfort, we suggest scheduling a visit with us. A colonoscopy can confirm the cause of your symptoms so you can get the right treatment.
In the meantime, you can lower your risk for colitis flare-ups with these tips.
Diet Tips During A Flare
A modified diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, its important to identify and limit these foods.
Your doctor and a dietitian can work with you to find a diet that best manages your symptoms while providing the nutrition you need.
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
Also Check: How Did I Get Ulcerative Colitis
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
“Try to engage in a moderate-intensity exercise like swimming or biking, three or four days per week,” he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Also Check: Can You Drink Coffee With Ulcerative Colitis
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Don’t Miss: Snack Ideas For Ulcerative Colitis
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohn’s disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Southern Cross Medical Library
The purpose of the Southern Cross Medical Library is to provide information of a general nature to help you better understand certain medical conditions. Always seek specific medical advice for treatment appropriate to you. This information is not intended to relate specifically to insurance or healthcare services provided by Southern Cross. For more articles go to the Medical Library index page.
Read Also: Herbal Tea For Ulcerative Colitis
Limit Your Fiber Intake
Fiber contributes to bowel regularity and bowel health, but too much fiber can also trigger UC flare-ups.
Try to stick to foods that have no more than 2 grams of fiber per serving. Low fiber foods include:
- refined carbohydrates such as white rice, white pasta, and white bread
- some cooked fruits
- juice with no pulp
Instead of eating raw vegetables, steam, bake, or roast your vegetables. Cooking vegetables results in some fiber loss.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Don’t Miss: Why Is Ulcerative Colitis Worse At Night
Make Time For Activities That Make You Happy
Tip number three to help you prevent an ulcerative colitis flare-up: Always make time for things that make you happy. For me, its dancing. I have been taking dance classes since my pre-school years and continues to do so to this day. Its wonderful exercise, I have met amazing friends through this hobby, and it is also my favourite form of exercise. When I am in the dance studio, I forget about everything else in the world and focus on being in the present. So, whether it be dance, a sport that you love, or something as beautiful as painting, make time to feed your hobbies with your time and hopefully you will feel more fulfilled and less stressed!
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
Don’t Miss: How Long Does Prednisolone Take To Work For Ulcerative Colitis
Tips On How To Stop A Flare
Learning how to stop, manage, or decrease symptoms during a flare-up can help improve the quality of life of people with UC.
Although managing flare-ups is important, knowing what can trigger a flare-up can help stop one from happening in the first place.
Some of the following strategies may be helpful to implement.
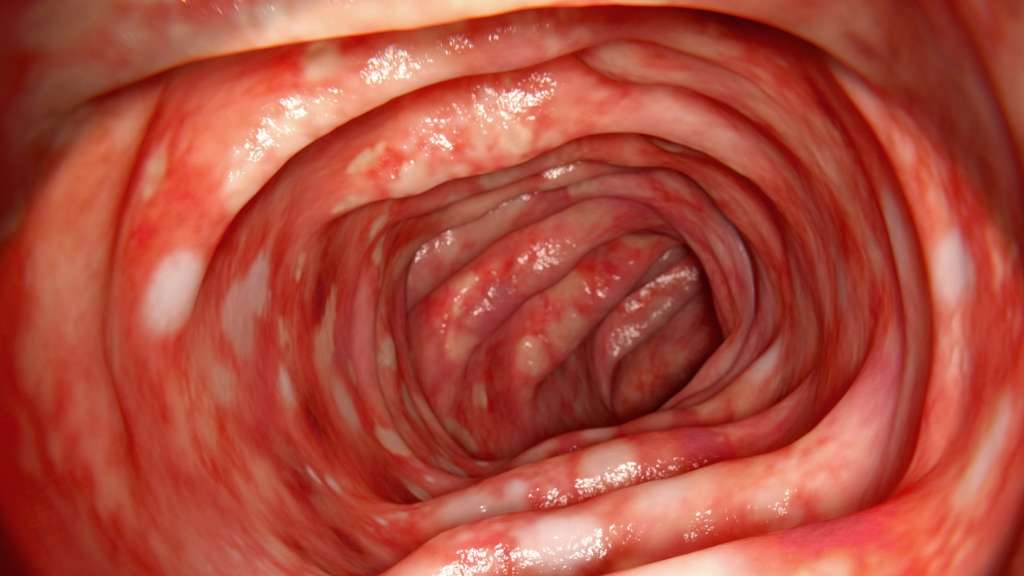
Layers Of The Bowel Wall
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, theres inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. More mucus may be produced by the inner layer of the bowel wall. Ulcers develop on the inner layer as the condition gets worse, but they can also go as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When youre having symptoms, its known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section Types of Colitis.
The most common symptoms are:
Andy
Living with Colitis
Also Check: Gastric Ulcer Treatment In Horses
Prevent An Ulcerative Colitis Flare By Following A Diet That Works For You
To prevent flare-ups, I think that all the stress management techniques combined with DIET make a huge difference for me. My amazing GI has talked to me about a diet eliminating as much sugar and refined carbs as possible. I will definitely talk more in-depth about diet and a breakdown of my diet in the future, but here are some diet based tips to help you prevent an ulcerative colitis flare
Assessing Response To Medical Treatment
The FBC, U+Es, albumin, CRP and stool frequency should be checked on a daily basis. The AXR should be repeated daily if there is severe extensive colitis, dilatation on the previous AXR, fever, tachycardia or abdominal tenderness otherwise repeating it every other day will suffice. In patients without evidence of toxic dilatation and impending perforation, a decision to continue with standard therapy, to commence rescue therapy, or to proceed to a colectomy should be made by the consultant gastroenterologist in conjunction with a colorectal surgeon at the end of 72 hours of intravenous hydrocortisone. In patients who respond to standard therapy, intravenous hydrocortisone should be continued for a minimum of five days before switching to prednisolone 40 mg daily, which can be tapered by 5 mg every week provided the patient remains in remission. Furthermore, topical and/or oral 5-ASA therapy can be restarted or commenced once the patient is improving.
Recommended Reading: How To Lose Weight With Stomach Ulcers
How Common Is It
If you have UC and experiencing diarrhea, youre not alone.
According to the Crohns & Colitis Foundation of America, about 907,000 people are currently living with UC in the United States. Among them:
- 48 percent are in remission
- 30 percent have mild disease activity
- 20 percent have moderate disease activity
- 1 to 2 percent have severe disease
During a flare-up, a person with UC may experience more frequent bowel movements. They may find their stools to be loose and very watery.
According to Crohns and Colitis Canada, people who have extensive inflammation of the colon are more likely to have:
- persistent diarrhea and urgency
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Also Check: Dakin’s Solution For Pressure Ulcers
Treating Stress Hormone Imbalances
The first step? Treating Sherries stress-response system. The hypothalamic-pituitary-adrenal axis regulates our circadian rhythm and our stress response. Chronic stress can really throw the HPA axis out of balance, which leads to hormone imbalances. It can cause the adrenal glands to pump out too much of the stress hormone cortisol. Some people call this adrenal fatigue, but its really a problem with the entire HPA axis.
As Sherrie tapered off the prednisone, I gave her a higher than normal dose of dehydroepiandrosterone , a hormone produced by the adrenal glands. Because she had been under stress, her adrenal glands were likely worn out and werent making enough DHEA.
In fact, every ulcerative colitis patient Ive treated has had HPA axis dysregulation. So I typically always address this in my UC patients.
And guess what? Her ulcerative colitis flare regressed for the first time in two years. She now had only minimal rectal bleeding and not every day.
What To Do During An Ulcerative Colitis Flare To Minimize Symptoms

Youll inevitably experience another UC flare-up at some point, despite your best prevention efforts. When this happens, there are a few ways youll need to tweak your normal routine to minimize the severity of your symptoms and get back into remission ASAP. Even some of your typically healthy habits like loading up on veggies may be a no-go. Here are a few natural remedies that may help:
Also Check: Side Effects Of Bleeding Ulcer
Failure To Have A Gastroenterology Specialist On Your Side
Your primary care physician can only do so much for you. In order to adequately manage and treat your Crohns or ulcerative colitis, you will need to see a specialist for regularevaluation. In fact, you should have a whole team of doctors working for you, from surgeons to radiologists to nutritionists however, your gastroenterologist should be your main point of contact when it comes to your condition.
We treat patients with Crohns and ulcerative colitis as well as a variety of other gastrointestinal diseases, including colon cancer, hepatitis, biliary diseases, esophageal disorders, and peptic ulcer disease. Our specialists can offer you more tips on how to best manage your condition, and work with you one-on- one to develop a workable treatment plan.
Call for an appointment with a gastroenterology specialist today.
Please note, the information provided throughout this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and video, on or available through this website is for general information purposes only. If you are experiencing related symptoms, please visit your doctor or call 9-1-1 in an emergency.
GET OUR FREE NEWSLETTER
Work With Your Doctor
You’ll need to see your UC doctor regularly. It may be every 6 months while you’re in remission. You’ll have routine procedures like colonoscopies and bloodwork to check on your UC.
If you’re having a flare-up, make sure to check in with your doctor. UC isn’t the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Can’t keep liquids down
When you have a flare, you can ask your doctor questions like these:
- Is UC causing my symptoms, or could they be due to another condition?
- Do I need to take any tests? If so, how often will I need to get them?
- Will you need to change the dose or type of my medication?
- If I need to take a new medication, what side effects could it cause?
- Should I make any lifestyle changes?
- When should I come back for another appointment?
Also Check: Stomach Ulcer And Back Pain
Avoid Sugar To Help Curb Inflammation
Refined sugar is not your friend if you have UC, according to Eleanor Baker, M.S., a registered dietician in Melbourne, FL. Diets high in added sugar contribute to a spike in blood glucose that can result in a short-term increase in energy, and then a drop in energy levels as the body strives to keep up with the excessive intake of sugar. Ms. Baker recommends eating foods with naturally occurring sugars and whole grains to provide you with a steady release of energy without the undesirable crash later. For a healthy treat try these low-sugar dessert recipes for people with UC.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
You May Like: How Can You Get Ulcerative Colitis
Manage Symptoms Of A Flare
While you work with your doctor to get your flare under control, you can take steps to ease certain symptoms:
Pain. Experts say acetaminophen is the safest way to get pain relief. If it doesn’t help you enough when you have pain in your stomach or another body part, ask your doctor what other meds they’d recommend.
Sometimes UC is linked to pain beyond your gut. If you get eye pain or if your eyes feel sensitive to light, see a doctor called an ophthalmologist as soon as possible. Some people living with UC develop eye problems that need fast treatment.
If you have leg pain or pain in another large joint, it might be due to arthritis linked to your UC. Your doctor may tell you to rest the joint that hurts. They may also recommend that you occasionally soothe it with moist heat, like from a warm bath or heated wash cloth. You could also ask the doctor if physical therapy might help.
Irritated bottom. Keep it clean with moist wipes and protect it with diaper cream. You could also soak in a saltwater bath.
Diarrhea. Ask your doctor if you can take an anti-diarrheal drug, like bismuth subsalicylate or loperamide .
Canker sores. Medicated mouthwash may ease the irritation that these small mouth ulcers bring on. A balanced diet and a multivitamin or mineral supplement may help, too. Talk to your doctor before you try any new supplement.