There Are Various Causes Of Colitis And Each Has Different Treatments
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
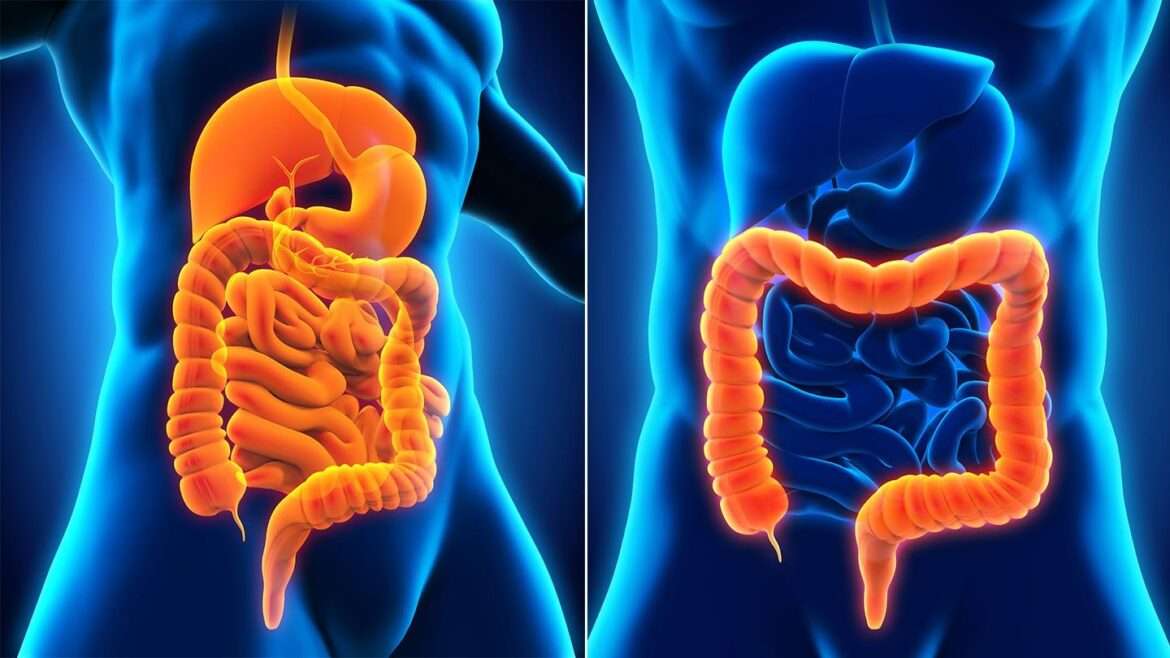
Colitis, which is inflammation in the large intestine, is a symptom of a disease or condition. It can be caused either by conditions that are chronic or those that come on suddenly .
Some of the causes of colitis include inflammatory bowel disease , microscopic colitis, ischemic colitis, pseudomembranous colitis , and allergic colitis.
Treating colitis will mean dealing with the underlying condition thats causing it. Because the causes are so different, there is no one treatment that will be used for every type of colitis.
This article will discuss how each type of colitis is treated. In most cases, treatments will include medications and/or changes to diet. For some conditions, certain types of surgery might also be used.
Watch What You Eat And Drink
You may have heard about diets for people with ulcerative colitis. There’s no evidence that certain foods can cause UC, cure it, or set off a flare. But if you’re having a flare, what you eat and drink can make symptoms worse:
- Fried or greasy foods can cause diarrhea and gas.
- Foods like beans, cabbage, and broccoli are likely to give you gas.
- Dairy products can cause gas, diarrhea, and cramps if you’re lactose intolerant.
- High-fiber foods, like raw fruits and vegetables, and whole grains, can make you have to poop more often. Don’t skip fruits and veggies, though. You can steam, bake, roast, or grill them instead of eating them raw.
- Carbonated drinks like soda can give you gas.
- Alcohol and caffeine can cause diarrhea.
When you’re having a flare:
- Eat smaller meals eaten more often. It may be easier on your system.
- Drink plenty of water. Diarrhea that comes with UC can make you dehydrated.
- Avoid or cut back on dairy, alcohol, and caffeine.
- Stay away from high-fiber snacks like nuts, seeds, corn, and popcorn. Then see if your symptoms improve.
UC can make it hard to eat normally, so you may lose weight. Your body also may not be able to absorb the nutrients you need.
Talk to your doctor to see if they recommend you take supplements. You could think about seeing a nutritionist, too. They can come up with an eating plan that works for you.
You can also use these tips to make an ulcerative colitis diet plan.
Uc Treatment Options At A Glance
The most commonly used treatments for UC:
These drugs, given orally or rectally, are anti-inflammatory compounds that contain 5-aminosalicylic acid . They decrease inflammation at the wall of the intestine. Examples of 5-ASAs include sulfasalazine, balsalazide, mesalamine, and olsalazine.
Metronidazole, ciprofloxacin, and other antibiotics may be used when infections occur, or to treat complications of ulcerative colitis.
Biologics for UC are designed to suppress the immune system to reduce inflammation. Certain biologics work by targeting specific inflammatory proteins called cytokines that play a role in inflammation. Others work by preventing certain white blood cells from getting into inflamed tissues.
Prednisone, prednisolone, and budesonide are included in this type of medication. They affect the bodys ability to initiate and maintain an inflammatory processkeeping the immune system in check. While effective for short-term flare-ups, theyre not recommended for long-term use.
These modify the bodys immune system activity to stop it from causing ongoing inflammation These drugs are usually used for people who have responded only to steroids.
You May Like: What Foods Should Be Avoided With Stomach Ulcers
Ulcerative Colitis Treatment Options You Should Be Aware Of
Ulcerative colitis can be unpredictable, which can make it challenging for physicians to determine whether a particular course of treatment has been effective. The main goal of treatment in UC is to reduce the signs and symptoms of ulcerative colitis by regulating the immune system, and to bring about long-term remission. While there is no cure for UC, treatment can help control symptoms so that patients can lead a fuller life. Treatment may include over-the-counter as well as prescription medications, lifestyle changes in stress management, diet and nutrition, and surgery.
Prescription medications typically include anti-inflammatory drugs, immune suppressants, and steroids. If these are not effective, -alpha inhibitors, or biologics, drugs typically given to treat certain types of arthritis, may be used.
Radiation Colitis And Enteritis
Inflammation of both the colon and the small intestine can be caused by radiation exposure, most commonly from cancer radiation therapy. However, medical procedures such as X-rays or CT scans can also irritate the colon tissues. Radiation colitis is usually temporary and is marked by diarrhea, cramping, nausea, and vomiting. Symptoms are temporary and usually fade in a few weeks. However, chronic radiation colitis can occur months to years following radiation therapy due to radiation damage. It is a progressive and serious complication of radiation therapy.
Also Check: Can I Take Imodium If I Have Ulcerative Colitis
Other Prescription And Over
Other medications may also be prescribed for targeting morespecific symptoms of colitis. For example, anti-diarrheals and pain medicationsmay be used to provide immediate relief until there is a more significantremission in symptoms. Often these medications can be purchased over-the-counter.Ulcerative colitis is also associated with an increased risk of infection thatmay need to be treated with antibiotics. Other nutritional supplements may berecommended by a healthcare provider to help the body naturally fightinflammation and maintain good overall health.
What If Proctitis Is Not Treated
Proctitis that is not treated or does not respond to treatment may lead to complications, including
- Severe bleeding and anemiaa condition in which red blood cells are fewer or smaller than normal, which means less oxygen is carried to the bodys cells
- Abscessespainful, swollen, pus-filled areas caused by infection
- Ulcers on the intestinal lining
- Fistulasabnormal connections between two parts inside the body
People with proctitis symptoms need medical attention. If diagnosed with proctitis, patients should take all medications as prescribed and see their doctor for a followup appointment to be sure the cause of the inflammation has been treated successfully.
Don’t Miss: Is Ginger Tea Good For Ulcerative Colitis
Blood And Stool Tests
Infections are the most common cause of colitis, so blood and stool tests are used to rule out microbes as the primary cause. Levels of certain substances in the blood could help identify other forms of colitis such as ischemic colitis, Crohn disease, ulcerative colitis, or microscopic colitis. The sedimentation rate of red blood cells helps to identify inflammatory conditions, such as active ulcerative colitis or Crohns disease.
Treating Uc Symptoms At The Source
To get ahead of UC symptoms, first you have to know whats behind them. UC symptoms are linked to excess inflammation that causes damage to your colon lining.
Controlling inflammation over time can help reduce UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain. Controlling inflammation can also help repair the colon lining.
Controlling inflammation to help repair your colon lining and improve your symptoms is a goal of UC treatment.
UC treatments are designed to control the excess inflammation in your colon. When inflammation is suppressed, it can help relieve common UC symptoms, achieve and maintain remission, and also help heal the tissue in your colon lining.
While many UC treatments are designed to control excess inflammation, some treatments work in different ways than others. You and your doctor should discuss all treatment options and considerations to find the one that may be right for you.
What is remission?
When your UC is in remission, it means you are experiencing no symptoms. If you think about all the ways UC symptoms may be impacting your life, its easy to see why achieving and maintaining remission is so important.
Read Also: Ulcerative Colitis Lower Back Pain
Check In Check Up: Ulcerative Colitis
You dont have to settle for good enough ulcerative colitis care. Take this series of assessments to evaluate how well your treatment is working.
Prednisone, hydrocortisone, and methylprednisolone work by suppressing the entire immune system, rather than targeting inflammation.
Because of their high risk of side effects, these three drugs are typically reserved for moderate to severe ulcerative colitis. They also shouldnt be taken for very long.
Budesonide , on the other hand, is considered a first-line treatment for ulcerative colitis. Budesonide can be taken orally as a tablet or capsule, or rectally, as a foam or tablet or in an enema. Because of the way the body processes budesonide, the oral form causes fewer side effects than other corticosteroids, according to a paper published in August 2016 in Expert Opinion on Pharmacotherapy.
If you take corticosteroids orally or by injection, you may have significant side effects. Local steroids which are applied just to the area that needs treatment are generally the preferred option.
For severe flares of ulcerative colitis, hospitalization and high-dose intravenous corticosteroids are often required. Once remission is achieved, your dose of steroids will be tapered gradually and ultimately stopped. Steroids cant be stopped suddenly because they cause the body to reduce production of the natural steroid cortisol.
Steroids are ineffective as maintenance therapy to keep ulcerative colitis in remission.
What Is A Fecal Transplant Procedure
A fecal transplant involves collecting stool specimens from one or more individuals and transplanting them into another persons gut. The aim is to recreate a diverse microbiota environment consisting of bacteria and other gut organisms from healthy donors.
The procedure uses various methods of transplantation. One technique involves creating a liquid slurry from donor stools and passing it through a nasoduodenal tube a tube that enters the nose and goes down into the small intestine, bypassing the stomach or, more commonly, using a colonoscopy.
Don’t Miss: Mouth Ulcer Vitamin B Complex
Work With Your Doctor To Understand Uc Severity
Its important for you and your doctor to understand how severe your symptoms are. Beyond that, tests and procedures may be done to evaluate your disease activity and get an even better understanding of whats really happening inside your bodyand the inflammation thats occurringgetting you to the treatment plan thats right for you.
Allergic Colitis In Infants
In some cases, this type of colitis is thought to be related to a food allergy. For breastfed infants, it might be recommended that the breastfeeding parent take certain foods that commonly cause allergies out of their diet.
In some cases, this may mean first stopping foods containing dairy. Other foods that cause common food allergies might be stopped as well if the colitis doesnt improve.
Recommended Reading: What Is The Best Thing To Put On Leg Ulcers
How Is Proctitis Diagnosed
To diagnose proctitis, a health care provider will take a complete medical history and do a physical exam. The health care provider will ask the patient about symptoms, current and past medical conditions, family history, and sexual behavior that increases the risk of STD-induced proctitis. The physical exam will include an assessment of the patients vital signs, an abdominal exam, and a rectal exam.
Based on the patients physical exam, symptoms, and other medical information, the doctor will decide which lab tests and diagnostic tests are needed. Lab tests may include blood tests such as a complete blood count to evaluate for blood loss or infection, stool tests to isolate and identify bacteria that may cause disease, and an STD screening. The doctor also may use one of the following diagnostic tests:
For either test, the person will lie on a table while the doctor inserts a flexible tube into the anus. A small camera on the tube sends a video image of the intestinal lining to a computer screen. The doctor can see inflammation, bleeding, or ulcers on the colon wall. The doctor may also perform a biopsy by snipping a bit of tissue from the intestinal lining. The person will not feel the biopsy. The doctor will look at the tissue with a microscope to confirm the diagnosis. In most cases, a light sedative, and possibly pain medication, helps people relax during a colonoscopy.
What Happens If You Don’t Treat Colitis
Colitis is usually a temporary condition that resolves on its own in a few days to a week. It can, however, be a sign of a more serious condition such as ulcerative colitis, Crohns disease, autoimmune disorders, metabolic disorders, circulation problems, heart problems, or radiation injury. It can also be a sign of a serious infection, such as a potentially fatal E. coli gut infection or amoebic dysentery. If the symptoms become severe or last longer than a week, its time to talk to a doctor.
Don’t Miss: What To Do For Leg Ulcers
How Can I Treat Colitis At Home
The primary goal of treating colitis at home is to replace fluids and electrolytes lost because of diarrhea. Drink fluids throughout the day and include electrolyte-rich foods such as broths or soups. If the colitis is caused by an infection, get plenty of rest to help the body carry on the fight against the pathogen.
Work With Your Doctor
You’ll need to see your UC doctor regularly. It may be every 6 months while you’re in remission. You’ll have routine procedures like colonoscopies and bloodwork to check on your UC.
If you’re having a flare-up, make sure to check in with your doctor. UC isn’t the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Can’t keep liquids down
When you have a flare, you can ask your doctor questions like these:
- Is UC causing my symptoms, or could they be due to another condition?
- Do I need to take any tests? If so, how often will I need to get them?
- Will you need to change the dose or type of my medication?
- If I need to take a new medication, what side effects could it cause?
- Should I make any lifestyle changes?
- When should I come back for another appointment?
Don’t Miss: Best Dog Food For Dogs With Stomach Ulcers
Related Resources For Colitis
* Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price.
Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
This article is not medical advice. It is intended for general informational purposes and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
How Long Will My Microscopic Colitis Flare Up Last
Its different for everyone, but flare-ups typically last for days to weeks. Many people find that they can reduce the length and severity of their flare ups by avoiding certain triggers, such as specific foods or chemicals, and medicating when necessary. Talk to your healthcare provider when your colitis is flaring.
Don’t Miss: Can I Die From Ulcerative Colitis
What Is The Best Probiotic To Take For Microscopic Colitis
Probiotics were previously recommended to help treat microscopic colitis, but current guidelines don’t recommend them. More research is needed before specific probiotics can be recommended.
A note from Cleveland Clinic
Microscopic colitis is still not well understood. Of all the inflammatory bowel diseases, its been the least often recognized or diagnosed, though scientists now suspect it may be just as common as the others. Its also had the least targeted research, and there’s currently no targeted medication for it. Fortunately, the treatments we have often work to control it. It may take some trial and error, but the right combination of medication and diet can help you manage your symptoms when they occur.
How Serious Is Microscopic Colitis

Its not as severe as other types of IBD, and not considered a life-threatening disease. Severe, unrelenting diarrhea could lead to dehydration, weight loss or even malnutrition, but microscopic colitis usually doesnt manifest this way. It tends to come and go, and it can be controlled with medication. It can affect your quality of life, however, with uncomfortable symptoms haunting your every meal.
Recommended Reading: What Is The Best Probiotic To Take For Ulcerative Colitis
What Is The Best Medication For Colitis
Medicines that directly treat colitis either reduce diarrhea, reduce swelling, or partly shut down the immune system. There is no best medication for colitis, just drugs that are the most appropriate for the patients medical situation and tolerance for side effects.
Add table classes to older pages
| Best medications for colitis | |
|---|---|
| Given in weeks zeor, two, and six and then every eight weeks. Dose depends on weight | Infections, headache, abdominal pain |
The standard dosages above are from the U.S. Food and Drug Administration and the National Institute of Health . Dosage is determined by your doctor based on your medical condition, response to treatment, age, and weight. Other possible side effects exist. This is not a complete list.
Drugs That Target Inflammation
Most people with UC take prescription drugs called aminosalicylates that tame inflammation in the gut. These include balsalazide , mesalamine , olsalazine , and sulfasalazine . Which one you take, and whether it is taken by mouth or as an enema or suppository, depend on the area of your colon that’s affected. As long as you avoid your triggers, these may be enough if your disease is mild to moderate.
You may need something else if your condition is more severe or if those standard treatments stop working. Your doctor may consider other medicines. Some people may also need surgery.
Read Also: Vegan Protein Powder For Ulcerative Colitis