What Measures Are Included In The Hac Reduction Program
The following measures are included in the HAC Reduction Program, grouped here by category:
Patient Safety and Adverse Events Composite
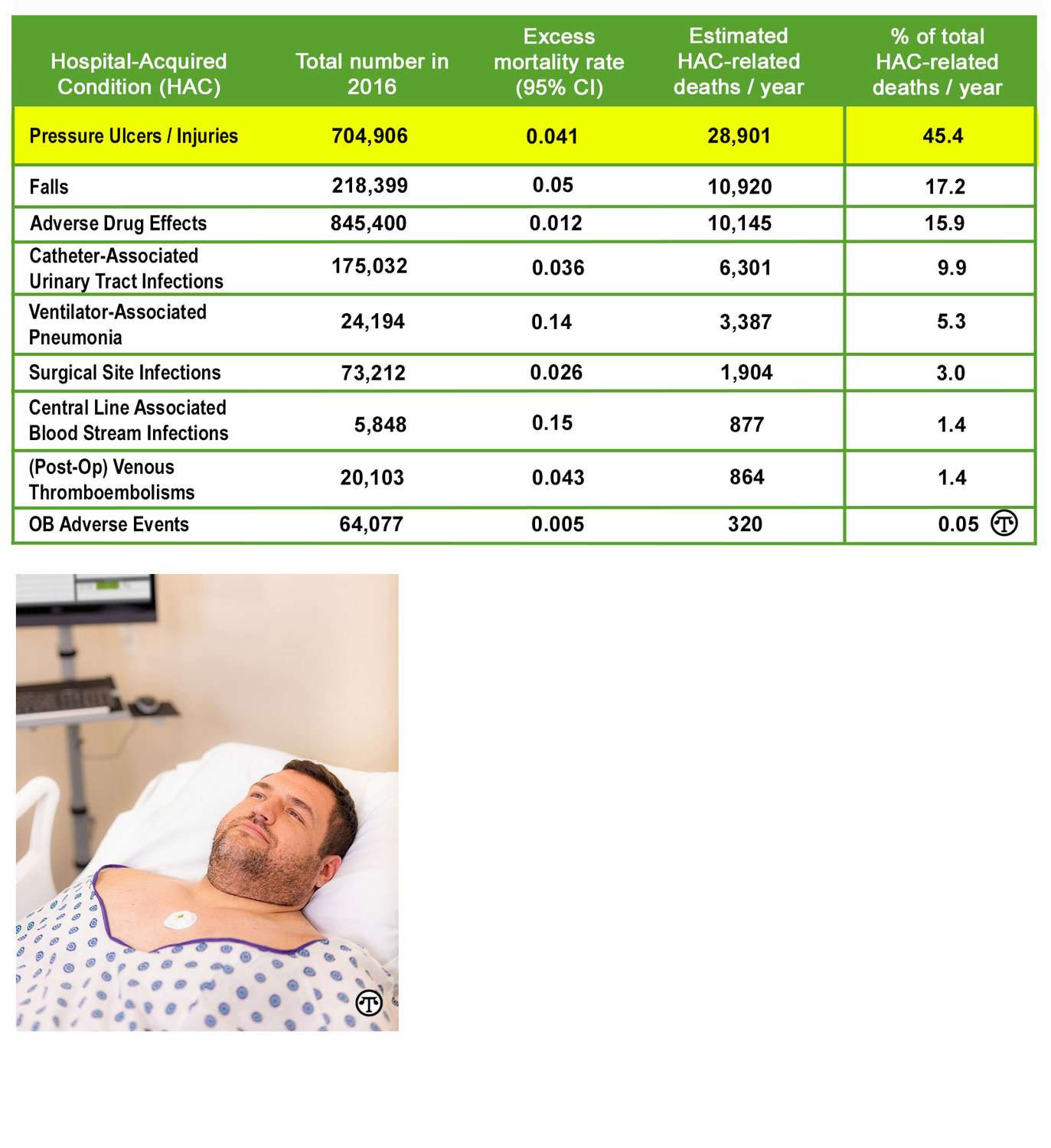
We calculate the CMS PSI 90 using Medicare Fee-for-service claims. The CMS PSI 90 measure includes:
- PSI 03 Pressure Ulcer Rate
- PSI 06 Iatrogenic Pneumothorax Rate
- PSI 08 In Hospital Fall with Hip Fracture Rate
- PSI 09 Perioperative Hemorrhage or Hematoma Rate
- PSI 10 Postoperative Acute Kidney Injury Requiring Dialysis Rate
- PSI 11 Postoperative Respiratory Failure Rate
- PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate
- PSI 13 Postoperative Sepsis Rate
- PSI 14 Postoperative Wound Dehiscence Rate
- PSI 15 Abdominopelvic Accidental Puncture/Laceration Rate
Centers for Disease Control and Prevention’s National Healthcare Safety Network healthcare-associated infection measures
We calculate the following HAI measures using data on infections taken from charts, reports, and other sources and reported to the National Healthcare Safety Network:
- Central Line-Associated Bloodstream Infection
- Catheter-Associated Urinary Tract Infection
- Surgical Site Infection
- Methicillin-resistant Staphylococcus aureus bacteremia
- Clostridium difficile Infection
Improvement As Puzzle Pieces
It is important to recognize that the path through the guide is not a single sequence of steps. Instead, the sections can be better viewed as interlocking pieces of a puzzle, for two reasons. The components of improvement are not linear and independent: one piece may depend on another and work will need to move back and forth between them. Just as people approach puzzles differently, with some starting with the outside border and others starting in the center, both strategies can end with a completed puzzle.
We represent this view of the guide as a puzzle with the image below. To orient readers as you move through the guide, we repeat this image at the beginning of each section with the content of the section highlighted. In addition, throughout the guide, we explicitly cross-reference subsections where assessments, decisions, or tools in one area will contribute to deliberations or actions in another.
Throughout this toolkit, additional helpful materials are identified as follows:
| Action and Resource Symbols |
|---|
|
Denotes a tool for this action in Tools and Resources |
|
Denotes a linked tool or other resource for this action |
|
Denotes practice insightsExamples were drawn from experiences at the participating medical centers, as well as from other organizations that the study team had knowledge of |
|
Denotes additional background material for those interested in pursuing this area in more detail |
Care Bundles And Risk Assessment
Although intervention studies to prevent HAPU development have been conducted in different clinical settings, most employed single interventions in comparison to standard care . However, multi-component interventions, or care bundles, with a risk assessment are more effective in preventing HAPU development . The Braden scale for predicting pressure sore risk , more commonly called the Braden scale , is the most widely used tool in hospitals to identify patients at high risk for HAPUs. The Braden scale is highly effective in assessing HAPU risk among patients in medical, surgical, and critical care settings , and is more accurate than the clinical judgement of nurses .
Care bundles combine evidence-based interventions, usually three to five components, to yield a significantly better outcome than when individually implemented . To maximize the clinical outcome, all the interventions must be performed collectively and implemented consistently . Most HAPU care bundles include a risk assessment, support surfaces, patient repositioning, mobilization, friction reduction, nutritional support and moisture management . Additional intervention strategies include unit-based wound care clinicians, health record monitoring, audit result feedback, staff education, computerized processes, and standardized clinical practices .
Read Also: What Is The Medicine For Ulcer
Statewide Rates Of Present
There were 2,401,269 adult discharges at 311 California hospitals in 2007 and 2,490,488 discharges in the same hospitals in 2009 . Considering all stages and locations , pressure ulcers were listed as present-on-admission for 56,531 discharges in 2007 and 74,684 discharges in 2009. Hospital-acquired pressure ulcers were listed for 6,705 discharges in 2007 and 6,654 discharges in 2009.
What If We Are Not Ready
You should not move ahead until you are confident of organizational readiness. You can use the checklist in section 1.7 below to assess each of the areas of organizational readiness for change that has been discussed in this section. To the extent that readiness is not yet evident, or is only partial, it is critical to take steps to address those areas. At a minimum, the facility must have one senior leader who understands the importance of this effort and is committed to supporting the effort both in terms of resources and necessary changes to work processes. In addition, evidence of a broader commitment to patient safety is an essential component. If any of these elements are missing, it is essential to build support and readiness before launching a full-scale change effort.
Some ways to build support and readiness may include:
You May Like: Can Ulcerative Colitis Lead To Crohn Disease
Hospital Acquired Ulcer Prevention Programs With Care Bundles
In a systematic review comparing intervention effectiveness for a HAPU clinical practice guideline, Qaseem et al. reported care bundles significantly improved skin care and reduced HAPU rates, with a cost savings of at least $3,000 per case. Similarly, Sullivan & Schoelles reported care bundles significantly reduced HAPU rates in 11 , with a mean reduction of 82% . For assessment within the care bundles, there was also no significant difference reported in diagnostic accuracy between the Braden, Cubbin and Jackson, and Norton and Waterlow scales .
The single randomized controlled trial was reported from Saudi Arabia . In this study researchers compared a care bundle with a training program for the intervention group to normal care for the control group. HAPU incidence was significantly reduced in the intervention group when compared to the control . There was also significantly less stage I/II pressure ulcers, with no stage III/IV, development for the intervention group. Differences in care processes were also observed for repositioning and health protector application . Furthermore, a retrospective observational cohort study found there was a longitudinal impact of payment policies on the quality improvement interventions to prevent HAPUs. In this regard, Padula et al. observed hospitals adopting bundled interventions had a 27% reduction in HAPUs . The bundled interventions were attributed to changes in reimbursement policy, resulting in a 100% reduction in HAPU cases .
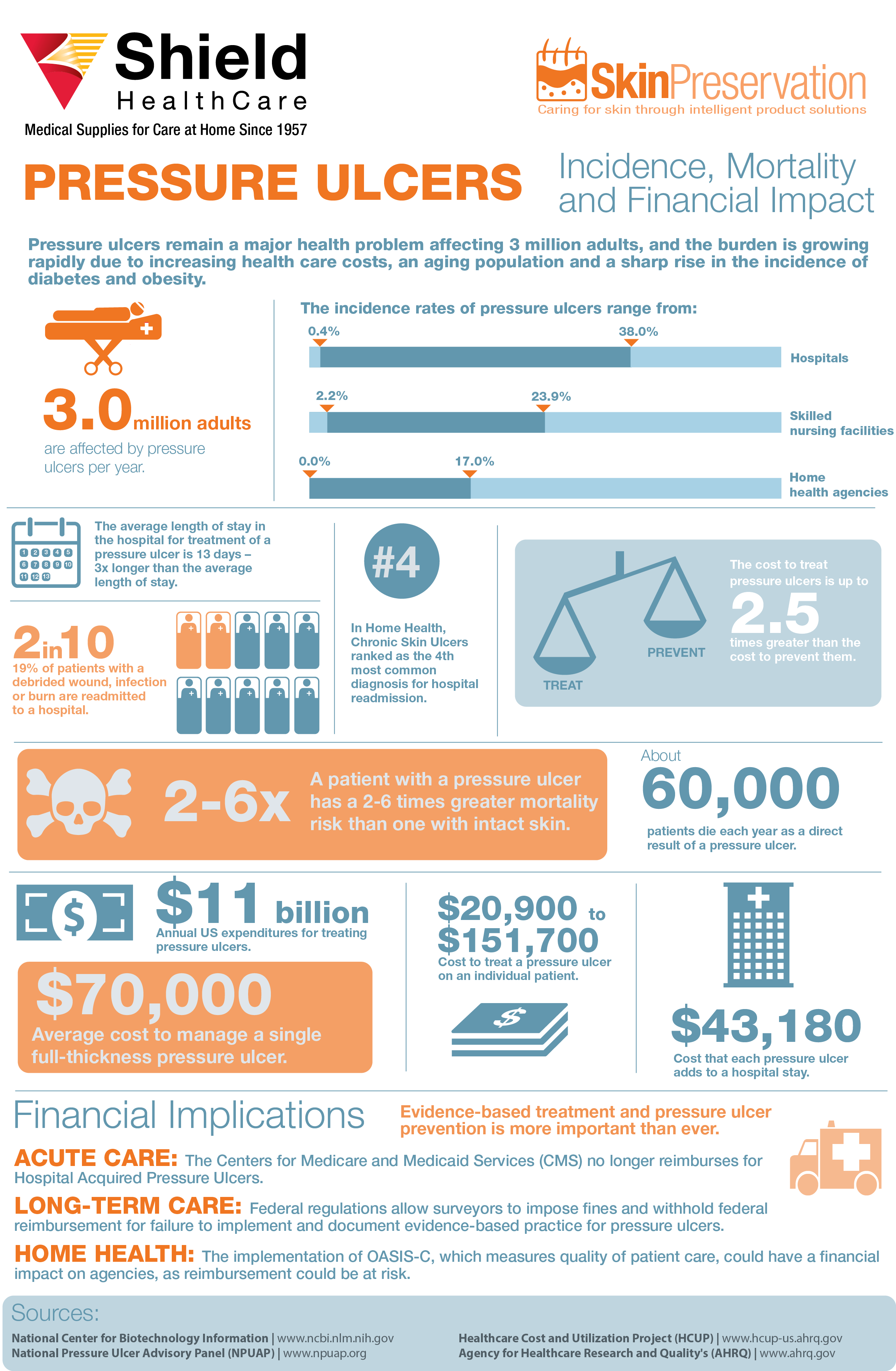
Implications Of Pressure Ulcers
Studies have revealed that pressure ulcers produce endless pain, restrict life activities and require a significant amount of coping on the part of the patient. The persistent pain is caused by the increase in pain that occurs as a result of moving , the pain associated with dressing changes and debridements, and the pain caused by alternating air mattresses. Pressure ulcers cause depression, anxiety, feelings of being burdensome, powerless, and inadequate. Wound odor affects the patient and others.
Pressure ulcers can cause significant emotional distress in patients. Pressure ulcers are associated with long lasting pain and suffering. The healing process can take months and involve elaborate surgical procedures such as flap creation, and impose a severe financial and social burden on families. The annual cost to treat pressure ulcers is 1.68 to 6.8 billion dollars. The cost of treating ulcers is well over twice the cost of preventing them. This does not even include the cost of litigation.
Don’t Miss: Can You Take Tylenol With Ulcerative Colitis
Contents Of The Daily Pu Report
The daily PU report includes: patient medical record number, name, unit , bed number, location of PU, POA documentation, and respiratory therapist documentation. This report consists of information from multiple areas of the medical record. The first, already mentioned, is the yes/no question does the patient have a PU which is part of the nurses assessment each shift. The other areas of the EMR that this report draws information from are: oral, skin, and neck assessments by respiratory therapists admission documentation and PU documentation forms. Drawing together documentation data from several different sources and different clinical disciplines allows more accurate capture and confirmation of PU presence throughout the EMR .
Sample of Daily Pressure Ulcer Report Used to Identify Patients. Data Are Representative of a Typical Daily Report
Who Will Take Ownership Of This Effort
Beyond the support of organizational leaders, improvement and change projects need strong advocates, members of the organization who are committed to the project’s goals and who can influence others to get involved. Successful change projects must have broader support than just one or two champions. These individuals would be from various disciplines and may include physicians, unit managers, wound care nurses, nutritionists, or staff members with a particular interest in this area. Some or all of these staff should make up the interdisciplinary Implementation Team that will guide the improvement effort, as described in section 2.
Action Steps
- Assess your organization to identify who the potential advocates of pressure ulcer prevention are likely to be. Some may be obvious, such as the Wound, Ostomy, and Continence Nurse , but others may not be immediately evident.
- Who cares about this issue? Why might it be important to them?
- Organizationally, what would be the logical home base for this effort?
- Are there individuals in that part of the organization who would be willing to take ownership?
Resources
Also Check: Can You Get Ulcers In Your Intestines
Data Collection And Analysis
After the sample was defined and the study quality evaluated, data from the included studies were abstracted into an Excel-based literature review matrix for analysis and synthesis. The data abstraction was completed by two reviewers and verified by a third. The quality of evidence was evaluated with the American Association of Critical-Care Nurses Levels of Evidence . Studies assessed within the first four evidence levels were included in the review, while level M studies were excluded. Studies assessed as the highest level of evidence, or level A, include a meta-analysis of multiple controlled studies or meta-synthesis of qualitative studies with results that consistently support a specific action, intervention, or treatment. The next level, or level B, describes well-designed controlled studies, both randomized and non-randomized, with results that consistently support a specific action, intervention, or treatment. Then, level C studies are qualitative, descriptive, correlational, integrative reviews, systematic reviews, or randomized controlled studies with inconsistent results. Next, level D studies include peer-reviewed professional organizational standards, with clinical studies to support recommendations. Finally, level M are manufacturer recommendations. This leveling facilitated study comparison to identify the strongest evidence for clinical practice .
What Are Hospital Acquired Pressure Injuries From Nippv Costing Your Hospital
The views and ideas presented in this blog article are solely those of the author, and the content is not intended to serve as medical advice. Vapotherm does not practice medicine or provide medical services. Practitioners should refer to the full indications for use and operating instructions of any products referenced herein before prescribing them.
Context
Hospital Acquired Pressure Injuries , also known as pressure ulcers, are often costly yet preventable events. To understand the impact of HAPI from noninvasive positive pressure ventilation on your organization and to develop effective strategies for pressure injury reduction, it is important to understand how a pressure injury is defined and classified, what stages of pressure injuries cannot be reimbursed, how these types of injuries occur, and their frequency.
Definition of a pressure injury
The NPUAP pressure injury staging system is the gold standard for classification of pressure injuries. The wound is numerically classified as Stage 1 or 2 or 3 or 4, based on the deepest tissue type exposed. The following definitions are taken from the NPUAP.
Stages of pressure injuries considered never events by CMS
Of note, Stage 2 injuries were found to be the majority of face mask ulcers in a study by Visscher et al, . This finding produces a heightened concern as Stage 2 device-related ulcers have a greater tendency to progress to Stage 3 and 4 compared with pressure ulcers caused by other factors.
HAPIs from NIPPV
| Type |
You May Like: Does Smoking Cause Ulcers After Gastric Bypass
What Is The Scoring Calculations Review And Correction Period For The Hac Reduction Program
The FY 2014 Inpatient Prospective Payment System/Long-Term Care Hospital Prospective Payment System Final Rule requires CMS to give hospitals confidential Hospital-Specific Reports. We give hospitals 30 days to review their HAC Reduction Program data, submit questions about the calculation of their results, and request corrections before public reporting.
The Scoring Calculations Review and Corrections period let hospitals request corrections to the following:
- CMS PSI 90 measure result
- Measure score for each measure in the program
- Total HAC Score
The Scoring Calculation Review and Corrections period does not let hospitals:
- Submit more corrections to the underlying CMS PSI 90 claims data
- Add new claims to the data extract we use to calculate the results
- Correct reported number of healthcareassociated infections
- Correct standardized infection ratios
- Correct reported central-line days, urinary catheter days, surgical procedures performed, or patient days
Does Senior Administrative Leadership Support This Initiative
It is crucial to make sure that your organization’s leadership team shares the urgency to change pressure ulcer practices and is willing and able to provide complete and ongoing support for this change effort. Lessons learned from key pressure ulcer prevention initiatives provide us with the evidence that support is needed from both the top-level administration as well as those at the bedside. Facilities that have already transitioned to a shared leadership model may be able to take a different approach through the channels that already exist for bottom-up input and leadership.
In a shared leadership model, the interdependence and expertise of staff at all levels is appreciated and staff are involved in key committees, developing the ability to analyze decisions from multiple perspectives. For other facilities that have a more traditional leadership structure and approach, the assessment and cultivation of senior leadership support will be a more crucial process.
Consider how support for this effort fits with other institutional values and commitments in order to frame it most effectively to obtain and maintain leadership attention. While you may not know at the outset all the kinds of support that will be needed, it is clear that the changes are going to require new or reallocated resources, most likely both human and material. The changes will also require focus and accountability for results, which will also need senior leadership oversight.
Tools
Action Steps
Tools
Also Check: How To Know If You Have A Peptic Ulcer
Hospital Liability And Bedsores
You may wonder how to sue hospitals for bedsores. After all, a hospital is a corporation and not a person. The medical staff is responsible for the neglect after all. Hospitals face liability for the actions and inaction of their employees, staff members and physicians by a legal theory called vicarious liability. If a hospital employee, a nurse or doctor fails to properly care for and treat a patient, and that patient develops a bedsore, the hospital is responsible and legally liable. If the sore worsens and causes other health issues or leads to the patients death, the hospital can also face liability for wrongful death.
Hospitals also make decisions about staffing. For several years, hospital staff and nurses have been waiving a red warning flag and speaking out about theirconcerns about understaffing. When hospitals are understaffed, its nurses and nursing assistants may not have adequate time to pay attention to patients who are immobile or unable to communicate or call for assistance, which may lead to less care and result in bedsores.
What Are The Different Stages Of Bedsores
At some time or another, a hospital patient may develop a stage 1 bedsore or pressure sore from not moving enough, or simply from sitting too long in one position, in bed or in a chair. You may see a red spot on the patients skin, and the area may feel swollen, warm or hard. In most cases, if pressure is removed from the area, the signs will clear up within a few days without needing additional medical care and treatment, outside of keeping the area clean and dry and maintaining a healthy diet. This is of course assuming that you do not repeat the behavior that caused the pressure sore to develop.
If a patients caregivers ignore the initial signs of a bedsore, if they fail to regularly turn and position a patient with limited mobility, this may lead to the development of a stage 2 bedsore. Stage 2 bedsores are characterized by blistering or abrasions on the skin where the original sore appeared.
In a hospital, if a caregiver fails to recognize the signs of this stage of a bedsore and fails to take action, the patient will likely develop other medical issues at this stage, and the wound will likely require additional medical care and treatment. Bedsores must remain clean and dry to avoid infection, and the wound may need to remain covered to avoid further irritation. Typically, the recovery for stage 2 bedsores varies from a few days to several weeks if adequately assessed and treated appropriately.
Recommended Reading: Best Cure For Mouth Ulcers
When Do We Adjust Payments Under The Hac Reduction Program
We adjust payments when we pay hospital claims. The payment reduction is for all Medicare fee-for-service discharges in the corresponding fiscal year. We let hospitals know whether their payment will be reduced in a HAC Reduction Program Hospital-Specific Report, which is delivered to hospitals from the Hospital Quality Reporting system Managed File Transfer inbox.
More information is available in the QualityNet HAC Reduction Program Scoring Methodology section.