Will Ulcerative Colitis Affect My Stool
Changes in bowel movements are one of the key markers of Ulcerative Colitis. UC stool shape, color, and smell can be quite different than your average bowel movement. If you have Ulcerative Colitis, your immune system essentially attacks healthy cells in your digestive tract, which causes inflammation in your colon and rectum. Below are some key indicators that you may have Ulcerative Colitis based on your stool.
- Color: You might notice bright red, maroon or black color indicating the presence of blood. You may also notice more mucus in the stool than normal.
- Odor: The odor of the stool may be increasingly foul compared to the typical smell.
- Texture: Presence of UC typically causes loose, watery stools. In reference to the Bristol stool chart, UC stool texture will most likely resemble types 5 through 7.
- Frequency: Inflammation can cause increased motility and frequency of bowel movements. Many people experience frequent urgency and diarrhea.
- Effort: People with UC may experience burning or painful stools.
Always consult your primary care doctor. They can refer you to a local GI specialist if needed
If diagnosed, you may want to seek a specialist for your specific disease in your area
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.
Spinach Artichoke Yogurt Dip
This easy-to-make dip will help you sneak in your daily veggie servings. Artichokes are a low fiber food thats generally safe for people with ulcerative colitis. Theyre also a prebiotic. That means they feed the good bacteria in the gut and may support colonic health.
Combine one can of artichoke hearts and a package of chopped spinach with low fat yogurt and shredded cheddar cheese.
Pour the mixture into a casserole dish. Then bake at 350°F for 20 to 25 minutes. Serve with sliced carrots and cucumbers for dipping.
Don’t Miss: Best Diet For Peptic Ulcer
Greek Yogurt Topped With Cantaloupe Or Honeydew Melon
Yogurt is a good source of probiotics. These friendly bacteria help your gut run more smoothly. Make sure the yogurt you buy says live and active cultures on the label. That means it contains probiotics.
Studies suggest that female patients with ulcerative colitis dont get enough calcium. Calcium deficiency increases the risk of osteoporosis. Yogurt is rich in the mineral, which helps keep your bones strong.
If lactose stirs up your ulcerative colitis symptoms, choose one of the many lactose-free yogurt varieties available.
Top tart yogurt with sliced melon. This ulcerative colitis-friendly food introduces a hint of sweetness without adding too much sugar.
Eating With A Stricture

If you have a stricture , you may need to change what you eat to help prevent the intestine getting blocked.You might be advised to avoid foods that could block the intestine, such as:
If you have a severe stricture, you may only be able to eat very soft or liquid foods.Its important to speak to a dietitian to make sure youre eating a healthy, balanced diet. In some cases, they may recommend a vitamin and mineral supplement.
You May Like: How To Remove Ulcers In Stomach
Ulcerative Colitis Diet Plans
A handy tip is to keep a food journal to help identify the foods that are your triggers. Essentially those foods that bring about an attack. Your food journal should allow you to make decisions about which foods you should or should not eat. Some helpful information to include in your journal:
- The foods you have eaten
- The date and time
What To Eat During Flare
Low-fiber foods are easiest to digest and are less irritating to the gut, especially with symptoms like abdominal pain or diarrhea. Choose:
- Grains/starches: White foods, instead of wheat or whole-grain, and those with less than 2 grams of fiber per serving
- Cooked vegetables: Well-cooked vegetables such as green beans, carrots, mashed potatoes without skin, steamed asparagus tips and pureed squash.Use fresh or frozen.
- Canned or soft fruits: Peeled apples, ripe bananas, cantaloupe, honeydew, watermelon, and canned fruit in fruit juice or light syrup
Be sure to eat enough protein — Inflammation causes increased protein needs. Choose:
- Tender, well-cooked meats: Poultry, salmon or other fish, lean beef and pork prepared without added fat
- Deli meats: Low-sodium and low-fat varieties
- Eggs: Well-cooked
- Smooth nut and seed butters: Peanut, almond or sunflower seed
Drink plenty of fluids — Aim for eight cups a day, and consider using oral rehydration beverages as needed. Try to limit caffeinated, sugar drinks and beverages made with sugar substitutes.
Limit added fats and oils — Focus on oils instead of solid fats, and limit intake to less than eight teaspoons per day.
Consume adequate calcium, vitamin D, probiotics, and prebiotics — Sources include:
Recommended Reading: Signs A Horse Has Ulcers
Dietary Advice For Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis?
Ulcerative Colitis is a form of Inflammatory Bowel Disease . IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
Diet is not a cause of UC however diet can help to relieve symptoms such as diarrhoea during a flare up and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the Eatwell Guide.
What foods are beneficial for UC during a flare up?
Soluble FibreDietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
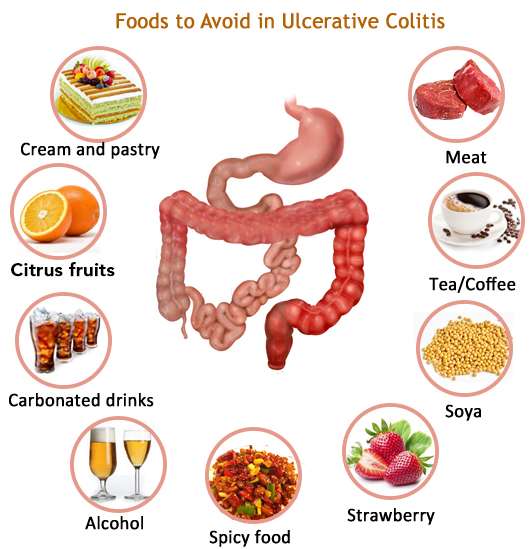
What foods may worsen UC during a flare up?
Dairy foods
Spicy foods and fatty foods
Cereal With Low Fat Milk
High fiber bran and wheat cereals could set off a bout of diarrhea and other ulcerative colitis symptoms. But you dont have to cross cereal off the snack list. Its still a good source of vitamins and minerals.
You do want to choose your cereal wisely, though. Lower fiber options like corn flakes and rice puffs are easier on your gut.
Yogurt is often easier on your gut if lactose causes ulcerative colitis symptoms. Or opt for a dairy alternative like soy or rice milk. Top your bowl of cereal with sliced bananas to ramp up the nutrition.
You May Like: 8 Foods To Eat During An Ulcerative Colitis Flare
New Guidelines Are A Good Place To Start
All patients with IBD should work with their doctor or a nutritionist, who will conduct a nutritional assessment to check for malnutrition and provide advice to correct deficiencies if they are present.
However, the recent guidelines are an excellent starting point for discussions between patients and their doctors about whether specific dietary changes might be helpful in reducing symptoms and risk of relapse of IBD.
About the Author
John Garber, MD, Contributor
Diet For People With A Stoma
Most people with a stoma have an acceptable output and do not need to modify their diet. Generally, the Australian Guide to Healthy Eating is recommended. One of the roles of the large intestine is to reabsorb water, so ensuring good hydration by having plenty of fluid is important. You may benefit from further consultation with a specialist dietitian if your stoma output is too much, too watery, or too gassy.
Please refer to the Complications with IBD page for further information.
Also Check: Ulcerative Colitis Lower Back Pain
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Tips For Meal Prepping

Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
Don’t Miss: Cost Of Biologics For Ulcerative Colitis
Faq: Dietary Management Of Ibd
Information regarding dietary treatments for IBD is often confusing. Many people receive information telling them to avoid entire food groups or specific foods. However, there is no need to avoid foods unless they worsen your symptoms. It is best to restrict as few foods as possible to increase the chances that you are getting a balanced, nutritious diet. This is important for maintaining the function of your digestive tract and your overall health.
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Don’t Miss: How Do Biologics Work For Ulcerative Colitis
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Recommended Reading: What To Drink With Stomach Ulcer
Nutrients Intake Of Patients According To The Disease Status
The nutrients intake of patients was compared against the standard recommendation intake values according to the disease state as shown in Table 2. The dietary intake of patients in the inactive state was higher than the active state , however, both groups of patients did not meet the standard recommendation for energy, protein, calcium, iron, folate, zinc, vitamin D, vitamin B12, and vitamin E. In particular, less than 10% of patients in the active disease met the recommendation for energy, protein, fat, calcium, iron, folate, zinc, vitamin D, vitamin B12, and vitamin E in comparison to the RNI for Malaysia 2017 as shown in Fig. 2.
You May Like: Ulcerative Colitis Blood In Urine
How Would Observing These Guidelines Help
The recommendations were developed with the aim of reducing symptoms and inflammation. The ways in which altering the intake of particular foods may trigger or reduce inflammation are quite diverse, and the mechanisms are better understood for certain foods than others.
For example, fruits and vegetables are generally higher in fiber, which is fermented by bacterial enzymes within the colon. This fermentation produces short-chain fatty acids that provide beneficial effects to the cells lining the colon. Patients with active IBD have been observed to have decreased SCFAs, so increasing the intake of plant-based fiber may work, in part, by boosting the production of SCFAs.
However, it is important to note disease-specific considerations that might be relevant to your particular situation. For example, about one-third of Crohns disease patients will develop an area of intestinal narrowing, called a stricture, within the first 10 years of diagnosis. Insoluble fiber can worsen symptoms and, in some cases, lead to intestinal blockage if a stricture is present. So, while increasing consumption of fruits and vegetable is generally beneficial for Crohns disease, patients with a stricture should limit their intake of insoluble fiber.
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Read Also: How To Treat Diabetic Ulcer On Toe
Ulcerative Colitis Diet: Foods To Eat And Foods To Avoid
- Keeping a food journal can help you identify foods that trigger ulcerative colitis symptoms.
- Avoiding common trigger foods may help manage symptoms during UC flares.
- Knowing which foods are most nutritious for those with UC and how to safely prepare them can help you eat healthier.
- Working with a registered dietitian can help you get the most nutrients out of the foods you can safely eat.
Ulcerative colitis is an autoimmune condition caused when the immune system attacks the tissues of the digestive tract, specifically the large intestine and rectum. Along with Crohns disease, ulcerative colitis is a type of inflammatory bowel disease. IBD inflammation leads to gastrointestinal symptoms, such as diarrhea, bloating, and cramping, as well as problems with digestion and absorption of nutrients.
No specific foods cause ulcerative colitis, and there is no specific diet that has been proven to cure it. However, each person with UC finds that certain foods can trigger or worsen symptoms, while other foods can be digested safely and comfortably. The foods on each list vary by individual. As one MyCrohnsAndColitisTeam member put it, This disease is not one-size-fits-all, so you will have to experiment to see what works for you and what does not.
The list of foods to avoid and foods to eat with ulcerative colitis may also change depending on whether youre currently experiencing a disease flare or remission .
What You Should Know About Strictureplasty
Any surgery is concerning, but learning about the procedure can lessen your concerns and give you information to discuss with your healthcare team.
-
Strictureplasty is a generally safe procedure. It is most effective in the lower sections of the small intestine, called the ileum and the jejunum.
-
Strictureplasty is less effective in the upper section of the small intestine, called the duodenum.
-
Strictureplasty avoids the need to remove a section of your small intestine. It is preferred when possible, because removing portions of your small intestine cause sometimes cause other complications, including a condition called short bowel syndrome which occurs when large sections of the small intestine are removed due to surgery and the body is unable to absorb adequate amounts of nutrients and water.
During the procedure
-
Your surgeon will make cuts lengthwise along the narrowed areas of your intestine, then sew up the intestine crosswise.
-
This type of incision and repair shortens and widens the affected part of your bowel, allowing food to pass through.
-
Your surgeon may repair several strictures during the same surgery.
You May Like: Interventions To Prevent Pressure Ulcers