How To Treat Symptoms
In a given year, 70 percent of people with active disease will have another episode the following year. But only 30 percent of people in remission will have active disease the next year.
Basically, the longer youre in remission, the less likely you are to have a flare-up the next year. And that means less diarrhea. Thats why its so important to find a treatment plan that works for you.
Medications to control UC symptoms include:
- aminosalicylates
- immune modifiers
There are also medications to help with diarrhea. Antidiarrheal agents help slow movement through the intestines, which helps your body absorb the fluids and nutrients you need. These include:
Fiber supplements may also be helpful in reducing diarrhea, but avoid them if youre in the middle of a flare-up. Check with your doctor if youre not sure whether these supplements are suitable for you.
Its also important to speak with your doctor under the following conditions:
- Before adding any over-the-counter treatments or dietary supplements to your regimen. Some have the potential to interfere with the medications youre currently taking.
There are a few ways to help manage urgent or frequent bowel movements. For example, you can set regular times to move your bowels. Choose times that are convenient, so youre not rushed.
Some items that can contribute to loose stools are:
Is This My Fault
No. Scientists dont really know why your immune system starts to go haywire and inflames your bowel in ulcerative colitis. What seems fairly clear, though, is that it has little to do with what youve done in the past. You didnt catch UC from some infected person or from eating or drinking the wrong thing. Nor did you get it from simply being stressed out.
That said, both hard-to-digest foods and stressful situations can trigger or worsen a flare-up of UC symptoms, if you already have the disease. You can often improve your symptoms if you avoid certain high-fiber foods like uncooked veggies, nuts and seeds, as well as fatty or greasy foods like burgers and fries. Use common sense. If you find that certain foods upset your stomach, try to stay away from them.
It can also help to maintain balanced mental health and avoid unnecessary stress and anxiety. Proper sleep, quitting smoking, and regular exercise could also keep flare-ups at bay.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Don’t Miss: How Serious Is A Stomach Ulcer
Ischemic Causes Of Colitis
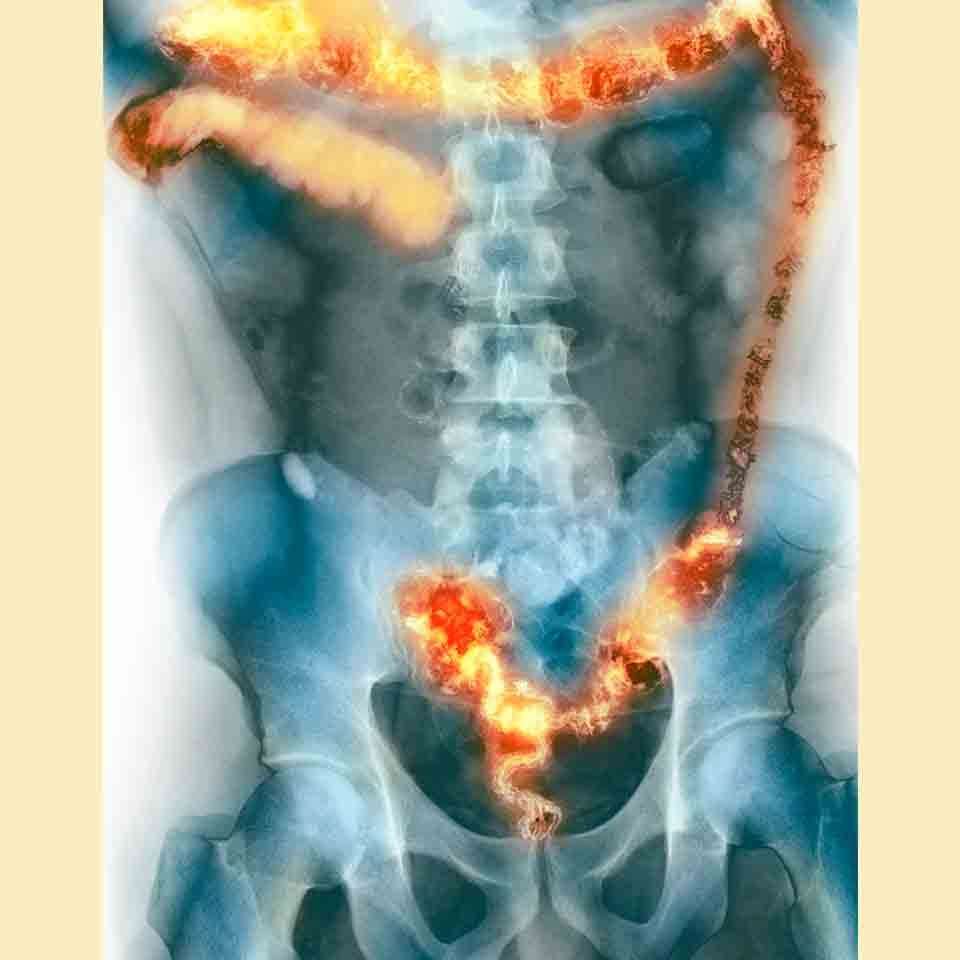
The colon can be thought of as a hollow muscle. It requires a normal blood supply to deliver oxygen and nutrients for the muscle to function normally. When the colon loses its supply of blood and becomes ischemic , it may become inflamed. Ischemia or lack of blood supply causes inflammation of the colon leading to pain, fever, and diarrhea .
- As a person ages, the arteries that supply blood to the colon gradually narrow and can cause ischemic colitis. Risk factors for narrowed arteries are the same as atheroscleroticheart disease, stroke, and peripheral artery disease . These include diabetes, high blood pressure, high cholesterol, and smoking.
Read Also: How Would You Know If You Had A Bleeding Ulcer
How Can Sulphur Cause Harm
Bacteria that live in the bowel convert the sulphur in food into hydrogen sulphide, in a process known as fermentation. This highly toxic product is responsible for the foul odour associated with passing gas, can cause abdominal pain, and frequent, urgent trips to the toilet. Normally, the cells lining the colon absorb and detoxify the gas but in people with ulcerative colitis, there is a two-fold problem. Firstly, ulcerative colitis patients appear to produce more hydrogen sulphide than normal, and they have a more difficult time breaking down the gas . The extra gas present may further damage the lining of the colon.
Hydrogen sulphide may have a number of adverse effects on the bowel and may contribute to the pathogenesis of ulcerative colitis. Hydrogen sulphide has been shown to increase the epithelial permeability and barrier function. In other words, it reduces the protective function of the cells lining the bowel. Other animal studies indicate high concentrations of the product can produce cell death, goblet cell loss, crypt architectural distortion, and superficial mucosal ulceration. It has also been shown to reduce the effectiveness of the immune system in trapping and killing unwanted bacteria. All of these examples point to the possible toxic effects of hydrogen sulphide on the cells lining the colon.
Also Check: Wound Care For Venous Leg Ulcers
Follow Up With Your Doctor
You may only need at-home or short-term care for some kinds of colitis. But UC is a condition youâll have for the rest of your life. And it affects everyone in a different way. Youâll need to work with your doctor to find a treatment plan that works for you.
No matter whatâs causing your symptoms, get medical care right away if you have:
- Watery diarrhea for more than a few days
- Heavy, ongoing diarrhea
Dont Miss: Psc Liver Disease Ulcerative Colitis
Altered Gut Microbiome And Its Impact On The Gutbrain Axis
Our current strategies of microbial manipulation include antimicrobials, fecal bacteriotherapy, and probiotics. Antimicrobials have questions around their safety, specificity, and durability . A systematic review of randomized control studies of probiotics found only support for a single formulation in a narrow indication of preventing UC relapse. However, this formulation as originally studied no longer exists under that trade name, but has been rebranded as Visibiome . At this point, there are microbial changes associated with disease activity and fatigue, but currently no narrowly targeted strategy exists to manipulate the microbiome to manage fatigue.
Recommended Reading: Cure For Chronic Fatigue Syndrome 2017
Don’t Miss: What Causes Venous Stasis Ulcers
Symptom No : Abdominal Cramps
Solution: Try to pinpoint your triggers. Stomach cramps are often caused by gas or spasms in the gut. Common culprits include foods high in fiber or fat, which can impact gas production, says , an assistant professor of medicine at the University of Minnesota Medical School in Minneapolis and director of their inflammatory bowel disease program. Foods that are high in insoluble fiber especially cruciferous vegetables, such as broccoli and cauliflower can be particularly hard to digest, according to the Crohns & Colitis Foundation.
Medications, such as a recent course of antibiotics or nonsteroidal anti-inflammatory medications ibuprofen, naproxen, aspirin can also trigger abdominal pain, he says.
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Response to treatment
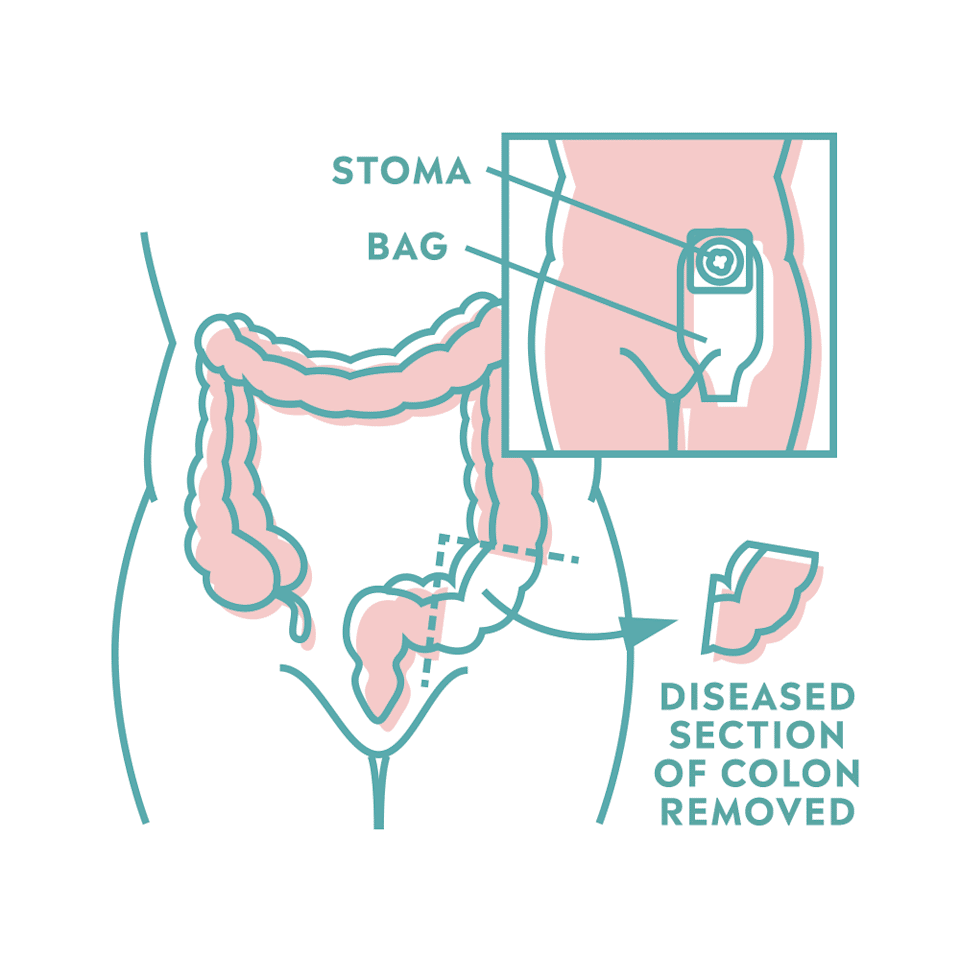
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Also Check: Crohn’s Disease Is Chronic Inflammation And Ulceration Of The
Signs Of Possible Colitis
General signs of colitis can include:
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Read Also: Good Foods To Eat With Stomach Ulcer
What Diet Is Best For Ulcerative Colitis
There is no specific diet or meal plan for ulcerative colitis , according to the U.K.s National Health Service . Some people may find that certain foods trigger symptoms or make them worse.
You may find that consuming a diet low in fiber during a UC flare may help ease your symptoms. Foods you can consume as part of a low fiber eating plan include:
Other meal plan tips for UC include:
- eating smaller meals more frequently rather than fewer larger meals
- drinking plenty of fluids
- taking food supplements at your doctors advice
- avoiding caffeine and alcohol, which can make diarrhea worse
- avoiding fizzy drinks, which can cause gas
- keeping a food diary to monitor which foods may be triggering your symptoms
Contact your doctor before making any significant changes to your eating habits. Your doctor may refer you to a dietitian or nutritionist to help make sure you get all of the nutrients you need while managing your symptoms.
Recommended Reading: Garlic Powder And Ulcerative Colitis
Your Priorities May Change
Facing chronic health challenges tends to make you realize what you value most. I know where I want to put my energy and whats worth it and whats not, Skomski says.
Getting diagnosed shifted Sams approach to her health in a similar way. I tend to be a very intense person and kind of a workaholic, she says. Being diagnosed with ulcerative colitis completely changed my priorities for life. I was always a health-conscious person, but now health is absolutely my number one priority. I am no longer willing to sacrifice my health for something else, like a job or even a passion.
It also affected her long-term goals. I originally wanted to become a professor and work in academia, she says. Now she works for an online pharmacy. As I went through this and I saw how amazing the health care system in this country is in some ways and how awful it is in so many ways, it really inspired me to go into health care and work with other people going through my struggle, she says. That was never on my radar before, and now thats what I want to go into for the rest of my life.
Related:
Also Check: What Are Stomach Ulcers Caused From
Tylenol And Heat Therapy
Doctors frequently prescribe nonsteroidal anti-inflammatory drugs such as ibuprofen or aspirin to help manage back pain. However, NSAIDs arent typically a viable solution for people with UC, as the medication can cause symptoms to flare.
Those with ulcerative colitis can generally take the pain reliever acetaminophen which is not an NSAID for minor aches and pains without side effects. Applying moist heat to affected areas may also reduce pain.
Why Choose Mount Sinai
Mount Sinai has a unique and rich tradition of specialized and individualized treatment and scientific research and discovery in ulcerative colitis. The physicians/scientists in the Mount Sinai Health System are constantly conducting clinical trials and are developing new drug therapies to help patients manage their disease. Learn more about ulcerative colitis.
There are 3 basic tests for colon cancer a stool test , sigmoidoscopy , and colonoscopy . All 3 are effective in catching cancers in the early stages, when treatment is most beneficial.
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
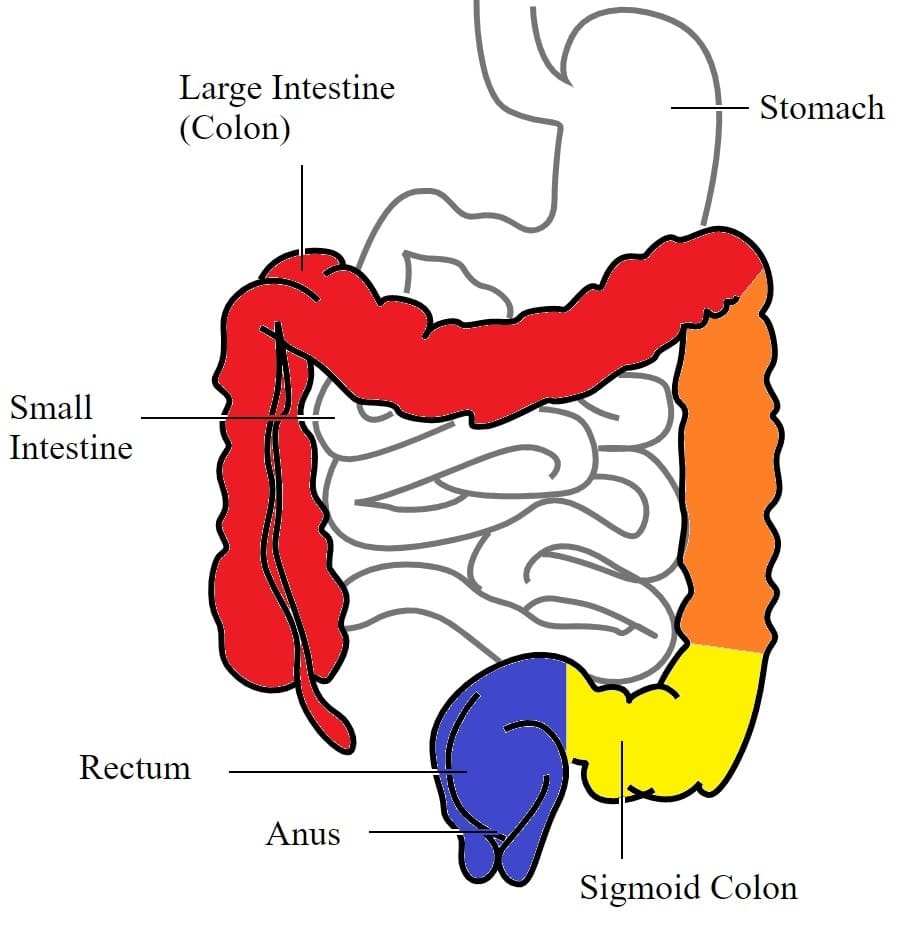
Ulcerative colitis is categorized according to location. Proctitis involves only the rectum. Proctosigmoiditis affects the rectum and sigmoid colon. Left-sided colitis encompasses the entire left side of the large intestine. Pancolitis inflames the entire colon.
Recommended Reading: Where Does It Hurt When You Have An Ulcer
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
Ibd And Altered Na+ Absorption In The Intestine
Mechanisms for vectorial transport of Na+ from apical to the basolateral membrane of intestinal epithelial cells can be a) nutrient dependent or b) nutrient independent.3,9,18,19 The nutrient dependent transport of sodium is mediated via Na+-glucose/amino-acid symporters and is energized by the electrochemical gradient of Na+ established by basolaterally located Na+/K+ ATPase. The symport of these organic solutes and Na+ involves the cotransport of water, which is absorbed osmotically. This has formed the basis of Oral Rehydration Solution used as the primary means for treating dehydration due to diarrhea.9,12,20
Sodium hydrogen exchangers in IBD associated diarrhea
Encoded by members of the SLC9 gene family, the Na+/H+ exchangers mediate the electroneutral exchange of an extracellular Na+ for a cytosolic H+. NHEs are of paramount importance in absorption of sodium and water, maintenance of intracellular pH and cell volume control. So far 11 NHE isoforms have been identified in mammals each having a different cellular localization and tissue distribution. In the intestinal epithelium, NHE2, NHE3 and NHE8 are present on the apical membrane and NHE1 is located on the basolateral membrane.26–30 Expression of other NHE isoforms in the intestine is debatable.31
Don’t Miss: What Foods To Eat For Ulcerative Colitis
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
What Is Ulcerative Proctitis
Of the people who have UC, about 25% to 55% have ulcerative proctitis when they are diagnosed. Your doctor diagnoses ulcerative proctitis based on where in the colon UC is present. When the disease is located in the last 15 centimeters of the colon , it’s termed ulcerative proctitis. If you have UP, you may experience:
-
Rectal bleeding
-
An urgency in your bowel movements
Ulcerative proctitis presents with symptoms such as rectal bleeding and pain, a persistent feeling that you need to have a bowel movement, says Elena Ivanina, M.D., and director of neuro-integrative gastroenterology at Lenox Hill Hospital in New York City. That, or your rectum feels full and your bowel movements have changed, most often to diarrhea.
Don’t Miss: Whey Protein And Ulcerative Colitis
It Can Make Social Events With Food Stressful
Food often dominates family, friend, or coworker gatherings, which can be tricky when you have an invisible illness like UC.
Not everyone understands the challenges of chronic GI issues. People might look at you funny if you’re the only one not happily chowing down at the potluck, or you bring a lunchbox to a catered dinner.
But even when I explain, not everyone understands or accepts my reasons perhaps because they don’t understand how much food can influence UC.
A few bites of the wrong food could leave me doubled over with cramps or make me pull over and dash for a bathroom while driving home. If I say “No, thanks” to a plate, I’m not trying to be rude. I’m just trying to stay on my gut’s good side.
Treatment Of Ulcerative Colitis
Vedolizumab is a drug for people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect it causes is increased susceptibility to infection. Vedolizumab has a theoretical risk of a serious brain infection called progressive multifocal leukoencephalopathy Progressive Multifocal Leukoencephalopathy Progressive multifocal leukoencephalopathy is a rare infection of the brain that is caused by the JC virus. People with a weakened immune system are most likely to get the… read more because this infection has been reported with the use of a related drug called natalizumab.
Ustekinumab is another kind of biologic agent given to people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The first dose is given by vein and then by injections under the skin every 8 weeks. Side effects include injection site reactions , cold-like symptoms, chills, and headache.
Don’t Miss: Drugs To Treat Ulcerative Colitis