Zinc To Speed Up The Healing
Zinc-rich foods like eggs, nuts, and legumes can prove to be very beneficial for both your diabetes and diabetic foot ulcers. Zinc promotes the production and secretion of insulin in the body and thus helps to keep blood sugar levels in check. Zinc also hastens the healing of the wound by maintaining the structural integrity of the dermal tissue.
Peripheral Arterial Disease And The Dfu
What Are The Signs And Symptoms Of Diabetic Foot Ulcers
Foot ulcers are open sores or wounds that occur most often on the ball of your foot or on the bottom of your big toe. They may also develop on the side of your foot, usually because of poorly fitting shoes. The ulcers are usually painless. Not all diabetic foot ulcers become infected but people with diabetes are at high risk of developing infection of the ulcer and the surrounding skin .
Depending on the severity of the wound and the presence of infection, diabetic foot ulcer can be classified in 4 ways:
- Uninfected the wound does not have signs of infection.
- Mild infection the area around the wound may be warm to the touch, red, slightly swollen, painful or tender, and the wound may ooze pus.
- Moderate infection foot infection that involves the deeper layers of your skin, into the muscle, tendons, bone or joints.
- Severe infection foot infection that causes . The symptoms of sepsis are high body temperature , fast heartbeat, and heavy or quick breathing.
Don’t Miss: Can Ibuprofen Help Ulcerative Colitis
How To Treat Ulcers
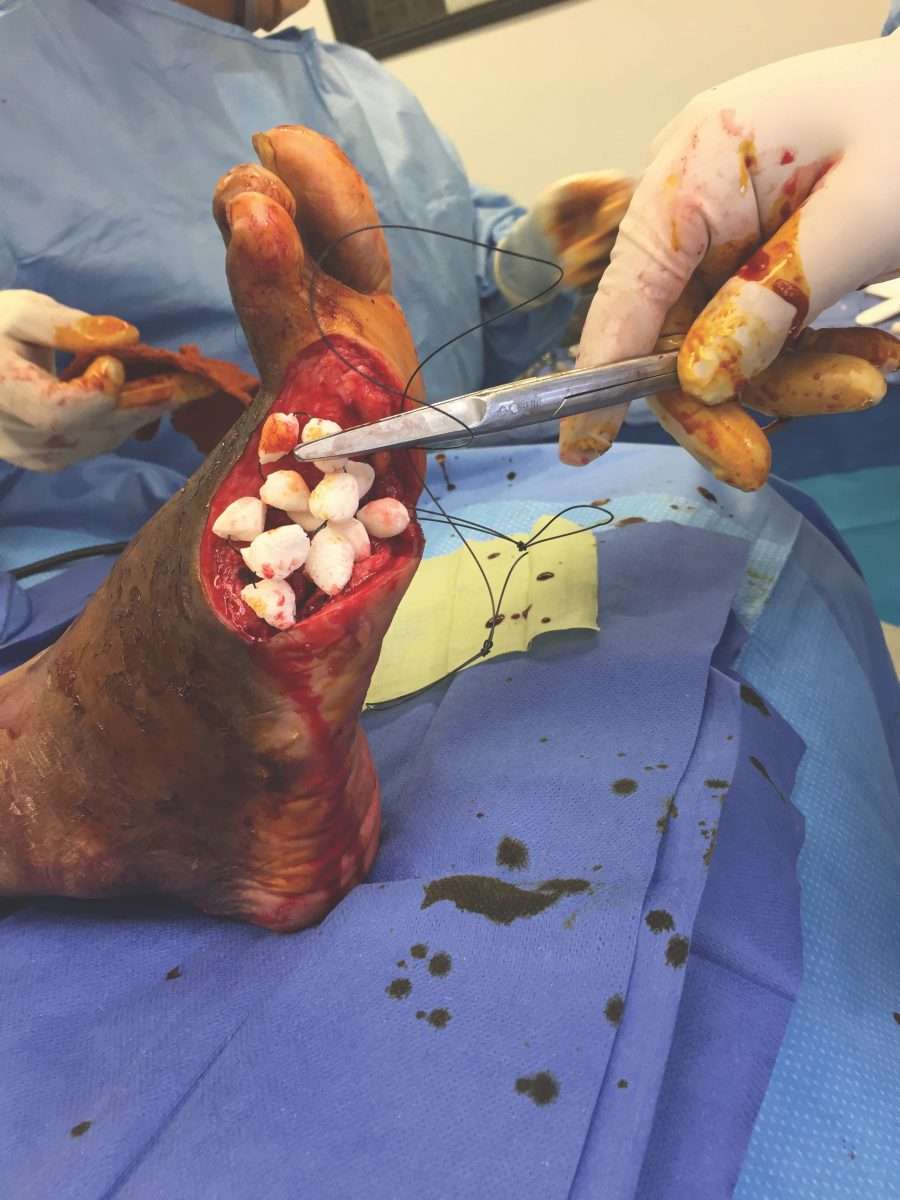
If you do get an ulcer or notice a change in your skin that youâre not sure about, tell your doctor right away. Youâll likely get a procedure called debridement, which removes unhealthy tissue from the wound to spur healing.
Your doctor will also work with you to try to keep your sore or ulcer from getting infected and becoming bigger. Some of the steps they may recommend include:
Clean your ulcer daily. Use soap and water, unless your doctor recommends another cleanser. Donât use hydrogen peroxide or soak your wound in a bath or whirlpool, because this could reduce healing and may boost your odds of infection.
Keep your ulcer bandaged or covered with a wound dressing. While you may have heard that itâs important to âair outâ wounds, experts now know that not covering a wound actually increases the odds of infection and slows healing.
Keep pressure off your ulcer, especially if itâs on your foot. This may mean you need to use crutches, special footwear, a brace, or other devices. Reducing pressure and irritation helps ulcers heal faster.
Use the topical medications your doctor recommends. These may be saline, growth factors, and/or skin substitutes.
Keep your blood sugar under control. In addition to reducing your risk of ulcers, tight blood sugar control helps your body heal existing ulcers.
How Do Diabetic Foot Ulcers Form

Ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation , and trauma, as well as duration of diabetes. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by elevated blood glucose levels over time. The nerve damage often can occur without pain and one may not even be aware of the problem. Your podiatric physician can test feet for neuropathy with a simple and painless tool called a monofilament.
Vascular disease can complicate a foot ulcer, reducing the bodys ability to heal and increasing the risk for an infection. Elevations in blood glucose can reduce the bodys ability to fight off a potential infection and also retard healing.
Read Also: What Causes Ulcers In Your Stomach
Data Sources And Searches
Since the 2006 guidelines, we sought to capture the highest quality of literature available regarding DFU diagnosis and treatment using a key word search of PubMed, Embase, and Cochrane Library databases. Similarly, the citations of relevant articles were examined by hand. Key terms were generated from the existing guidelines. In this search as opposed to the previous data collection prior to 2006, we used human and disease specific data and limited to meta-analyses, systematic reviews, RCTs, retrospective series reviews, clinical case series, and expert panel recommendations published between January 2006 and present. References prior to 2006 supporting the original guideline recommendations are not included. Therefore, in some cases no additional updated references were included and the support for the guideline recommendation is based on evidence presented in the 2006 guideline. Therefore, no updated references are presented. It was further limited to only English publications. Any relevant additional references found after the formal search were also included.
The findings of these articles have been divided into one or more of the appropriate categories as performed in the original guideline
Evidence Reference:
-
- Retrospective series review
Caring For Wounds And Foot Ulcers In Diabetic Patients
The Centers for Disease Control and Prevention reports that there are 30.3 million people living with diabetes in the United States. Diabetes comes with many serious complications, including chronic wounds, nerve damage and foot ulcers.
The American Podiatric Medical Association reports that 15 percent of diabetic patients will develop a foot ulcer. Further, diabetes is the leading cause of nontraumatic, lower-extremity amputations in the U.S. caused by infected wounds and foot ulcers that cannot heal. While difficult to treat, foot ulcers often can be prevented.
Controlling risk factors and monitoring the skin daily is key to minimizing the negative effects of diabetes, said Nancy Estocado, Advanced Wound Care Clinical Coordinator at Sunrise Hospital and Medical Center. For anyone with diabetes, understanding how to prevent and properly address wounds especially foot ulcers is integral to living a healthy life.
Read Also: Wound Vac For Pressure Ulcers
Don’t Miss: How To Prevent Ulcers In The Stomach
Finding The Best Treatment For A Diabetic Foot Ulcer
Youre probably wondering if a person who has no history of diabetes is likely to have a foot ulcer and the answer is yes, its possible. Its important to contact a health professional no matter your current health condition as you do not want symptoms to get worse.
The Wound Institute of America is ready to accept new patients who want to have professional wound care from the number one wound care center in California. To make an appointment with Wound Institute of America or to learn more about your foot ulcer, call 919-4179. You can also learn more about foot ulcers and other wound care treatments on our website here.
What Are Neurotrophic Ulcers
Neurotrophic ulcers occur primarily in people with diabetes, although they can affect anyone who has impaired sensation in their feet. They can be found anywhere on your feet, but they usually develop on the parts of your feet and toes that are most sensitive to weight .
Neurotrophic ulcers dont cause pain. But they can be serious if they arent treated promptly or they dont respond to treatment.
A neurotrophic ulcer might be the following colors:
- Pink.
- Black.
- Any combination of those colors.
The thin borders of the ulcers are punched out, meaning that theyre taller than the surrounding tissues.
Recommended Reading: Medihoney For Stage 1 Pressure Ulcer
How Does Npwt Work For Diabetic Foot Ulcers
1. Drainage of interstitial fluid decreases localized edema, which increases continuous blood flow and decreases tissue bacterial levels.
2. Application of negative pressure produces mechanical deformation or stress within the tissue resulting in protein and matrix molecule synthesis which enhances faster recovery.
A Diabetic Foot Ulcer Can Be Divided Into The Following Category
- No open lesions may have healed lesion.
- Superficial ulcer without penetration to deeper layers.
- Deeper ulcer, reaching tendon, joint capsule, or bone.
- Deeper tissues involved, with abscess, osteomyelitis , or tendonitis
- Gangrene in a portion of the forefoot or heel.
- Extensive gangrenous involvement of the entire foot.
When caught early, foot ulcers are treatable. Visit a wound specialist if you develop any sore. Early detection of infection can reduce the healing time and cost. Infections if not addressed on time may require amputation.
Ulcers may take even longer to heal if you dont control your blood sugar levels or if constant pressure is applied to the ulcer.
Remaining on a diet that helps you meet your glycemic targets and off-loading the affected area.
Recommended Reading: Booties To Prevent Pressure Ulcers
When Should I See My Healthcare Provider About Foot And Toe Ulcers
If you have diabetes, its important to see a podiatrist regularly. Whether you have diabetes or not, you should see a healthcare provider immediately if you find an ulcer on your foot or toe. Left untreated, it could get infected, leading to complications like amputations.
A note from Cleveland Clinic
It can be distressing to discover an open sore on your foot or toe. You might not know what caused it, it might not be healing and, if you have neuropathy from diabetes, you might not even feel it. Keep in mind that your healthcare provider can successfully treat your ulcer, especially if its found early. If left untreated, an ulcer can lead to serious complications.
If you have neuropathy caused by diabetes, remember that its important to check your feet and toes on a regular basis. Check your toes and feet every time you shower or when you go to put on your shoes. Contact your healthcare provider right away if you find an ulcer.
Diagnosis Of Diabetic Foot Osteomyelitis

Recommended Reading: Venous Stasis Ulcer Treatment Dressings
What Is The Outlook For People With Diabetic Foot
Diabetic foot ulcers are fairly common in people who have had diabetes for a long time. Even with foot checks and careful blood glucose monitoring, some people with diabetes develop infections.
The outlook depends on factors such as:
- How early the wound was found.
- Presence of infection and how much it spreads.
- Treatment effectiveness.
If the infection cant be controlled and spreads too far, amputation may be necessary.
Evidence Base For Wound Care Treatments
There is currently little evidence to justify the adoption of very many of the products and procedures currently promoted for use in clinical practice. Guidelines are required to encourage clinicians to adopt only those treatments that have been shown to be effective in robust studies and principally in RCTs. The design and conduct of such RCTs needs improved governance because many are of low standard and do not always provide the evidence that is claimed. There should be new guidance on the conduct of RCTs in this field, and it should embrace items such as those covered in the 21-item checklist of study quality reproduced as . Clinicians need to be able to assess the relative validity of published work, including its strengths and limitations in trial design, conduct, and reporting.
Recommended Reading: How Do I Know If I Have A Peptic Ulcer
Read Also: Foods To Avoid With Peptic Ulcer
How Is A Diabetic Foot Ulcer Diagnosed And Treated
Your healthcare provider will ask about your symptoms and examine your foot and the ulcer. He or she may check your shoes. He or she may also send you to a podiatrist for treatment. The goal of treatment is to start healing your foot ulcer as soon as possible. The risk for infection decreases with faster healing. Do the following to help the ulcer heal:
Nonsurgical Treatment For Diabetic Foot Ulcers
To help a diabetic foot ulcer heal, doctors at NYU Langone clean and disinfect the area. If the ulcer is infected, your doctor prescribes antibiotics to clear it up and prevent it from traveling to a bone in the foot.
Your doctor can refer you to an NYU Langone vascular specialist for additional medication if you have lower extremity arterial disease, a condition that impairs blood flow to the legs and feet and can cause an ulcer to heal more slowly.
NYU Langone doctors recommend regular wound care for foot ulcers, as well as other therapies.
Also Check: What Causes Severe Ulcerative Colitis
Risk Of Foot Ulcers In Patients With Diabetes
A diabetic foot ulcer is a common complication of diabetes mellitus. 19 to 34 percent of people with diabetes will suffer from a diabetic foot ulcer at some point in their lives. The risk of developing such an ulcer increases with time.
The top priority in treating the diabetic foot syndrome is to avoid a major amputation. Because currently, the majority of all foot and lower leg amputations are performed on patients with diabetes mellitus. It is estimated that up to a third of all patients with diabetes suffering from diabetic foot ulcers will undergo amputation.2)
Patients with diabetes are at risk of foot ulcerations due to both peripheral and autonomic neuropathy as well as macro- and microangiopathy.
Who Gets Diabetic Foot Ulcer
Diabetic foot ulcer has an annual incidence of 26% and affects up to 34% of diabetic patients during their lifetime. Risk factors for developing a diabetic foot ulcer include:
- Type 2 diabetes being more common than type 1
- A duration of diabetes of at least 10 years
- Poor diabetic control and high haemoglobin A1c
- Being male
- A past history of diabetic foot ulcer.
Don’t Miss: How To Stop An Ulcerative Colitis Flare
How Should A Diabetic Foot Ulcer Be Treated
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing of the wound, the less chance for an infection.
There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Prevention of infection
- Taking the pressure off the area, called off-loading
- Removing dead skin and tissue, called debridement
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
Not all ulcers are infected however, if your podiatric physician diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
Preventing Infection
There are several important factors to keep an ulcer from becoming infected:
- Keep blood glucose levels under tight control
- Keep the ulcer clean and bandaged
- Cleanse the wound daily, using a wound dressing or bandage
- Do not walk barefoot
Off-Loading
For optimum healing, ulcers, especially those on the bottom of the foot, must be off-loaded. Patients may be asked to wear special footgear, or a brace, specialized castings, or use a wheelchair or crutches. These devices will reduce the pressure and irritation to the ulcer area and help to speed the healing process.
Applying Medication and Dressings
For a wound to heal there must be adequate circulation to the ulcerated area. Your podiatrist may order evaluation test such as noninvasive studies and or consult a vascular surgeon.
Managing Blood Glucose
Management Of Diabetic Foot Ulcer: A Literature Review
Angger Anugerah Hadi Sulistyo2483
Abstract
This article explores the effective management of diabetic foot ulcer. A literature review was conducted by analyzing scholar papers including systematic review, clinical and a randomized control trial published between 2000 to 2016 in the English language. Data were searched through CINAHL, PubMed, Proquest and Google Scholar. The keywords used were diabetic foot ulcer or diabetic foot ulcers or diabetic foot or neuropathic foot ulcer combined with assessment and treatment. There were two kinds of assessment used in diabetic foot ulcer which are risk assessment and wound assessment. The treatments that frequently used in diabetic foot ulcer are systemic treatment and local treatment. This literature review can be used as a guideline and literature for further experimental studies.
Keywords: diabetic foot ulcer, management of foot ulcer, assessment of foot ulcer, treatment of foot ulcer
Abstrak
Kata Kunci: luka kaki diabetes, manajemen luka kaki, pengkajian luka kaki, penanganan luka kaki
Keywords
Full Text:
References
Abbas, Z.G., Lutale, J.K., Game, F.L., & Jeffcoate, W.J. . Comparison of four systems of classification of diabetic foot ulcers in
Tanzania. Diabetic Medicine, 25 , 134137.
Alexiadou, K., & Doupis, J. . Management of diabetic foot ulcers. Diabetes Therapy, 3, 4.
Bentley, J., & Foster, A. . Management of the diabetic foot ulcer: Exercising control. British journal of community nursing, 13 .
Recommended Reading: Can You Die From A Bleeding Ulcer