What Are The Types Of Ulcerative Colitis
The different types of ulcerative colitis are defined by the location of the inflammation, explains Aja McCutchen, MD, a gastroenterologist at Atlanta Gastroenterology Associates. The four types of UC are:
Ulcerative proctitis
Inflammation occurs in just the rectum.
Proctosigmoiditis
Inflammation occurs in the rectum and the sigmoid colon, the area right above the rectum.
Left-sided colitis
Inflammation occurs from the rectum to the descending colon.
Pancolitis
The entire colon is affected.
How To Prevent Ulcerative Colitis
Unfortunately, theres no way to prevent ulcerative colitis. The best thing anyone with UC can do is work to prevent flare-ups making lifestyle changes:
- Dietary changes. Most nutrient absorption occurs in the small intestine, which doesnt play a role in UC, so theres no universal diet for this condition, Dr. McCutchen says. It can help to keep a food journal so you can note when flare-ups happen. You may notice that certain foods, such as those high in fiber, sugars, or fats, exacerbate your symptoms. Discuss any dietary changes with your healthcare provider or a registered dietitian experienced at working with people who have UC.
- Stress management. Stress also appears to increase the likelihood of flare-ups. I really encourage IBD patients to see a therapist or mental health provider who is versed in IBD and can help them manage their symptoms, Dr. McCutchen says. Additionally, things like yoga, regular exercise, , and mindfulness practices may help manage the symptoms of ulcerative colitis.
- Medication changes. Non-steroidal anti-inflammatories can cause flare-ups. Ask your doctor about alternative options for pain management when needed.
References
What Are Somelifestyle Changes People Can Make To Improve Their Ibd
Work with your healthcare professional or a dietitian to create a meal plan that works for you. Knowing your food triggers and maintaining good nutrition are both important ways to help control your symptoms. Moderate exercise and finding ways to reduce your stress, such as incorporating yoga or mindfulness into your daily routine, can also help relieve IBD symptoms.
Also Check: Icd 10 Code For Ulcerative Colitis With Bleeding
How Do Ibd Andcovid
While diarrhea, stomach pain and vomiting can be symptoms of both COVID-19 and IBD, people with COVID-19 often have respiratory symptoms as well, including shortness of breath and cough and fever. If you’re experiencing any of these symptoms, be sure to contact your healthcare provider.
This resource was created with support from Bausch Health, Bristol-Myers Squibb, Ferring Pharmaceuticals, and Takeda Pharmaceuticals U.S.A, Inc.
How Do I Spot The Signs And Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are abdominal pain and diarrhea, which often contains blood or pus.
Symptoms of the disease typically develop gradually and come and go.
Periods without active disease known as remission may last for months or even years.
Over time, ulcerative colitis can progress to cover more of the colon. This typically leads to more severe disease and greater symptoms.
If left untreated, UC can also lead to a number of complications:
Also Check: Signs Of A Bleeding Stomach Ulcer
Theres More Than One Type Of Ulcerative Colitis
All UC affects the rectum, but different types of ulcerative colitis travel farther up the colon. Ulcerative proctitis is limited to the rectum and tends to be milder than the other forms. Proctosigmoiditis involves inflammation in both the rectum and the lower section of the colon, while left-sided colitis extends from the rectum farther into the large intestine. Total colitis, which affects the entire large bowel, is rare. Doctors will consider the severity and areas affected by UC when suggesting a treatment.
Effects Of Crohns Disease And Ulcerative Colitis
Every person responds differently to IBD. The severity of symptoms will vary from time to time and from person to person. IBD is not a progressive disease . Rather, flare-ups can range from mild to severe and back to mild again. Some people will experience periods of relief from symptoms in between flare-ups.We cannot predict how long a person will stay free from symptoms, or when their next flare-up will occur. Some flare-ups settle down quite quickly with treatment. Other times, it may take months for a persons symptoms to respond to treatment.IBD interferes with a persons normal body functions. Signs and symptoms can include:
- pain in the abdomen
- delayed or impaired growth in children.
Don’t Miss: What Are The First Signs Of A Stomach Ulcer
Certain Personalities Are Prone To Ibd
Fact: The underlying cause of IBD is biological, not emotional. About 50 years ago, it was believed that IBD was part of a group of medical disorders that were characteristic of certain personality traits and a specific biological predisposition. The latest research does not show this to be true. In fact, earlier studies have concluded that psychoanalysis actually worsened the cases of ulcerative colitis because no other treatment was offered.
Cause Of Ulcerative Colitis
Despite many research studies and test trials, the cause of ulcerative colitis is not known. In the past, it has been suspected that stress and diet may have caused the condition. However, there is not enough research to back these claims. It is now thought that diet and stress can aggravate ulcerative colitis but they are not the cause. A possible cause of the disease is an abnormal immune system response. This may occur when the immune system acts to combat an invading bacterium or virus and instead the immune system attacks the cells of the gastrointestinal tract as well. Another cause may be genetics, as ulcerative colitis tends to be more prevalent amongst individuals who already have a family member with the disease.
Recommended Reading: What Is A Gastric Ulcer And What Is Its Cause
If You Start Biologics Stay On Biologics
While your doctor might agree to let you stop taking medication if youve been in remission for a long time, you should continue biologics treatment if you can, says Glenn H. Englander, MD, gastroenterologist in West Palm Beach, Florida. Young people dont want to stay on medicine for the rest of their lives, he says. But the body can build up antibodies to biologics if you stop taking them, so its best to keep up with treatment.
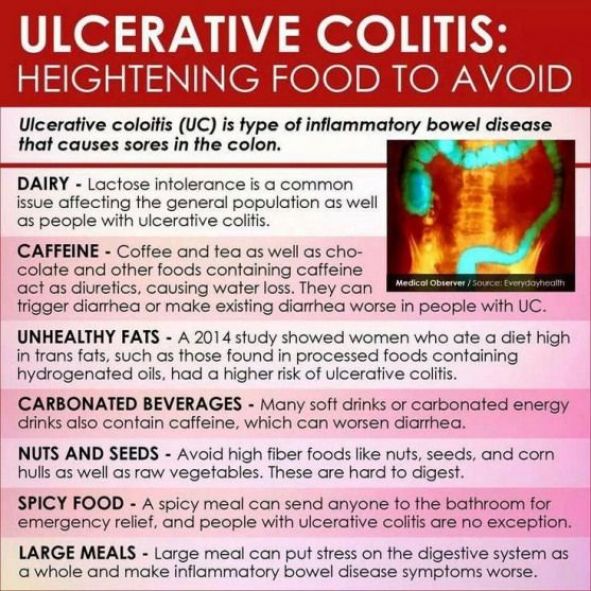
Youre Eating Large Meals
When UC symptoms are active, you can ease your bodys burden by eating frequent, smaller meals so the volume of food and fluid is stable and limited. Consider having five or six fist-sized meals every three to four hours instead of three large meals a day.
On top of helping reduce discomfort from UC symptoms, this strategy is also a way to cope with nausea or loss of appetite that might accompany your flare.
Read Also: How To Cure An Ulcer In Your Stomach
Myth : Ulcerative Colitis Develops Due To Wheat And Gluten Intolerances
Ulcerative colitis is not due to food allergies or intolerances.
However, some people with ulcerative colitis do find that eating certain foods makes their symptoms worse. For example, spicy foods, high fat foods, and dairy products are common triggers in people with ulcerative colitis.
Some people with ulcerative colitis also have food allergies or intolerances, such as celiac disease. This is a condition in which wheat and other gluten-containing grains trigger an immune reaction.
A 2020 review of studies found that celiac disease is more common than average among people with ulcerative colitis. However, most people with ulcerative colitis do not have celiac disease.
A person should speak with a doctor if they think that they might have a food allergy or intolerance. The doctor may refer them to an allergist.
The doctor may also refer them to a registered dietitian, who can help them identify food triggers and develop a diet plan to meet their needs.
Youre Not Drinking Enough Fluids

If youre experiencing bouts of diarrhea, you run the risk of becoming dehydrated, because your body is losing more fluids than its taking in. This can be harmful to your overall well-being and interfere with your bodys ability to heal.
Drink as much water as you can during a UC flare. Just keep in mind that there are some liquids you should think twice about if you have diarrhea, including pear, peach, or prune juice, according to the Crohns & Colitis Foundation all of them contain nonabsorbable sugars that can be rough on your gut. Try, too, to avoid alcohol, caffeinated drinks, and carbonated beverages.
Recommended Reading: Signs And Symptoms Of Peptic Ulcer
What Are The Symptoms Of Ulcerative Colitis
Symptoms of ulcerative colitis come and go. A flare-up can be severe for a few days or weeks and then go away or at least get better for a while. For most people, symptoms continue to flare up on and off throughout their life.
Usually, a flare-up begins slowly. Symptoms include:
-
A strong urge to pass stool
-
Mild cramps in your lower belly
-
Blood and mucus in your stool
A flare-up may be sudden and severe, causing:
-
Violent diarrhea often with a lot of mucus and blood
Sometimes in a severe flare up, your large intestine swells up a lot and may develop a small hole . A perforation lets stool leak into your belly, which can cause a life-threatening infection .
If you’ve had ulcerative colitis for a long time, you can have:
-
Problems with your liver and gallbladder
-
Low blood count
Myth : You Can Stop Taking Your Medications Once You Feel Better
Biologics and other medications that reduce inflammation may help bring ulcerative colitis into remission. Remission refers to when inflammation is under control and a person is not experiencing ulcerative colitis symptoms.
If someone stops taking medications to treat ulcerative colitis, they may experience a relapse. Inflammation and symptoms may return. Their medications might not work as well if they start taking them again.
Sometimes, it is possible for a doctor to lower a persons prescribed dosage of certain medications or reduce the number of medications they take without triggering a relapse.
People with ulcerative colitis should speak with a doctor before they stop taking medications or make any other changes to their treatment plan for ulcerative colitis.
A doctor can help a person weigh the potential benefits and risks of changing their treatment plan and monitor them for any symptoms of relapse.
Read Also: Diet Plan For Ulcerative Colitis Flare Up
What Are The Symptomsbeyond The Intestines That Affect Overall Health
People with both Crohn’s disease and ulcerative colitis can experience symptoms outside of the GI tract, such as arthritis and joint pains eye and vision problems and skin disorders, including mouth ulcers and skin rashes. Women with IBD are more likely to experience premenstrual symptoms and iron-deficiency anemia. Women with IBD who have had certain surgeries can have higher rates of infertility compared to the general population. It is important to discuss family planning with your physician prior to considering any elective surgery for IBD.
Things You Need To Know About Ulcerative Colitis
Following Siobhan-Marie O’Connor’s superb performance at the Rio Olympics, we have published these facts and infographics about Ulcerative Colitis.
Read Also: Is Keto Good For Ulcerative Colitis
Complications Of Ulcerative Colitis
As ulcerative colitis progresses and if it remains severe, there are possible complications associated with the condition. Potential complications of the disease include osteoporosis severe bleeding heightened risk of blood clots in arteries and veins liver disease perforated colon severe dehydration inflammation of eyes and skin arthritis toxic megacolon increased risk of colorectal cancer primary sclerosing cholangitis . Some medications used to treat ulcerative colitis can cause some complications. For example, the prolonged use of corticosteroid medication which is used to treat UC can lead to osteoporosis and the weakening of the bones. In children and adolescents, failure to grow or poor growth and development can occur as a complication of ulcerative colitis.
Ulcerative Colitis: A Definition
The intestinal disease ulcerative colitis is characterised by the following properties, among others:
- The inflammation usually only affects the large intestine.
- The inflamed area in the intestine is continuous.
- The inflammation affects the upper intestinal layer.
This clearly distinguishes ulcerative colitis from the most common intestinal disease Crohns disease. Other parts of the digestive system may also be affected by the inflammation. In Crohns disease the inflammation is not distributed on a continuous surface and also affects deeper layers under the intestinal mucosa.
Recommended Reading: What Can Cause Ulcerative Colitis Flare Ups
Youre Skipping Your Uc Medications
The most important thing to do if you have UC? Take your medications as prescribed, and work closely with your doctor to stay well, says Richard Bloomfeld, MD, a gastroenterologist and professor at Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
A variety of medications can treat UC, depending on the severity of your condition and your overall health. While it may be tempting to skip doses once you start feeling better a report published in the journal Intestinal Research reported that medication adherence is a significant problem for people who have inflammatory bowel disease doing so can cause your symptoms to reappear.
Skipping medications is the biggest reason people experience flares, says Laura Yun, MD, a gastroenterologist and assistant professor of medicine at Feinberg School of Medicine at Northwestern University in Chicago. Whether your doctor has you taking an anti-inflammatory drug, an immunosuppressant, or a combination of medications, none of them will work if you dont take them as your doctor prescribes.
Favorite Resource For Diet Advice
This book by A. Hillary Steinhart, MD, provides dietary strategies and recipes to help manage inflammatory bowel disease. The head of the combined division of gastroenterology for Mount Sinai Hospital and the University Health Network in Torontos Mount Sinai Hospital, Dr. Steinhart worked with the clinical dietitian Julie Cepo to offer well-researched dietary advice for people to maintain health during flare-ups as well as periods of remission. The book is packed with 150 recipes, from risotto to stew, to help anyone with IBD eat well and prevent malnutrition.
Doctors assured Danielle Walker that her diet was not a factor in her ulcerative colitis flares. But after years of suffering and multiple hospitalizations, Walker realized that she needed to make dietary changes. At the two-year remission mark, the mom, wife, and self-trained chef began blogging about her experience and sharing recipes to help others struggling with IBD. You can buy Walkers cookbooks on her website, which is loaded with nutritional resources including a blog and videos.
Recommended Reading: How Do You Develop Stomach Ulcers
When To See A Doctor
It is important to note that IBD and irritable bowel syndrome often get confused. IBS may present with some of the same symptoms that can cause discomfort and pain, but it is non-inflammatory in nature. So, while IBS symptoms can affect your quality of life, the condition does not have the likelihood of causing permanent damage, as with IBD.
Symptoms between the two conditions are common, with ailments such as diarrhea, abdominal pain and cramping, weight loss, fatigue, and nausea. If you experience a number of these symptoms for over 10 days to two weeks, its a good idea to consult your gastroenterologist for a clear diagnosis and treatment of symptoms. IBD is more dangerous than IBS, and at the very least should be ruled out.
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
Don’t Miss: What Not To Eat If You Have An Ulcer
What Are The Risk Factors Of Ulcerative Colitis
The cause of ulcerative colitis is unclear, but its thought that a combination of genetics and environmental factors are at play. Up to 20 percent of people with ulcerative colitis have a parent, sibling or child with the disease.
Ulcerative colitis is more common for people living in urban, industrialized areas compared to undeveloped countries, which indicates that highly refined diets may play a role. Although all ethnic groups are affected, the problem is most common among Caucasians and people of Eastern European Jewish descent.
Lastly, there appears to be a connection to nonsteroidal anti-inflammatory medications. Its not that these medications cause the disease but, because they inflame the bowel, they can worsen symptoms. This category of medication includes ibuprofen , naproxen sodium and diclofenac sodium .