Ulcerative Colitis And Colonoscopy
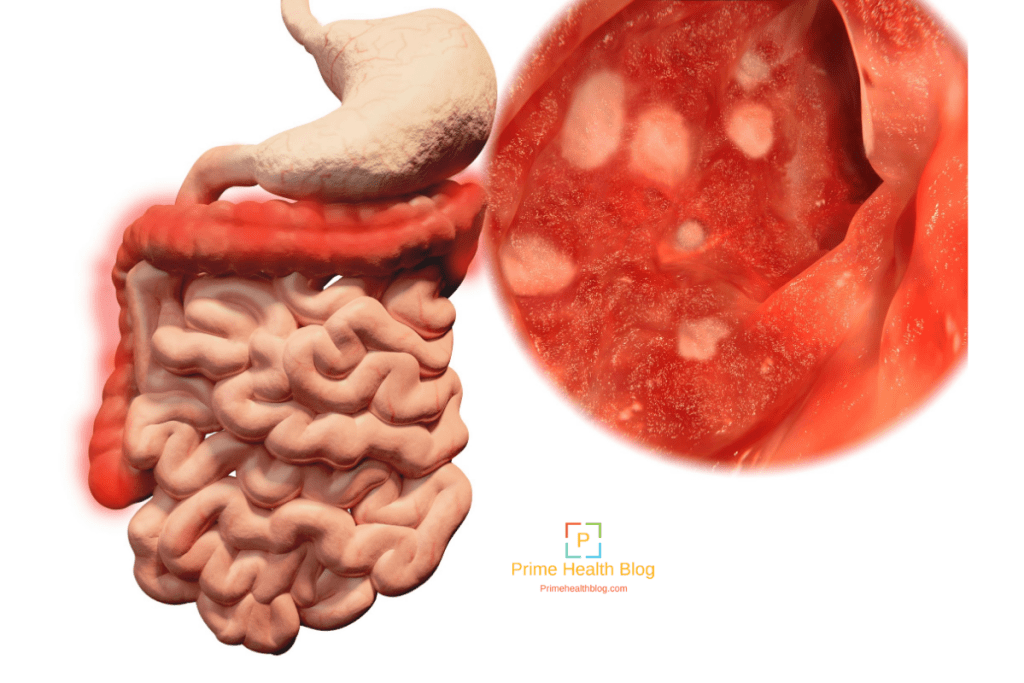
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
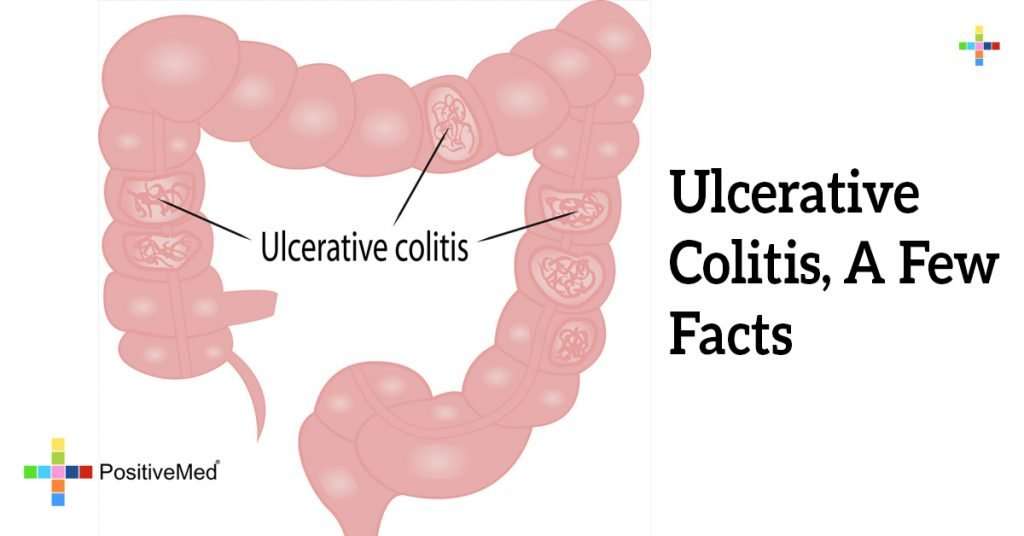
Symptoms By Type Of Ulcerative Colitis
Ulcerative colitis can be broken into subtypes depending on where the inflammation is in your colon.
- Ulcerative proctitis. Ulcerative proctitis affects your rectum, the part of your colon closest to your anus. Its the most common type and affects 30 to 60 percent of people with ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis causes inflammation of your rectum and the lower part of your colon, called the sigmoid colon.
- Left-sided colitis. Left-sided colitis affects your rectum, your sigmoid colon, and the descending part of your colon on the left side of your body.
- Pancolitis.Pancolitis affects your entire colon.
Symptoms typically become worse as inflammation spreads farther along your colon.
| Ulcerative proctitis |
show ulcerative colitis is slightly more prevalent in men, but most studies show no difference.
Symptoms of ulcerative colitis are similar regardless of sex, but unique issues may occur for some people.
Rectovaginal fistulas may develop, which are holes that allow stool to leak from the bowel to the vagina.
Ulcerative colitis may also lead to irregular periods or increased menstrual pain. Women may also be at a higher risk of anemia and osteoporosis, and ulcerative colitis can further increase this risk.
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Don’t Miss: Best Protein For Ulcerative Colitis
Duration Of Ulcerative Colitis
Your risk for colon cancer typically starts to increase once youve lived with UC for about 8 to 10 years, according to the Crohns & Colitis Foundation. The longer you have UC, the higher your cancer risk.
According to a 2019 literature review , colorectal cancer rates for people in North America increase dramatically after a person has lived with UC for 30 years.
Colorectal cancer rates in Asia increase dramatically after a UC duration of 10 to 20 years. Cancer rates for Asian people whove had UC for 10 to 20 years were four times higher than rates for Asian people whove had UC for 1 to 9 years.
Cancer rates for Europeans also increased as UC duration increased. However, the increase in cancer rates over time wasnt considered statistically significant. There wasnt enough data from Oceania to compare cancer rates over time.
This literature review had some noteworthy limitations. For instance, data wasnt included for people whod had colorectal polyps or a colectomy for UC.
Data for people with cancer outside of the colon or rectum, or those with a family history of colorectal cancer, was also excluded.
Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
You May Like: Diet For Gerd And Ulcers
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you don’t get treatment for UC. That’s because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if you’ve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesn’t go away.
- You’re a man.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member who’s had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think it’s because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
What Is The Cause Of Ulcerative Colitis
The cause of ulcerative colitis is unknown but it seems to be related to genetics and how the environment affects the immune system. Ulcerative colitis is not infectious.
There also appears to be a change in the gut bacteria of people with ulcerative colitis but it still isnt clear if the change is caused by inflammation.
Certain genes make people more likely to develop ulcerative colitis and can be triggered or activated by something in the environment. Research is ongoing to discover which environmental conditions are risk factors for developing the disease. As an example, ulcerative colitis is more common in non-smokers or ex-smokers but the reason for this is not known.
People who have one or both parents with ulcerative colitis are more likely to develop the IBD. You can learn more about inheriting or passing on ulcerative colitis at Fertility, Pregnancy and IBD.
Recommended Reading: Cpt Code For Ulcerative Colitis
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
Symptom Development And Flares
The symptoms of UC usually start out fairly mild, such as slightly looser or more frequent bowel movements. The symptoms may become more severe as inflammation worsens and open sores develop in the bowel. Eventually, a person with UC might experience fatigue, fever, nausea, and weight loss.
Some people experience ulcerative colitis constantly. However, it is more common to have flare-ups, during which symptoms begin or worsen, followed by periods of remission, when symptoms go away or improve for a while.
Don’t Miss: How To Relieve A Stomach Ulcer
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Recommended Reading: How To Apply Compression Bandages For Leg Ulcers
Complications In The Intestine
Malabsorption and Malnutrition
Malabsorption is the inability of the intestines to absorb nutrients. In inflammatory bowel disease , this occurs as a result of bleeding and diarrhea, as a side effect from some of the medications, and as a result of surgery. Malnutrition may occur in ulcerative colitis, but it tends to be less severe than with Crohn disease.
Toxic Megacolon
Toxic megacolon is a serious complication that can occur if inflammation spreads into the deeper layers of the colon. In such cases, the colon enlarges and becomes paralyzed. In severe cases, it may rupture, which is a life-threatening event requiring emergency surgery. Symptoms include weakness, abdominal pain, abdominal distention, and frequently, fever.
Toxic megacolon is characterized by extreme inflammation and distention of the colon. Common symptoms are pain, distention of the abdomen, fever, rapid heart rate, and dehydration. This is a life-threatening complication that requires immediate treatment, usually surgical removal of the colon.
Bleeding and Anemia
Rectal bleeding due to ulcers in the colon is a common complication of ulcerative colitis. It can increase the risk for anemia . In some cases, internal bleeding can be massive and dangerous, requiring surgery.
Intestinal Infections
Colorectal Cancer
How To Treat Ulcerative Colitis
The treatment of Ulcerative Colitis also depends upon the severity of the patient. The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis.
Following drugs may calm down the inflammation and make the patient feel better.
You May Like: Can You Take Imodium If You Have Ulcerative Colitis
What Are The Symptoms During A Flare
- Diarrhoea. This varies from mild to severe. The diarrhoea may be mixed with mucus or pus. An urgency to get to the toilet is common. A feeling of wanting to go to the toilet but with nothing to pass is also common . Water is not absorbed so well in the inflamed colon, which makes the diarrhoea watery.
- Blood mixed with diarrhoea is common .
- Crampy pains in the tummy .
- Pain when passing stools.
Feeling generally unwell is typical if the flare-up affects a large amount of the colon and the rectum , or lasts for a long time. High temperature , tiredness, feeling sick , weight loss and anaemia may develop.
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Don’t Miss: Do Enemas Help Ulcerative Colitis
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Ulcerative proctitis has very few complications but with increased irritation to the anal and rectal area, hemorrhoids may occur. Only rarely do other complications occur, such as abscesses and extra-intestinal manifestations. Individuals with ulcerative proctitis are not at any greater risk for developing colorectal cancer than those without the disease.
Recommended Reading: Best Anti Diarrhea Medicine For Ulcerative Colitis
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
Don’t Miss: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
Prognosis Of Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have ulcerative proctitis have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
Treat To Target Disease Monitoring And Long
The treatment strategy in ulcerative colitis has evolved into a treat to target approach, in which patients are regularly assessed to ensure they are meeting strict targets for disease control. The targets for ulcerative colitis are resolution of patient reported outcomes and endoscopic remission. Given the importance of endoscopic healing, the colon should be directly assessed 36 months following the initiation of a new treatment. Flexible sigmoidoscopy is sufficient for assessing endoscopic healing. Patients should have a regular follow-up at a minimum of every 3 months until symptom resolution, and then at least every 612 months with the goal of maintaining tight control. Once patients are in remission, non-invasive markers, such as fecal calprotectin, can be used to monitor disease activity. In a post-hoc analysis of a clinical trial, a fecal calprotectin cutoff of 150 mg/kg was best for endoscopic remission .
Don’t Miss: Best Dressing For Decubitus Ulcers