Treating Crohns And Colitis
Its important to know that neither Crohns nor ulcerative colitis can be cured, though doctors will work with patients to manage symptoms. The two illnesses are generally treated with the same types of medication, although each patient may respond differently to the same drug. The goal of treatment is to reduce the inflammation, which in turn reduces symptoms, allows your body to repair damaged tissue, and helps slow the progression of the disease.
Today, many patients get a relatively new class of drugs, called biologics, which are live antibodies that are given to patients to help their immune cells fight the inflammation. Other classes of drugs include immunomodulators, which help tamp down the immune systems inflammatory response, and aminosalicylates, the oldest class of drugs, which are used to help keep the disease in remission. According to the Crohns and Colitis Foundation, immunomodulators can take up to six months to become fully effective, so doctors usually prescribe them along with fast-acting steroids that patients will ideally go off of once the immunomodulators reach their full potential. I absolutely think that with these new drugs, its a new era in the treatment of inflammatory bowel disease, says Dr. Cohen.
Is Colitis An Inflammatory Bowel Disease
Ulcerative colitis is an inflammatory bowel disease, but its causes are normally due to infections from bacteria, viruses, parasites, or fungus. The term colitis refers to the main symptom, which is diarrhea. Infectious colitis is often linked with food poisoning, which is an infection of the stomach and rectum.
Ulcerative Colitis Vs Diverticulitis: Us Prevalence
The CDC estimated that one to 1.3 million Americans are affected by IBD. Generally, ulcerative colitis is more prevalent in males than females.
Roughly two million people in the U.S. suffer from diverticular disease. Prevalence rate is one in 136, or 0.74 percent. Annually, 300,000 new cases of diverticular disease are diagnosed.
Recommended Reading: How Do You Know If You Have Ulcerative Colitis
What Is Crohns Disease
Crohns disease is a type of IBD where there is inflammation of the entire gastrointestinal tract, or parts of it, from mouth to anus. In addition, the entire thickness of the bowel wall is involved in Crohns disease, which can lead to some serious complications.
What are symptoms of Crohns disease?
The symptoms of Crohns disease depend on what parts of the GI tract are involved. Common symptoms include abdominal pain, weight loss, and diarrhea.
If the lower part of the GI tract such as the colon and the small intestines are involved, you might also experience:
-
Abdominal pain
What are complications of Crohns disease?
Crohns disease can lead to some serious complications, such as:
-
Fistulas, where a hole is formed between the intestines and other parts of the body such as the skin, bladder, or vagina
-
Abscesses, which are pockets of infection that may need surgery or a procedure to drain them
-
Strictures, which are a narrowing of the bowel that can lead to blockages
-
Cancers of the GI tract
Read Also: How Do They Check For Ulcers
Difference Between Colitis And Diverticulitis
Inflammatory illnesses of the colon include colitis and diverticulitis. Colitis is the inflammation of the colon. Diverticulitis is the inflammation of the colons diverticula. Both of these conditions are inflammatory. It falls into the group of digestive illnesses in general. To hasten the healing of the colon, it is occasionally necessary to start the patient on a steroid.
Also Check: Can You Take Imodium With Ulcerative Colitis
What Vegetables Should Be Avoided With Colitis
Cruciferous vegetables like broccoli and cauliflower contain insoluble fiber and have tough stalks. They may cause problems with gas and bloating. If gas is a problem for you during a flare, its best to avoid vegetables such as: broccoli.
- Watch Out For Fiber. Whole grain cereals and breads are difficult to digest and lead to flare ups if you have UC.
- Nuts And Seeds. These foods are difficult to digest and aggravate the symptoms.
- Dairy.
Antidepressants And The Management Of Ibs Symptoms In Uc
Tricyclic antidepressants and selective serotonin reuptake inhibitors are more effective than placebos in treating IBS. A systematic review of publications reporting the efficacy of antidepressant medications in the maintenance and induction of remission of IBD was published by Mikocka-Walus et al in 2006. The review included six case reports, one nonrandomized, open-label study, and one letter that, collectively, reported beneficial effects of bupropion, paroxetine, amitriptyline, and phenelzine. However, the studies were small, and all except one was conducted in patients with Crohns disease rather than UC.
We are aware of only one study reporting the efficacy of tricyclic antidepressants in UC patients with ongoing symptoms who had no objective evidence of disease activity. It is important to point out that patients in this retrospective study were not screened formally by using validated questionnaires to confirm whether or not they met symptom-based criteria for IBS. Outcomes, which were based on self-reported symptom severity by participants who were using a Likert scale, appeared to be good, with at least a moderate improvement in symptoms in 56% of UC patients. Symptom response among those with UC was similar to that observed in a control group of IBS patients.
You May Like: Can Ulcers In The Colon Be Cancerous
Can Ibs Cause Depression
Absolutely. Does IBS make you happy or sad? IBS can be very debilitating and therefore can cause people to be depressed. It used to be common to treat IBS with antidepressants . Unfortunately, this will rarely cure IBS and is not addressing the cause of the IBS. Many studies have documented a link between IBS and depression as well as anxiety, as described in the European Archives of Psychiatry and Clinical Neuroscience.
You May Like: Stomach Ulcer Blood In Stool
Crohns Disease Vs Diverticulitis: Us Prevalence
Prevalence of Crohns disease in the U.S. is 26 to 199 per 100,000 persons, and the incidence rate of Crohns disease is 3.1 to 14.6 cases per 100,000 person-years.
Roughly two million people in the U.S. suffer from diverticular disease. Prevalence rate is one in 136, or 0.74 percent. Annually, 300,000 new cases of diverticulitis are diagnosed.
Recommended Reading: How To Get Rid Of Tongue Ulcers
Difference Between Ulcerative Colitis And Diverticulitis Causes
As mentioned, the immune system is suspected to play a role in ulcerative colitis, along with genetics and environmental factors. Certain genes seem to be involved in the development of ulcerative colitis, and having more than four family members with this condition increases your risk of developing it, too. Environmental factors include place of residence, especially because there are higher rates of ulcerative colitis in urban areas, North America, and Western Europe. Air pollution, medications, and certain diets have also been found to be associated with a higher risk of ulcerative colitis.
Weak spots along the bottom of the large intestine can prompt the formation of diverticula. When pressure is added, bulges form. These bulges, or pouches, may protrude through the colon wall. When they burst or get infected, this marks the diagnosis of diverticulitis. It is worth noting that diverticula themselves do not necessarily create symptoms.
Diet Considerations For Colitis
Colitis can be caused by several different conditions and each condition might require additional consideration when planning a diet. People with inflammatory bowel disease and irritable bowel syndrome may have to monitor the amount of fiber they consume as it may cause gas and bloating. Since fiber is important to gastrointestinal health and should be a significant part of the stage three diet, you should speak with your physician concerning your level of fiber intake according to your disease. You may also need some supplementation if you are at risk for malnutrition your physician can help with this as well.
- Colitis can be caused by several different conditions and each condition might require additional consideration when planning a diet.
- You may also need some supplementation if you are at risk for malnutrition your physician can help with this as well.
Don’t Miss: Ulcerative Colitis And Renal Failure
Diagnostic Focus And Assessment
The laboratory tests performed on the first day of admission revealed leukocytosis with neutrophilia , thrombocytosis , anemia , elevated inflammatory biomarkers , and low serum urea levels . The abdominal ultrasound examination was normal. Lower digestive endoscopy pointed out multiple ulcerations, hemorrhage, and edema of the sigmoid colon , thus suggesting a possible IBD however multiple orifices raised the suspicion of a CD, which was afterwards confirmed through a barium enema.
Figure 1. Initial aspect of the colon at colonoscopy.
Histopathological examination of the colonic biopsy specimens showed active inflammation associated with architectural changes of the colonic mucosa and crypt abscesses, which highly suggested a chronic inflammatory process, most likely UC. By taking into account the macroscopic aspect of the colonic mucosa and the histopathological results correlated with the presence of colonic diverticula, we were able to establish the diagnosis of SCAD.
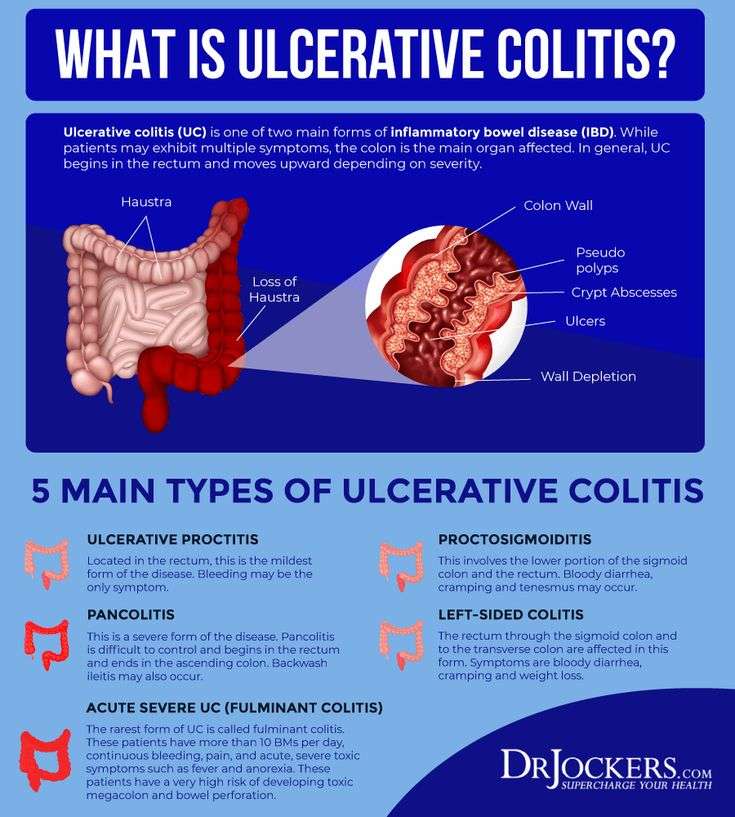
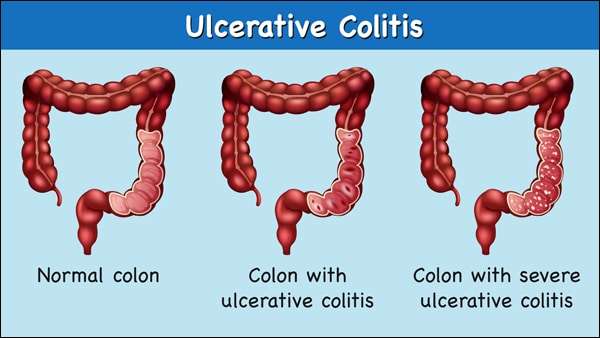
What Is Ulcerative Colitis
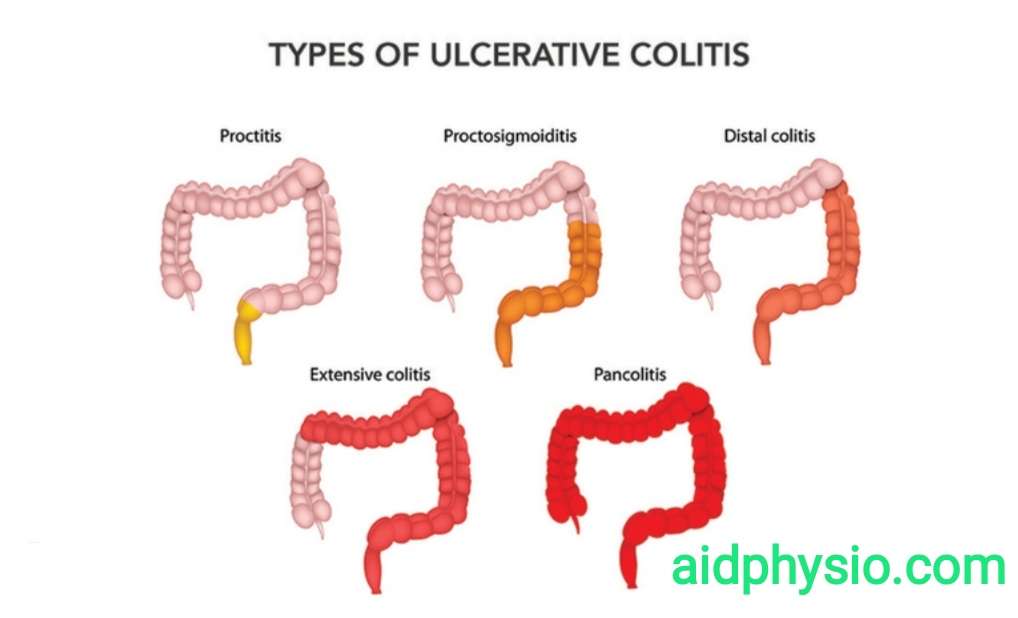
Defined as a chronic inflammation of the large intestine and rectum, ulcerative colitis is a type of inflammatory bowel disease which can also give rise to inflammation in joints, spine, skin, eyes, and the liver and bile ducts, if the severity increases with time. This inflammatory process can also give rise to multiple tiny sores and ulcers in the affected areas, causing bleeding and discharge of pus.
This condition can affect individuals of any age, but symptoms will mainly be visible around the age of 15-30 and 50-70.
Even though the exact etiology for ulcerative colitis is not known yet, stress, heredity, and weakened immune system are thought to be playing important roles in the pathophysiology. People who are under the treatment of Isotretinoin, which is used to treat cystic acne are also at a high risk of developing this condition.
Patients with ulcerative colitis will usually experience abdominal pain, increased abdominal sounds, stools mixed with blood, diarrhea, fever, rectal pain, weight loss and malnutrition. Sometimes, there can be associated features such as nausea, vomiting, joint swelling and pain, skin ulcers and mouth sores depending on the affected systems.
According to latest research studies, ulcerative colitis is known to increase the risk of colon cancer. Therefore, it is highly important to carry out a colonoscopy in order to exclude a possible risk.
You May Like: Remicade Dosing For Ulcerative Colitis
How Others Treat Me Because Of It
Its one thing to lose the pleasure of eating but to add insult to injury TPN has caused people to stop inviting me to events and I have had to miss out on things that I want to be a part of. Almost everything revolves around food and drinks. When friends get together they usually want to meet for dinner or go out for drinks. When you start dating someone its the same thing. Holidays revolve around food. Your mom and Grandma probably think that they arent loving you enough if you didnt eat 5 plates of food and then take some home with you when you visit them. I could go on and on! Its probably difficult for you to think of the last time you were invited somewhere and food wasnt involved.
You May Like: New Meds For Ulcerative Colitis
Diverticulitis & Colitis Diet
Fact Checked
Diet is an important part of the management of diverticulitis or colitis 1. In diverticular disease, small pockets or pouches form in the wall of the colon when these pouches get inflamed, the condition is called diverticulitis. Colitis is an inflammation of the large intestine this can be caused by irritable bowel disease, an inflammatory bowel disease like Crohn’s, or infections. When you have either of these conditions, you have to make some changes in your diet during the flare-ups to aid in your recovery.
Don’t Miss: Best Ulcerative Colitis Diet Book
Are There Ibd Or Ibs Diets
There is no special recommended diet to treat IBD, but some people may respond to dietary changes such as eating smaller and more frequent meals, taking nutritional supplements, and avoiding certain foods, for example, fatty and fried foods, meats, spicy foods, and fiber-rich foods. People with Crohns disease may have difficulty tolerating dairy products because of lactose intolerance.
Patients with IBS may respond to dietary changes. Low fat, high carbohydrate, and low FODMAP foods may help ease symptoms. Fiber can be helpful in some people.
Read Also: Remicade Infusion For Ulcerative Colitis
Whats New In Treating Ulcerative Colitis And Diverticulitis
New paradigms and new management in treating these diseases
OUR UNDERSTANDING of ulcerative colitis and diverticulitis is changing, according to Jonathan Terdiman, MD, who directs the gastroenterology department at University of California, San Francisco. Dr. Terdiman, who spoke at UCSFs management of the hospitalized patient conference last fall, pointed out new developments in treating those conditions, as well as common mistakes clinicians make.
Physicians often dont recognize soon enough, for instance, when ulcerative colitis patients are failing steroids. Doctors also need to change how they dose infliximab in those patients.
Even more far-reaching: Experts are now developing a new way of thinking about diverticular disease, seeing it as more of an immune disorder than an infection. That new paradigm, Dr. Terdiman explained, could broadly affect treatment and management.
An ulcerative colitis diagnosisUlcerative colitis, which ranges from mild to fulminant, comes with many predictors of bad outcome. By bad outcome, we mean people who end up leaving the hospital without their colons, Dr. Terdiman said.
Infliximab is not just an induction drug but a maintenance drug.
~ Jonathan Terdiman, MDUniversity of California, San Francisco
Those predictors include stool frequency , percentage of bloody stools, a fever of more than 37.5 degrees, a heart rate over 90 beats per minute, and a CRP greater than 25.
Read Also: How Long Does A Ulcerative Colitis Flare Up Last
Diagnosis For Crohns Disease And Diverticulitis
Crohns disease is diagnosed through a detailed examination of ones medical and family history, as well as additional testing as needed.
Because Crohns disease can mimic other conditions like infections, diverticulitis, and cancer, its important to rule them out. Blood tests are ineffective in diagnosing Crohns disease, so an ultrasound, CT scan, MRI, colonoscopy, and internal biopsy may be conducted.
To properly diagnose diverticulitis, your doctor will conduct a physical examination, checking your abdomen and pelvic region. Other tests include blood tests, pregnancy test for women, liver function tests, stool tests, and CT scans, which can help gauge severity of diverticulitis.
When Surgery Is Needed
If medication isn’t reducing the inflammation and IBD progresses, surgery may be needed. This is where people with ulcerative colitis tend to fare better.
If the colon gets bad enough in ulcerative colitis, its removed and replaced with an internal pouch, which functions like a colon, says Cohen. According to the Mayo Clinic, colectomy surgery whether partial or full usually requires additional procedures that reconnect the remaining portions of the digestive system so they can still rid the body of waste.
However, things are looking up. A study published in December 2019 in the Journal of Gastrointestinal Surgery found that due to advances in medicine and medical care for IBD patients over the past decade, the number of hospitalized patients with ulcerative colitis who require a colectomy decreased by nearly 50 percent between 2007 and 2016.
According to the Crohns and Colitis Foundation, proctocolectomy with ileal pouchanal anastomosis usually called J-pouch surgery is the most common surgery performed on people with UC who have not responded to medication. Surgeons remove the rectum and colon and then create a temporary opening in the abdomen, called a loop ileostomy, which will allow waste to move from the small intestine into an ostomy bag that sits outside the body while the digestive system heals from the surgery. In some cases a stoma, or permanent opening in the abdomen that funnels waste into an external bag, is required, notes the Mayo Clinic.
Recommended Reading: Indian Diet For Ulcerative Colitis
Summary Diverticulitis Vs Ulcerative Colitis
Diverticulitis is the inflammation of the diverticula arising from the colon whereas ulcerative colitis is the inflammation of the colon with the formation of associated ulcers. In the ulcerative colitis the colonic mucosa gets inflamed, but in diverticulitis, the diverticula that originate from the colon are the structures that get inflamed. This is the difference between diverticulitis and ulcerative colitis.
Are Ibs And Diverticulitis Related
People with one may also have the other, but technically are not directly related. However, the symptoms can be very similar, as discussed by Dr. Spiller in the medical journal Digestive Diseases. Diverticulitis is a type of inflammation in the colon. Sometimes doctors misdiagnose a patient with diverticulitis when they may actually have IBS, or they may also have IBS. These two conditions are sometimes difficult to differentiate. Learn more about IBS and diverticulitis.
Don’t Miss: What Causes Mouth Ulcers On Gums
Ibd Mimics: Most Common Conditions Misdiagnosed As Ibd
Since there is no single, gold standard diagnostic test for inflammatory bowel disease there are many disease processes that can be misdiagnosed as IBD, given its often non-specific symptoms. There is a broad differential diagnosis when considering IBD, however most of the etiologies generally fall into two categories: infectious and non-infectious. Some of these disease states affect a portion of the gastrointestinal tract which may help differentiate them from IBD and one another. First, we will review the non-infectious etiologies which include autoimmune disorders, vasculidities, ischemia, diverticular disease, drugs, cancer, and radiation-induced disease. It is important to note that while many of the etiologies discussed have histologic changes in colon biopsies in order to diagnosis IBD features of chronicity are warranted.
Non-infectious Mimics
Hermansky-Pudlak syndrome is a rare autosomal recessive condition where patients have oculocutaneous albinism, bleeding diathesis and other organ specific involvement including granulomatous colitis which can have features like CD. Patients with this condition who manifest GI disease usually have abdominal pain, fever, bloody stool and weight loss.6 The colon is most commonly affected, but like CD, may affect any part of the GI tract.
Infectious Mimics