Colon Cancer Vs Ulcerative Colitis
The main difference between Colon Cancer and Ulcerative Colitis is that Colon cancer is a tumour on the colon wall, which is fatal. At the same time, Ulcerative Colitis is just the immune systems reaction to Candida Albicans proliferation in the colon and is not fatal but incurable.
Colon cancer is a prevalent type of cancer, and still, there are no measures till now which can prevent it or precisely diagnose it at an early stage apart from colonoscopy.
If it gets severe, it is proven to be fatal and brings down the chances of living for five years to 8 per cent.
Ulcerative cancer has a lot of common symptoms to colon cancer, like fatigue.
It is generally considered an autoimmune disease that is the immune system after the body attacks itself. It is a lifelong disease that is incurable but at least not fatal.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Medications That May Help
Some medical therapies for UC may offer built-in protection.
For instance, the review in the Journal of Cancer Research and Therapeutics notes that anti-inflammatory medicines for UC, such as 5-ASA, thiopurines, and steroids, can help protect against the inflammatory damage that leads to cancer.
However, it is worth noting that although the researchers explain that the risk of colorectal cancer for people who took these drugs was similar to that of those who did not, the medications may protect against inflammatory damage without reducing the overall risk of colon cancer.
Another study, this one in the journal Clinical Gastroenterology and Hepatology , suggests that statins, which typically help lower cholesterol in the body, may reduce the risk of colorectal cancer in people with inflammatory bowel disease . The research found that people with IBD who took one or more statin drugs were less likely to develop colorectal cancer than those who did not take the drugs.
Another study, in , found that the anti-inflammatory drug adalimumab helps effectively control inflammation in people with UC. This may reduce the cell damage that gives rise to cancer.
You May Like: Stage 2 Pressure Ulcer Treatment Dressing
Recommended Reading: Tnf Blockers For Ulcerative Colitis
What Are The Risks Of A Colon Cleanse
Regardless of the lack of proven benefits, interest in this type of procedure has stayed steady over the years. And even though it is possible for it to be performed without deleterious effects, there are a number of potential risks that should be taken seriously before considering a colonic:
In addition to these risks, many people who have opted to get a colon cleanse have reported side effects from the actual procedure such as abdominal pain or cramping, bloating, nausea, diarrhea, and vomiting there have even been cases where people have died as a result of the cumulative side effects. These risks are even more pronounced for people who have heart problems or kidney disease because of the challenges associated with maintaining a proper fluid balance. Additionally, people with a weakened immune system can also be more susceptible to the dangers of colon cleansing.
You May Like: Bleeding Ulcer Blood In Stool
Layers Of The Bowel Wall
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, theres inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. More mucus may be produced by the inner layer of the bowel wall. Ulcers develop on the inner layer as the condition gets worse, but they can also go as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When youre having symptoms, its known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section Types of Colitis.
The most common symptoms are:
Andy
Living with Colitis
Read Also: Is Ulcerative Colitis And Colitis The Same Thing
What Foods Cause Colitis
Foods with high fiber content like brown rice, quinoa, oats can trigger the symptoms of Colitis especially Ulcerative colitis . It is difficult to digest high fiber foods which increase the bowel movements and abdominal cramps. Caffeine. Coffee, tea and other caffeine-rich drinks are known to flare up the UC.
Management Of Acute Severe Ulcerative Colitis
- The presence of both of the following indicates acute severe ulcerative colitis :
- ⥠6 bowel movements daily
- ⥠1 sign of systemic toxicity
Neither total parenteral nutrition nor empiric antibiotics are routinely indicated in ASUC.
Also Check: Humira Not Working For Ulcerative Colitis
What Symptoms Do Colitis And Ulcerative Colitis Share
Colitis can cause similar belly and bowel issues no matter the cause. Some symptoms are mild while others are more serious.
General signs of colitis and UC include:
- Stomach cramps that come and go
- Constant belly pain
- Mucus or blood in your poop
- Weight loss without trying
- An urgent need to poop
- A feeling like you didnât get all your poop out
If you have periods, you may have:
- Worsening diarrhea during your period
What Is Ulcerative Colitis In Children
Ulcerative colitis is an inflammatory bowel disease . In this condition, the inner lining of your childs large intestine and rectum gets inflamed. This inflammation often starts in the rectum and lower intestine. Then it spreads to the whole colon.
This causes diarrhea or frequent emptying of the colon. As cells on the surface of the lining of the colon die and fall off, open sores form. This causes pus, mucus, and bleeding.
Dont Miss: Whats A Stomach Ulcer Feel Like
Don’t Miss: Is Ulcerative Colitis An Infection
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
What To Eat For Acid Reflux
Whether its a chronic condition or a newfound symptom of stressful days, heartburn happens! Avoiding spicy, acidic and fried foods as well as cutting back on alcohol and chocolate can help douse the flames and there are some foods you should gravitate towards to help reduce the discomfort. Heres what you can eat to help keep heartburn symptoms from being too upsetting.
Also Check: Can Stress Cause Ulcerative Colitis
Also Check: Can Diet Help Ulcerative Colitis
Actions For This Page
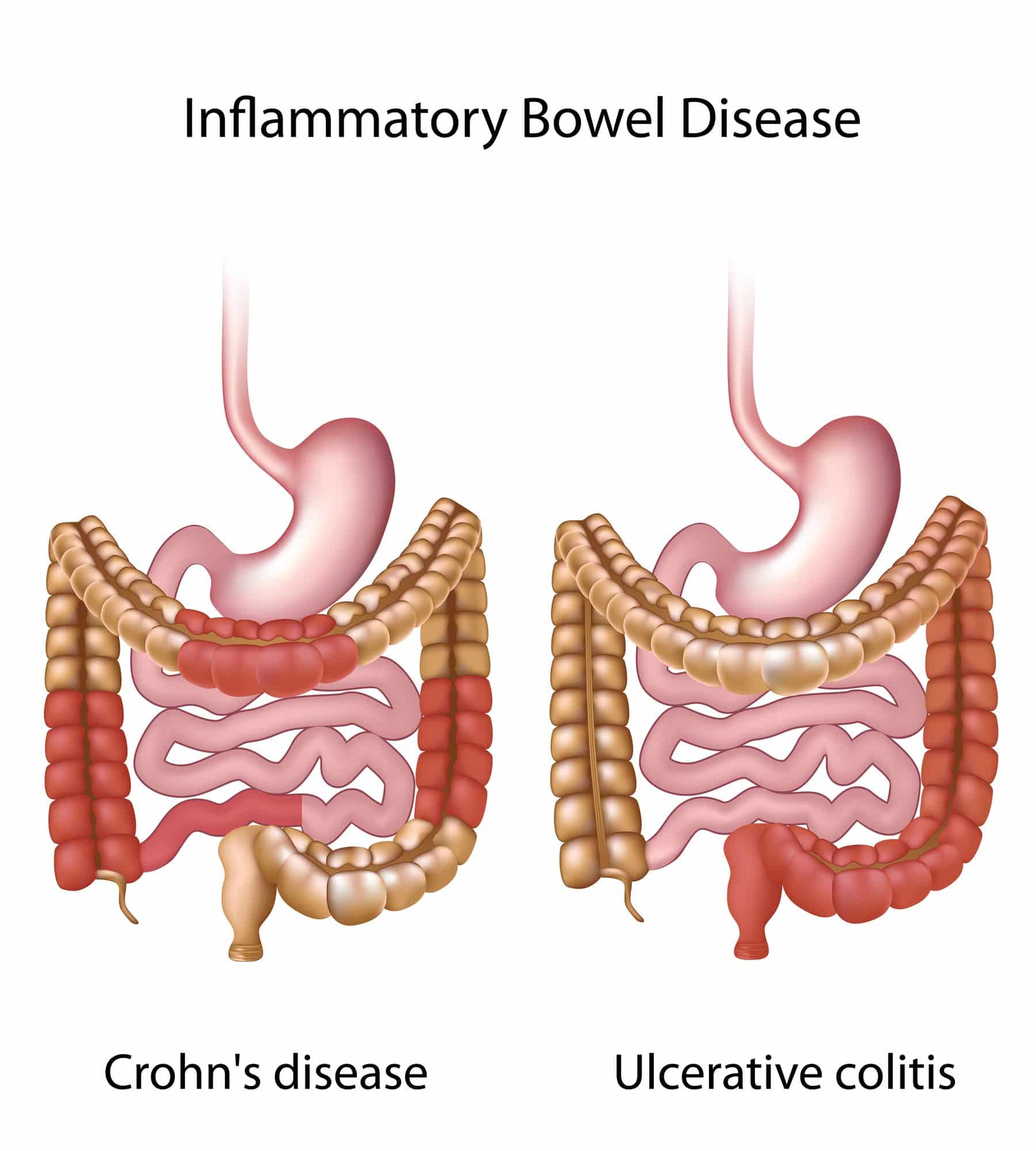
- Crohns disease and ulcerative colitis are collectively known as inflammatory bowel disease .
- Ulcerative colitis is located only in a persons large bowel .
- Diet and food allergies do not cause IBD.
- Medications help manage the symptoms of IBD.
- People with IBD can lead useful and productive lives.
- Some dietary changes can help you manage symptoms of IBD and allow medications to work better.
- Always talk with your doctor, healthcare specialist or dietitian before changing your diet. Arrange an emergency plan of action with your doctor, including after-hours phone numbers.
Abdominal Pain And Bloating
Stomach bloating, distention, cramps or pain in the abdominal or bowel region can be symptoms of colon or rectal cancer. These are common issues that can also be caused by a number of conditions, including diet-related gastrointestinal distress, Crohns disease or ulcerative colitis. See your doctor if you experience frequent abdominal pain and bloating that does not have an obvious cause.
Recommended Reading: Signs And Symptoms Of Diabetic Foot Ulcer
Effects Of Crohns Disease And Ulcerative Colitis
Every person responds differently to IBD. The severity of symptoms will vary from time to time and from person to person. IBD is not a progressive disease . Rather, flare-ups can range from mild to severe and back to mild again. Some people will experience periods of relief from symptoms in between flare-ups.We cannot predict how long a person will stay free from symptoms, or when their next flare-up will occur. Some flare-ups settle down quite quickly with treatment. Other times, it may take months for a persons symptoms to respond to treatment.IBD interferes with a persons normal body functions. Signs and symptoms can include:
- pain in the abdomen
- delayed or impaired growth in children.
How Can We Decrease The Risk Of Crc In Ibd
The positive association between UC and CRC raises several practical questions. The causes behind the changing trends in UC-related CRC epidemiology are complex. One key element may be the early diagnosis and treatment of precancerous lesions by colonoscopic surveillance or sometimes prophylactic colectomy, while the third option is primary chemoprevention. Nowadays, prophylactic colectomy is obsolete. Nonetheless, the high colectomy rate, especially in Scandinavian countries has been associated with lower CRC risks. There are however, obvious changes in the patient management, also in Scandinavia. In the new population-based cohorts, a decrease in the colectomy rate can be observed.
Also Check: Best Foods To Eat With Ulcerative Colitis
Coffee Enemas To Clear The Colon
Compared to colonics, enemas are done at your home in private. They are inexpensive compared to a more costly visit to your colon hydrotherapist. You can buy kits at any drugs store or online. Here is a great stainless steel kit that I recommend.
Enemas also work by cleansing your colons with water. In some cases, coffee, wheatgrass, herbs, or apple cider vinegar is added for extra cleansing. While colonics target your entire intestine, enemas are targeting your descending colon only. Here is a helpful article on how to do a coffee enema.
If you choose to get a colonic or try an enema yourself, it is important that you take probiotics to support your healthy gut flora. Colonics clean your colon from waste, toxins, bacteria, fungi, and parasites. However, they also clean out good bacteria in the process.
Taking high-quality probiotics and eating a nutrient-dense, gut-supporting diet is important to achieve long-term results. Continue reading for further tips on how to reset your microbiome after a colon cleanse.
Also Check: Stage 4 Decubitus Ulcer Treatment
Leukocyte Telomeres Are Significantly Shorter In Uc Patients Than In Normal Controls
Leukocyte telomere length significantly decreased with age, both in UC patients and in normal controls . Since these two populations were not matched for age and gender, we used a linear regression model to compare leukocyte telomere length in both groups after age and gender adjustments. This showed slightly, but significantly shorter telomeres in leukocytes from UC patients compared to normal individuals . The adjusted leukocyte telomere length means calculated at age 50 were 1.22±0.24 for control and 1.14±0.23 for UC, a 6.6% difference. There were no significant associations between age-adjusted leukocyte telomere length and disease activity or medication use, although there was a non-significant trend for longer telomeres in patients that used 5-ASA.
Association between leukocyte telomere length and age in UC patients and normal individuals . Simple regression lines are shown for UC patients and normal controls .
Don’t Miss: Can Ulcerative Colitis Cause High White Blood Cell Count
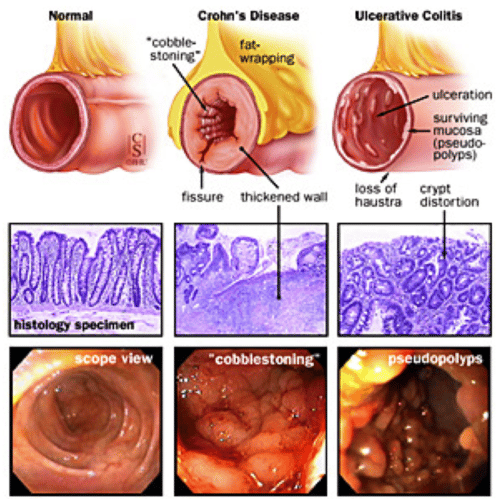
Evaluation Of Colectomy Specimens
In resection specimens, UC typically shows diffuse continuous mucosal disease , in the absence of fissuring ulcers, fistula tracts, transmural inflammation, small bowel involvement, or granulomas. However, in certain clinical settings, atypical features may be observed in colectomy specimens for UC. These atypical features include discontinuous disease and rectal sparing in medically treated or fulminant UC, and deep fissuring ulceration in fulminant UC.
What Is Colon Cancer
Colon cancer is a common disease, and it is a growth of abnormal cells that gradually spreads to other organs of the body.
It is hard to identify it in the early stages, and therefore, its chances of becoming fatal increase even more.
Starting like a polyp or growth of an abnormal tumour on the walls of the colon, it gradually grows and after years becomes apparent.
It can have minor symptoms that include diarrhoea, changes in bowel systems, constipation, Malena, narrow stools or reduction in faeces, fatigue, unexpected weight loss, and bloating.
Colon cancer causes gripping and acute pain. Colonoscopy is a great way to detect colon cancer and an early stage. It is generated for many known and unknown reasons.
The most common cause of colon cancer is Hereditary, a family history of colon cancer, an ongoing or past case of ovarian cancer, Crohns disease, etc. It usually happens before 40 years of age.
After detection of colon cancer, if the polyps are few, then they can be easily removed during colonoscopy by a method known as polypectomy in this case.
Apart from this, surgical treatments that mean removing the colon part affected by surgery that is further followed by chemotherapy and radiation treatment are also considered for treating colon cancer.
Radiation treatment is brought into work when the surgery does not succeed.
Recommended Reading: Things Not To Eat With A Stomach Ulcer
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Vitamin And Mineral Supplements For Ibd

A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
Recommended Reading: Chicken Recipes For Ulcerative Colitis
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
How Is Ibd Diagnosed
- A combination of endoscopy or colonoscopy and imaging studies, such as:
- Contrast radiography.
- Types of common medications to treat IBD:
- 5-aminosalicyclic acids.
Links with this icon indicate that you are leaving the CDC website.
- The Centers for Disease Control and Prevention cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website’s privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance on other federal or private website.
Read Also: Ulcerative Colitis Increased Risk Of Colon Cancer
Upper Gastrointestinal Tract Manifestations
While UC is traditionally considered to be a disease of the colon, inflammation of the upper gastro-intestinal tract has been described in a small proportion of UC patients. Gastric findings in UC patients include superficial plasmacytosis, focal gastritis, and basal mixed inflammation . Duodenal pathology in UC includes diffuse chronic active duodenitis and intra-epithelial lymphocytosis, with or without partial villous atrophy. None of these patterns of upper GI inflammation are diagnostically specific for UC in the absence of granulomas, the presence of upper GI inflammation in IBD patients should not necessarily be equated to Crohns disease.
What Are The Causes Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Causes
Most colorectal cancers arise from adenomatous polyps. Such polyps are comprised of excess numbers of both normal and abnormal appearing cells in the glands covering the inner wall of the colon. Over time, these abnormal growths enlarge and ultimately degenerate to become adenocarcinomas.
People with certain genetic abnormalities develop what are known as familial adenomatous polyposis syndromes. Such people have a greater-than-normal risk of colorectal cancer. In these conditions, numerous adenomatous polyps develop in the colon, ultimately leading to colon cancer. There are specific genetic abnormalities found in the two main forms of familial adenomatous polyposis.
Adenomatous polyposis syndromes tend to run in families, which are referred to as familial adenomatous polyposis . Celecoxib has been FDA approved for familial adenomatous polyposis. After six months, celecoxib reduced the mean number of rectal and colon polyps by 28% compared to placebo 5%.
Other risk factors for developing colon cancer include:
- Ulcerative colitis or Crohns disease
- Breast, uterine, or ovarian cancer now or in the past
- A family history of colon cancer
- Colon cancer usually occurs before age 40 years.
Ulcerative Colitis Causes
Emotional stress or food sensitivities do not cause ulcerative colitis however, these factors may trigger symptoms in some people.
Risk factors for inflammatory bowel disease include:
You May Like: Can Foot Ulcers Be Cured