Check The Skin For Signs Of Developing Pressure Sores Often
The skin should be checked frequently for the signs of developing pressure sores. A pressure sore may develop in less than a few hours.
For example, have you ever experienced increased soreness and redness on your buttocks while driving for more than an hour or two? If so, you developed a Stage I pressure sore, but your ability to move allowed you to recognize the pain and adjust your position to prevent it from progressing.
For some seniors, you must be the one to check and recognize the signs of a pressure sores development when performing perineal care, providing showers or performing other assessments of skin integrity. All such checks should be documented as well.
Symptoms Of Pressure Sores
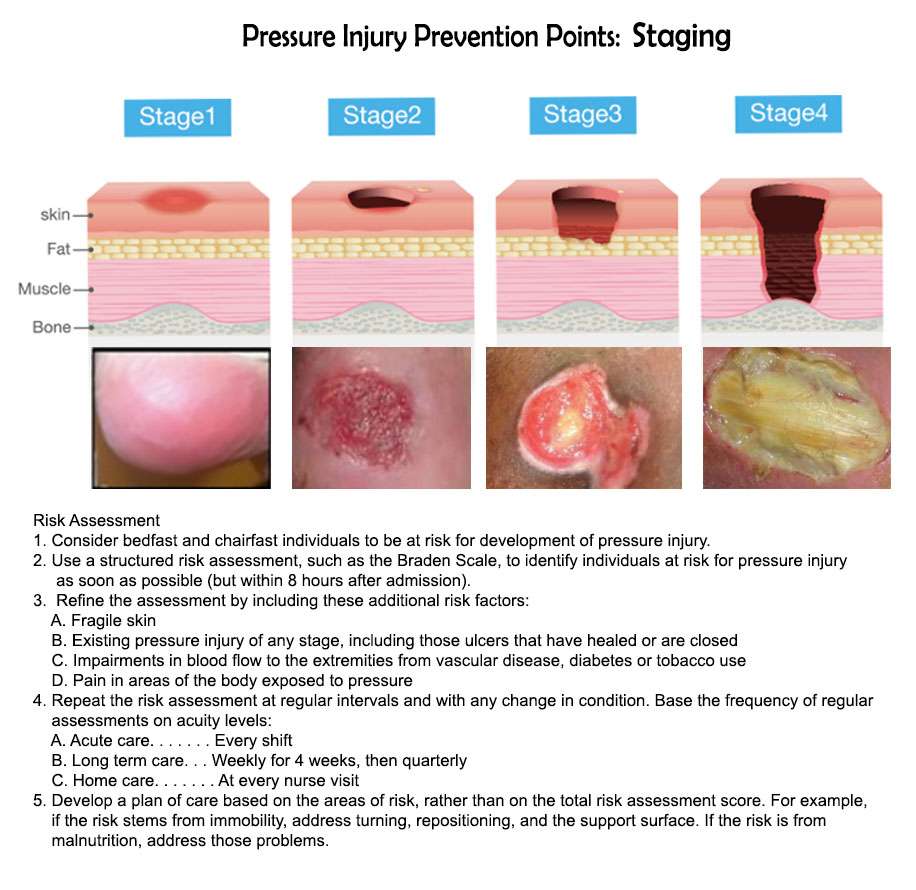
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
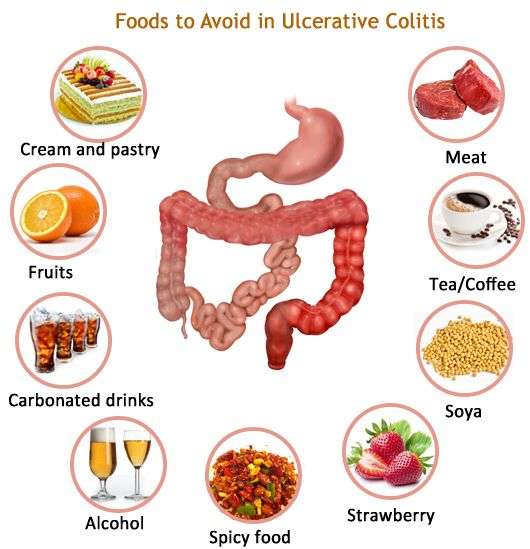
Dont Miss: Foods To Eat If You Have A Stomach Ulcer
Also Check: How Do You Diagnose A Stomach Ulcer
What Other Kinds Of Aids Are Available
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while.
Pressure ulcers often occur on peoples heels. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used. But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn’t been much research on aids such as special positioning cushions or special cushions for people to sit on either.
Bed Sore Staging And Treatment
There are many treatments for each stage, so this list merely highlights common options, advises Dr. Aronson. For all but the most superficial wounds that respond to efforts to decrease pressure or friction, it is very important to seek care from a doctor, nurse practitioner , physician assistant or wound care nurse with specialized expertise in these injuries.
Regardless of the stage of the wound, decreasing pressure to the affected area is necessary to prevent worsening and begin healing. If pain persists once pressure has been taken off the affected area, Dr. Aronson urges family caregivers to seek medical care immediately for their loved ones. This may be a sign of a serious infection or other complication.
You May Like: Signs You May Have Stomach Ulcers
Prone To Sores Every Body Part
Bony protrusions are not the only parts of the body which are exposed to pressure and friction. Other parts are affected, too. For example, when a patient is lying in a supine position, which is the preferred position for critical COVID-19 patients.
Askina® DresSil® is a foam with a silicone adhesive which ensures gentle, secure adherence and minimal trauma during dressing changes. It can be cut and shaped for application on smaller areas which need protection.
Askina® DresSil® Border is a foam dressing with silicone adhesive and an additional adhesive border, are made for difficult-to-dress or moving areas as they are able to conform to a variety of anatomical contours.
Every foam dressing can be repositioned during application or even lifted up during wear time to check the skin or wound. They can also be applied on wounds as they provide a moist environment promoting natural healing.
Treatment Of Decubitus Ulcers
Depending on the stage of the ulcer, treatment can include some or all of the following:
- Cleaning the ulcer and putting a dressing on the wound
- Meticulous wound care with frequent dressing changes
- Reducing pressure on the area by repositioning and using supporting surfaces
- Antibacterial drugs to treat infection
- Pain medications to relieve discomfort
- Debridement surgery to remove dead tissue from the ulcer
- Diet changes and increased fluid intake for faster recovery
Read Also: What Medicine Is Good For Stomach Ulcer
Who Is Most Likely To Get A Pressure Ulcer
Anyone living in a care home can develop a pressure ulcer, but some factors make it more likely.
Risk factors include:
- Limited mobility or being unable to change position without help.
- A loss of feeling in part of the body.
- Having had a pressure ulcer before, or having one now.
- Not having eaten well for a period of time.
- Thin, dry or weak skin.
- A significant cognitive impairment.
Put These Steps Into Action Today
There are many different paths you can take to reducing pressure sores in your facility, and even if seniors in your care receive services at home, every step can be implemented in different types of care settings. Since it is in the best interest of your organization and the seniors you serve, start using these seven steps today, and be creative if you run out of other ideas. You could even have a brainstorming session with caregivers about the best ways to knock out pressure sores for your specific clients too.
Interested in Learning More?
Read Also: Natural Remedies For Leg Ulcers
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
S To Prevent Pressure Sores
By Jason Vanover, on October 11, 2016
Seniors are at risk for a variety of health problems, ranging from physical health deterioration to cognitive decline. While the risk factors for these conditions differ, nearly all seniors are at risk for pressure sores. These sores develop when pressure builds in a specific area of the body over time, and repeated pressure exposure on the same area will result in the degradation of the skins integrity, literally opening the skin up to infection.
Beginning October 2017, the Centers for Medicare and Medicaid Services will begin requiring all health facilities to track and report data reflecting pressure sore development on all clients, and by October 2018, financial penalties will be assessed to health facilities that do not meet these requirements. However, senior caregivers can work to reduce pressure sores among seniors, as well as ailing people of any age, by following these seven steps.
Also Check: How To Prevent Pressure Ulcers On Heels
How Can Friends And Family Help
Caregivers might sometimes provide too much help. For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat.
If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals. This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly. This also includes regularly changing diapers or incontinence pads.
You should tell the nurses or doctors immediately about any red or sore areas of skin. They can then take a closer look at the affected area. It is always important to take pressure off that part of your body.
How Can I Prevent Pressure Ulcers
Pressure ulcers can be avoided, but often you may need help. If you have difficulty moving, preventing pressure ulcers might require a team effort, involving your health team, carer or a family member.
To protect your skin and prevent pressure ulcers, the following will help:
- Keep active and move as much as you can .
- Eat a variety of nutritious foods, including plenty of fruits and vegetables.
- Drink plenty of fluids to make sure you are hydrated.
- Avoid smoking because this reduces blood flow to your skin.
- Avoid firm massage, especially over bony areas.
- Keep your skin dry as far as possible.
- If you feel any skin pain or a feeling of burning, tell your doctor.
There are several things that will help you care for your skin:
- Instead of soap, use a mild cleanser and dry the skin gently afterwards.
- Apply moisturisers if the skin is dry, flaky or seems to crack easily.
- Use barrier cream in skin folds.
- Use warm water when having a bath or shower.
It is important to move around as often as you are able. Continuous pressure on the same areas can lead to a pressure ulcer developing very quickly. The following may help you avoid this:
- Change positions in bed at least every 30 minutes and, if you can, stand up and walk around.
- If you cant stand, move as much as you are able for example, lean forward or move side to side in your chair for 2 minutes to take the pressure off your bottom and hips.
- Try to avoid slumping or sliding forward in your chair.
Don’t Miss: Is Colitis The Same As Ulcerative Colitis
Bone And Joint Infection
Infection can also spread from a pressure ulcer into underlying joints and bones .
Both of these infections can damage the cartilage, tissue and bone. They may also affect the joints and limbs.
Antibiotics are required to treat bone and joint infections. In the most serious of cases, infected bones and joints may need to be surgically removed.
Stages Of Decubitus Ulcers
The National Pressure Ulcer Advisory Panel has developed a series of four stages of a decubitus ulcer to aid in diagnosis and treatment.Stage I: The skin is discolored but not broken. Light-complexioned people may have red marks. Dark complexioned people may have a discoloration that is blue or purple. In some people, the discoloration is white.Stage II: Skin breaks open and the ulcer is shallow with a reddish or pinkish wound bed. There may be tissue death around the wound, or a fluid-filled blister.Stage III: Ulcer on the skin is deeper, affecting the fat layer and looking like a crater. Pus may be in the wound.Stage IV: Ulcer moves to deeper layers of muscle or bone. A dark material called “eschar” may be inside the ulcer.Unstageable: An ulcer that is yellow or green. It might have a brown scab covering it, or be soft and look pus filled. A dry and stable ulcer surface is the body’s natural protection and should be allowed to continue healing. However, if extensive tissue damage is evident, the covering might need to be removed for treatment.
Read Also: Best Over The Counter For Ulcers
Symptoms Of Pressure Ulcers
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
- knees, ankles, heels or toes
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- the back of your arms and legs
- the back of your hip bone
Adapt A Holistic Approach
There are different measures available to prevent pressure ulcers. For example, whenever a patient enters a ward, a pressure ulcer risk assessment should be used, followed by a regular skin assessment to check for any signs of sores.
Also, nutrition plays a huge role in the patients overall health status influencing the probability of developing pressure injuries. It is important to assess the nutritional needs and adapt the diet accordingly and ensure adequate hydration.
Recommended Reading: Peptic Ulcer Vs Gastric Ulcer
The Importance Of Pressure Ulcer Prevention
Pressure ulcers are caused if the blood supply to the skin and the underlying tissues is compromised for prolonged periods of time due to mechanical compression of the local vasulature, with ensuing hypoxia and tissue necrosis. Most of the time, pressure ulcers significantly impact the patients morbidity, mortality and quality of life.
In some cases, these occur quickly – between the first hour and 4 to 6 hours after sustained loading.
Depending on population and ulcer grade, up to 50 percent of pressure injuries can be avoided.
Furthermore, research has proven that the costs of pressure ulcer treatment exceed those of prevention by 2.5 times.
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
You May Like: Natural Home Remedies For Ulcers In Stomach In Tamil
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
What Causes Bedsores
A bedsore develops when blood supply to the skin is cut off for more than 2 to 3 hours. As the skin dies, the bedsore first starts as a red, painful area, which eventually turns purple. Left untreated, the skin can break open and the area can become infected.
A bedsore can become deep. It can extend into the muscle and bone. Once a bedsore develops, it is often very slow to heal. Depending on the severity of the bedsore, the person’s physical condition, and the presence of other diseases , bedsores can take days, months, or even years to heal. They may need surgery to help the healing process.
Bedsores often happen on the:
- Heels of the feet
- Backs and sides of the knees
You May Like: How To Tell If You Have A Stomach Ulcer