What About Vitamins And Minerals
It is a good idea for all people with IBD to take a standard multivitamin every day. People with IBD who are doing well do not need any extra vitamins or minerals. If you have Crohn’s disease is in the ileum or the ileum has been removed you may need to take B12, calcium, or vitamin D. You may need iron supplements if you have blood loss during inflammation or reduced iron absorption as a result of inflammation. Diarrhea or vomiting can cause loss of potassium and magnesium. If you are lactose intolerant and avoid dairy products, this can lead to low calcium. Ask your doctor if you need to be tested for any of the above.
Is Ulcerative Colitis And Autoimmune Condition
We are frequently asked whether Ulcerative Colitis it is an autoimmune condition. The short answer is yes, but its most important to understand what that means for your treatment plan.
With Ulcerative Colitis, the body recognizes harmless gut bacteria as an enemy and attacks the tissues in the colon. In a typical immune response, the body will send white blood cells to the area of illness or infection to help protect the body. After the body has combated the illness or infection, the inflammation will resolve.
However, in a colon affected by UC, the body continues to send white blood cells to the inner layer of the large intestine, which accumulate and continue to attack. This process causes a buildup of inflammation and can lead to sores, or ulcers, in the affected area. Because UC is recognized as an autoimmune condition, the treatment methods generally target the immune response within your body.
Medical Treatments for Ulcerative Colitis include:
Read our full discussion of Ulcerative Colitis autoimmune treatment options here.
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
You May Like: Gastric Ulcer Treatment At Home
It Can Be Challenging To Differentiate Between Crohns And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Recommended Reading: Can You Develop Ulcerative Colitis Later In Life
My Life: Managing Ulcerative Colitis With Drugs
At the time, I was receiving Remicade infusions for the managing of the Ulcerative Colitis condition that I had been dealing with for over 10 years. Ulcerative Colitis is a type of inflammatory bowel disease characterized by abdominal cramping and bloody diarrhea. Remicade is not a treatment it only manages the symptoms therefore, it does not address the root problem.
To give you some history, I had been dealing with digestive issues since 1999 when I was diagnosed with Ulcerative Colitis. To manage and hide symptoms throughout those years, I went through the typical pyramid of conventional medications, beginning with Asacol, Colazol and Prednisone. Finally, Remicade was prescribed in 2006 when a major flare-up landed me in the ER. In the hospital, I was first given the highest dosage of IV Prednisone possible in attempts to stop the bleeding and cramping. When that wasnt successful, they told me the only other option besides surgery was Remicade, an intravenous drug that suppresses the immune system. It had just recently been approved for Ulcerative Colitis when previously it was only approved for Crohns Disease and Rheumatoid Arthritis.
Remicade managed my symptoms, bleeding, and abdominal pain. However, I soon realized that I wanted out of the managing symptoms cycle. You may be wondering why would I want to risk flaring, risk spending more time in a hospital, risk more pain and bleeding, and risk facing many health uncertainties.
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.
Also Check: Foods To Avoid If You Have A Stomach Ulcer
Foods To Fight Ulcerative Colitis
- Salmon The essential fatty acids in salmon will help counterbalance an inflammation flare-up.
- Cultured Yogurt Cultured yogurt contains probiotics, beneficial bacteria necessary for maintaining a healthy gastrointestinal tract.
- Squash The antioxidants Beta-carotene, vitamin A, and vitamin C in squash will help repair damage done by inflammation.
- Egg Whites Rich in B vitamins and a great source of protein, eggs whites are often well tolerated by people with ulcerative colitis and may help reduce inflammation.
- Honeydew Melon Honeydew melon will help soothe the lining of your colon.
- Avocados Studies have found that 85% of people with inflammatory bowel disease are malnourished. Avocados are a great source of calories, healthy fat, and protein. Theyre also easily digested by the body.
- Instant Oatmeal Instant oatmeal is more processed than steel cut oatmeal, making it easier to digest for people who have ulcerative colitis.
- Turkey For a healthy intake of protein, try turkey and other lean meats like skinless poultry and lean pork loin. The unsaturated fat in other meats may trigger a symptom flare-up.
Common Supplements Recommended For Ibd Patients
Your healthcare provider may recommend that you take vitamin or mineral supplements, especially if you are experiencing nutritional deficiencies. We can help you learn about supplements that are commonly recommended for IBD patients.
This information can help you learn which vitamins and minerals are important to maintain your nutrition, along with the various foods you may want to try as part of your IBD-friendly diet.
Your body is unique. What works for one patient, will not work for everyone. Check with your healthcare providers before starting any supplements, as you will need proper dosing.
Also Check: What Does Asacol Do For Ulcerative Colitis
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
What To Eat During Remission
Increase fiber and reintroduce whole grains Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
You May Like: Can You Feel A Stomach Ulcer
You May Like: Symptoms Of Crohn’s Disease And Ulcerative Colitis
Gut Microbiota And Ibd
Any alteration of the bowel eubiosis or in the composition of the microbiota is defined as dysbiosis. IBD is associated with alterations in the composition of the intestinal microbiota, characterised by decreased diversity, reduced proportions of Firmicutes, and increased proportions of Proteobacteria and Actinobacteria . Some of the bacterial species with pro-inflammatory effect are enriched in patients with IBD , while anti-inflammatory species are largely reduced in IBD . For example, patients with active IBD have been shown to have a lower abundance of Clostridium coccoides, Clostridium leptum, Faecalibacterium prausnitzii and Bifidobacterium . Prospective studies investigating the role of microbiome changes on the disease course have been scarce. A Dutch study based on 10 CD and nine UC patients reported patient-specific shifts in the microbial composition, but could not demonstrate general changes in the microbial composition or diversity . A Spanish study followed up 18 UC patients over the course of one year in those who remained in remission Faecalibacterium prausnitzii increased steadily, while in those who relapsed it did not .
Healing Ulcerative Colitis With Diet The Principal Guide

Healing ulcerative colitis naturally with diet is possible.
At least it was for me.
I was diagnosed with severe ulcerative colitis in 2004. It nearly killed me several times. It was that bad.
But that was many years ago.
As I write this in 2021, Im quite healthy.
Its been many years since Ive had a flare-up. I dont worry about them anymore.
My stools are well-formed and theres no blood.
I dont use any medication other than medical marijuana.
Ive been going along for years like this with no problems.
It hasnt been easy and its a lot more than diet. But without a solid diet foundation, little else matters with regard to managing and healing ulcerative colitis .
Also Check: How To Prevent Decubitus Ulcers
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Read Also: What Should I Eat With Ulcerative Colitis
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohn’s disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Also Check: Is Avocado Good For Ulcerative Colitis
Choosing The Right Diet For Ulcerative Colitis
Because each body is different, there isnt a one-size-fits-all diet for UC. Work closely with a registered dietitian to design a diet that works for you, Diekman advises. Its also good to keep track of what you eat in a food journal.This makes it easier to pinpoint which ingredients trigger your symptoms.
Additional reporting by Kaitlin Sullivan
Sign Up For Our Newsletter For Ibd Recipes & Diet Tips
The information listed on the website is only for informational purposes.
This is the official site for the IBD-AID . It is moderated by trained personnel who represent Umass Medical School Center for Applied Nutrition. The diet is an evolving pattern of foods, expanding as we learn more from our research. We welcome patients and professionals alike, to support each other in applying this diet to each individuals needs. The core principles of the diet must remain evidence-based but may be adapted to fit a diverse population from cultural and geographic perspectives.
This is an official Page of the UMass Chan Medical School
Center for Applied Nutrition 55 Lake Avenue North Worcester, Massachusetts 01655
Questions or Comments? E-mail: Phone: 508-856-5195
Read Also: What To Take For Stomach Ulcer Pain
Think About Vitamin Supplements
Crohns disease often limits the amount of vitamins and minerals your body can absorb from foods. Vitamin B12 is one common deficiency. According to Kennedy, this can be further depleted for those following a semi-vegetarian, vegetarian, or vegan diet, since meat, poultry, and fish are three main sources of this vitamin. If youre transitioning to a plant-based diet, be aware of this deficiency and talk to your doctor about supplementing.
Donât Miss: How To Soothe Mouth Ulcers
The Best Diet For Ulcerative Colitis

Most experts say that people with UC should simply try to eat a well-balanced diet whenever possible. This should include a variety of foods:
- Lean meat, fish, and poultry
- Low-fat dairy products
- Bread, cereal, and whole grains
- Fruits and vegetables
- Healthy fats such as vegetable oils
Keep a food diary to help you figure out which foods cause problems for you and whether or not you’re getting enough nutrients.
If you lose weight because of your ulcerative colitis, try to eat five or six small meals and snacks during the day instead of two or three large meals.
When you have chronic diarrhea, drink plenty of water or other fluids to stay hydrated.
A dietitian can plan a diet that meets your calorie and nutrient needs. Before you take any dietary supplements, talk to your doctor or dietitian. Find out how to make a diet plan for ulcerative colitis.
You May Like: What Foods Help Stomach Ulcers
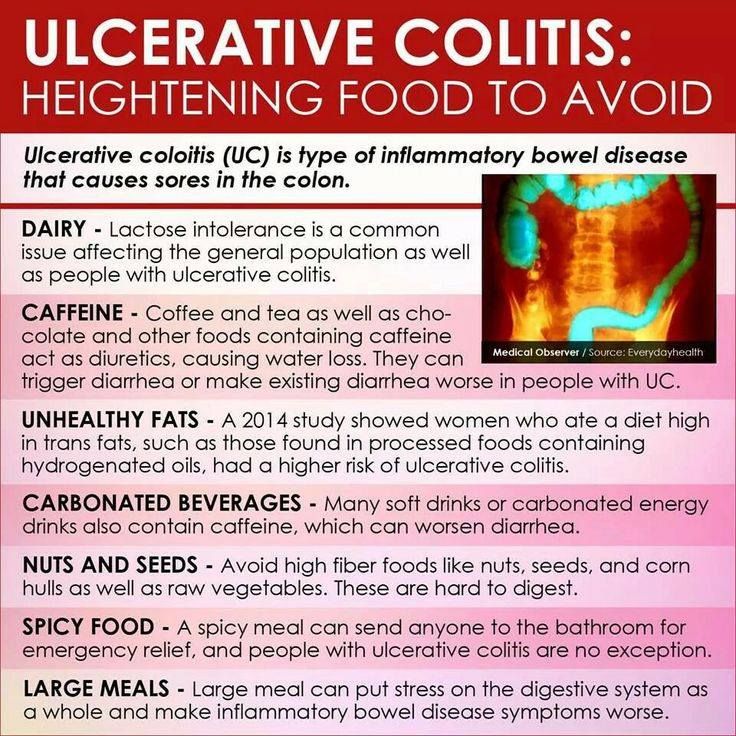
What Foods Should I Avoid
Certain foods can exacerbate UC flares, but everyone has different trigger foods. For some, it might be a juicy burger and for others, it could be their morning latte.
In general, inflammatory foods, like fast food, processed food, alcohol, and sugary drinks contribute to the development of flares, says Dr. Singh. Freuman adds that saturated fat, specifically, can be an issue for certain people. Foods that contain significant amounts of saturated fat include:
- Whole-milk dairy, such as cheese, cream, butter, and full-fat yogurt
Lactose is the sugar present in milk and dairy products, and lactase is the enzyme people need to break down those sugars during digestion. If someone is lactose-intolerant, it means they dont produce enough lactase to break down the sugars, which can cause cramps, bloating, diarrhea, and gas.
To complicate matters, UC is sometimes coupled with lactose intolerance. But lactose intolerant dairy lovers, take heart: Its often possible to still consume dairy with lower lactose content, like cottage cheese and yogurt. Because these products contain live cultures that produce their own lactase, your body doesnt have to do all the work to break down lactose5.
Thats a win-win, since dairy foods provide important nutrients, like calcium and vitamin D, to your diet. In fact, avoiding them completely is not recommended unless 100% necessary.