Effect Of Probiotics For Maintaining Therapy In Ulcerative Colitis Crohn’s Disease And Pouchitis
Clinical Relapse in Maintaining Therapy in Ulcerative Colitis, Crohns Disease, and Pouchitis
To date, maintaining remission is still one of the goals in IBD therapy. Therefore, a total of 16 trials,,,,,,,, that reported clinical relapse rates were combined in the analysis of maintaining remission. Data were available for 1208 patients, of whom 637 received probiotics as maintaining treatment and 571 received controls with the follow-up ranged from 2 to 42 months. Significant benefit in favor of probiotics administration for lower relapse rates was indicated in the meta-analysis . However, there was moderate to high heterogeneity among these studies .
The forest plot of the clinical relapse rates for probiotics compared with control groups in maintaining remission of IBD.
Subanalyses for Clinical Relapse in Maintaining Therapy in Ulcerative Colitis, Crohns Disease, and Pouchitis
Pooled estimates were, however, characterized by considerable heterogeneity in the meta-analysis of overall clinical relapse rates . Subgroup analyses were carried out on the criteria specified in the protocol to attempt to explain and reduce such heterogeneity.
Endoscopic Relapse in Maintaining Therapy in Crohn’s Disease
Only 3 trials reported endoscopic relapse rates.,, Fortunately, all of the participants pooled in these 3 studies were patients with CD . No statistically significant advantage was found for patients using probiotics for maintaining treatment .
Stanford Scientists Link Ulcerative Colitis To Missing Gut Microbes
Bacteria normally inhabiting healthy peoples intestines and the anti-inflammatory metabolites these bacteria produce are depleted in ulcerative colitis patients, a Stanford study shows.
Aida Habtezion is the senior author of a study that describes how people with ulcerative colitis have insufficient amounts of a metabolite produced by a family of gut-dwelling bacteria.Steve Castillo
About 1 million people in the United States have ulcerative colitis, a serious disease of the colon that has no cure and whose cause is obscure. Now, a study by Stanford University School of Medicine investigators has tied the condition to a missing microbe.
The microbe makes metabolites that help keep the gut healthy.
This study helps us to better understand the disease, said Aida Habtezion, MD, associate professor of gastroenterology and hepatology. We hope it also leads to our being able to treat it with a naturally produced metabolite thats already present in high amounts in a healthy gut.
When the researchers compared two groups of patients one group with ulcerative colitis, the other group with a rare noninflammatory condition who had undergone an identical corrective surgical procedure, they discovered that a particular family of bacteria was depleted in patients with ulcerative colitis. These patients also were deficient in a set of anti-inflammatory substances that the bacteria make, the scientists report.
What Are The Precautions Of Probiotics For Ulcerative Colitis
You are probably thinking of buying the best probiotic for ulcerative colitis now, so you can help remedy your digestive issue. However, there are certain precautions that you need to consider before you start buying all the probiotics that you come across because you should keep in mind that probiotics cannot be used in place of medications when it comes to ulcerative colitis.
Also, if your immune system has been compromised or weakened, you might want to consider other alternatives to soothing the inflammation in your digestive tract. There might be some effects on your overall health if you consume too many probiotics.
The best probiotic for ulcerative colitis can help reduce the symptoms and flare-ups, but they cannot stop it altogether. Therefore you still need to follow the medication that your doctor has prescribed to help you with your digestive problem. Think of probiotics as simply a supplement for your treatment.
Read Also: I Think I Have Ulcerative Colitis
Sparse Current Evidence Points To Some Benefit In Managing Pouchitis And Keeping Uc Quiescent
This Reading Room is a collaboration between MedPage Today® and:
Expert Critique
In the early 1900s, the Russian biologist Élie Metchnikoff of the Pasteur Institute described a correlation between probiotic lactobacillus-containing foods and immunity, intestinal health, and longevity. Since then, researchers have steadily homed in on probiotic therapy as being potentially beneficial in medical conditions ranging from acne and bipolar disorder to Crohns disease and ulcerative colitis .
And consumers have been boarding the probiotics bandwagon, with almost four million Americans reporting the use of prebiotics and probiotics in 2012 according to a National Center for Complementary and Integrative Health , a number that has likely increased even more since the market research firm Nilesen recently reported that 20% of Americans say that probiotics are important to them.
While evidence suggests that probiotics can be effective against various types of diarrhea and functional bowel disease, the potential in inflammatory bowel disease remains unclear. One recent literature found a positive effect of the yeast Saccharomyces boulardii in two CD studies and one UC study.
No benefit of probiotics emerged in inducing remission of active CD, in preventing relapse of quiescent CD, or in preventing endoscopic or clinical relapse of CD after surgically induced remission.
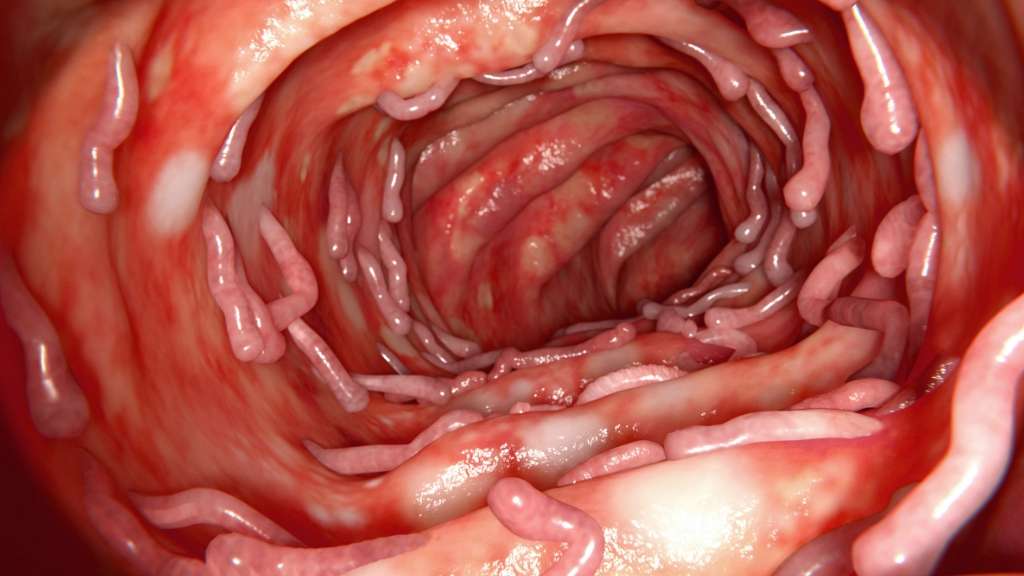
Function Of Large Intestine

The large intestine is a significant part of the digestive tract. It is also known as the gastrointestinal tract . The GI consists of the large intestine, colon as well as the rectum. So, the region starting from the mouth to the rectal opening covers the GI tract. Your small intestine breaks the food particles and sends it to the large intestine. The main function of the large intestine is to reabsorb the water and electrolytes. The waste is then transferred by the colon to the rectum. Finally, the rectum stores the waste , which gets expelled from the body.
Also Check: Humira For Ulcerative Colitis Reviews
Will Probiotics Cure My Ibd
No. Unfortunately there is currently no cure for IBD.
However, some people have found that some probiotics assist in alleviating some symptoms of their IBD. If you choose to take a probiotic it is recommended you do so alongside any other treatment you are undergoing and that you discuss taking it with your doctor before starting.
People who report success with probiotics have found a reduction in symptoms such as bloating, diarrhoea, fatigue, skin conditions and constipation. Probiotics are increasingly being recognised to help people who have irritable bowel syndrome. Many people with IBD suffer from IBS too.
The success rate varies from person to person and a probiotic that may produce results for one person may not do the same for another.
Who Shouldn’t Take Mesalamine
Mesalamine may not be safe if you have certain medical conditions, including:
- An allergy to aspirin or sulfasalazine
- Heart, liver, or kidney disease
- A blockage in your stomach or intestines
- Swelling of the heart muscle, called myocarditis
- Swelling of the sac around the heart, called pericarditis
- Skin problems like eczema or atopic dermatitis
Mesalamine may cause more liver, kidney, and heart risks in older adults. Your doctor might need to adjust the dose to prevent these problems.
You’ll need to avoid Apriso if you have the inherited condition phenylketonuria . This medicine contains the artificial sweetener aspartame, which people with PKU must avoid.
Let your doctor know if you’re pregnant, you could become pregnant, or you’re breastfeeding. There haven’t been enough studies to show that mesalamine is safe to take during pregnancy. You can safely use this medicine while you breastfeed, but let your doctor know if your baby has diarrhea or other side effects.
Recommended Reading: Can You Get An Ulcer In Your Intestines
Probiotic Minas Frescal Cheese Modulated Gene Expression In The Mice Colon
In this work, we sought to evaluable the colonic mRNA expression levels of epithelial barrier genes , production of mucin gene , colonic oxidative stress , and cytokine gene expression . Our results showed that the consumption of conventional or probiotic cheese in healthy control groups was not able to alter the expression of the genes evaluated . The intake of DSS in drinking water also did not alter the expression of zo-1, zo-2, ocln, cln-1, MUC-2, IL-10, and IL-17 genes, when compared with the naive group. On the other hand, we observed an increase in the expression of iNOS and IL-1 genes, when compared with the DSS group and naive group . Interestingly, we observed that the consumption of probiotic cheese in unhealthy mice induced an increase in the expression of zo-1, zo-2, ocln, and cln-1 genes of epithelial barrier, compared with the DSS and naive groups, while the expression of iNOS and IL-1 genes was decreased in animals treated with probiotic cheese. Also, we observed that MUC-2 gene expression tended to increase in animals treated with probiotic cheese but was not statically different from DSS .
Figure 4. Impact of probiotic cheese on colonic expression markers of cell barrier and oxidative stress. Colonic mRNA expression levels of zo-1, zo-2, ocln, cln-1, MUC-2, and iNOS genes analyzed by qRT-PCR. The data represent the mean ± SD . Asterisks represent statistically significant differences: *p< 0.05, **p< 0.01, ***p< 0.001, ****p< 0.0001.
Dr Ohhiras Probiotics Original Formula 60 Capsules
Dr Ohhiras Probiotics Original formula has a three-year-long shelf life and is fermented in nature made from prebiotics, probiotics and postbiotics. It contains live cultures and is fully vegetarian with no gluten, no dairy product, and completely non-GMO. The prebiotic food components used are seaweed, mushroom, fruits, and vegetables. Live probiotics are twelve selected strains that have been cultured together with no fermentation. Postbiotics from the fermentation process include short-chained fatty acids, organic fatty acids like acetic, citric, fulvic, humic and phenyl lactic acid, trace amounts of minerals, lactic and amino acids. The supplement does not contain products that have carcinogenic substances. The probiotic supports good digestion, immune health and promotes a healthy microbial environment.
Don’t Miss: Home Remedies For Stomach Ulcer In Tamil
Good Sources Of Prebiotics
According to a review published in March 2018 in the journal Current Developments in Nutrition, there are eight categories of prebiotic dietary fibers that support digestive health. These categories include:
Fructans These fructose molecules are found in foods like artichokes, asparagus, leeks, onions, jicama, and wheat.
Inulin A group of naturally occurring polysaccharides, inulin is found in foods including chicory root, garlic, onions, leeks, dandelion greens, bananas, and asparagus.
Beta-Glucan This complex sugar is in foods like edible seaweed, algae, oats, barley fiber, and whole grains.
Guar Gum Guar is a fiber from the seed of the guar plant. Guar gum is a common additive used to thicken foods like ice cream, yogurt, and kefir.
Galacto-Oligosaccharides These plant sugars that occur naturally in human milk are also found in dairy products and beans like chickpeas, green peas, lima beans, and kidney beans.
Lactulose The nondigestible, synthetic sugar is primarily used to treat constipation. But according to research published in June 2016 in the journal Microbial Biotechnology, lactulose also stimulates the growth of beneficial bacteria in the human gut. It is used as a food additive to improve taste and stimulate intestinal health.
Xylooligosaccharides and Arabino-Oligosaccharides Similar to GOSs, these simple sugars are commonly found in dairy products, sports drinks, cereals, and bars.
Living With Uc: Probiotics
Probiotics consist of bacteria that confer a health benefit on the person who ingests them. In general, they are bacteria that are normally found in the human intestine. Probiotics have beneficial effects in several medical conditions. Studies have shown that probiotics help people with ulcerative colitis maintain their remissions. Probiotics are found in yogurts and some other foods, but the probiotics that have been studied and found to be effective are sold separately as supplements and are not food products. The effects of probiotics vary greatly and depend on the exact bacteria that are present. Therefore, it is likely that many probiotics that are sold have no beneficial effect, and, therefore, the one that is used for treatment needs to be chosen carefully on the basis of scientific studies.
Also Check: Ulcerative Colitis Nausea In Morning
Do Probiotics Help Ulcerative Colitis And Crohn’s Disease
Researchers are starting to think that imbalances in our gut microbiome are linked to many diseases, ailments and even our mental health.
There is increasing evidence that suggests intestinal microbiota plays a role in initiating, maintaining and determining the characteristics and development of IBD1, 2. And, some people with IBD do report that taking probiotics can help with easing some of their symptoms.
However, studies into the effectiveness of probiotics on people with IBD are limited. There have been a few studies into specific strains of bacteria and their effect on IBD and even fewer studies specifically testing probiotic products on IBD. Generally, at the moment, the research shows that some specific probiotics may be helpful for people with ulcerative colitis but the evidence in Crohns Disease is less convincing.
Some of these studies include:
Probiotic product specific
VSL#3 and pouchitis. The study concluded that high doses of the probiotic VSL#3 are effective in the treatment of mild pouchitis3.
VSL#3 and ulcerative colitis. The study demonstrated that VSL#3 is effective in achieving clinical responses and remissions in patients with mild-to moderately active UC4.
Some studies have also been carried out into Crohn’s disease and microscopic colitis.
Symprove and ulcerative colitis. The study found that 76% of those with ulcerative colitis taking part in the study had significant reductions in faecal levels of calprotectin5.
Bacteria strain specific
Probiotic Fact #: Probiotics Are Strain Dose & Duration Specific
When we evaluate the research on a probiotic in our practice, we always consider the strain name of a probiotic.
When identifying a probiotic, there are three parts to a name:
- The first part is the genus.
- The second part is the species.
- The third part is the strain.
The letters and numbers after that specify the STRAIN of probiotic which is the most important identifying factor when it comes to probiotics. In research on probiotics- the strain name is what differentiates it from the sometimes hundreds of others in its category.
However, many probiotics do not even list the strain name which makes it hard to even evaluate its effectiveness. Not understanding which strain is being used is one major reason why people disagree on the use of probiotics and why its so hard to find consistent information on probiotics for IBD.
The bottom line is: If the strain isnt listed, avoid it.
Beyond strains, the specific dose and how long you take a probiotic can also play a role in its effectiveness. For example, if the evidence shows that it takes 6 weeks to reduce symptoms while taking 10 billion CFUs, we cant expect that taking 1 billion of the same strain for 2 weeks will yield the same results.
Yet oftentimes people will assume probiotics work at every level and any time duration. Like most things- the quality and duration of use can really make a difference. Avoid experimenting on yourself and go with what we know works in research.
Also Check: Children’s Mouth Ulcers Treatment
Who Is At Risk Of Ulcerative Colitis
- Age: Ulcerative colitis may affect any age group, although there are peaks at ages 15 to 30 years, and again at ages 50 to 70 years.
- Race/ethnic background: Ulcerative colitis is more common among caucasians and in people of Ashkenazi Jewish descent.
- Family history: People with a first-degree relative with ulcerative colitis are at greater risk of developing the condition.
Read Also: How To Treat A Diabetic Ulcer
Medications To Treat Crohns Disease And Ulcerative Colitis
We work with our patients to develop treatment to control the disease taking patient preference and personal goals into consideration. We also work with your other providers to minimize drug interaction and make sure that IBD treatment does not compromise the care of your other health concerns.
A full-time clinical pharmacist is available for staff and patients alike to discuss treatment options and provide patient education and resources. You may see the clinical pharmacist one-on-one for the first doses of medication injections. The pharmacist can also work with you to quit smoking and can provide complete medication reviews to assist with medication compliance and understanding.
You May Like: Do Baby Probiotics Help With Gas
Don’t Miss: Diet For Gerd And Ulcers
A Look At The Intestinal Flora Of Ibd Patients
It has been hypothesised for many years that alterations to the intestinal bacterial flora may contribute to the onset and progression of IBD. This is a theory that is now supported by clinical evidence, as several different research studies have found the composition of gut flora to be very different in IBD patients to healthy control patients. Three separate trials1,2,3all found greater numbers of anaerobic bacteria in faecal samples taken from Crohns disease patients than in healthy controls, with particularly elevated levels of Bacteroides .
Contrary to these studies, Giaffer et al4 found no difference in total anaerobes between active CD patients, inactive CD patients and healthy controls, but they did find more aerobes and Enterobacteria in active CD, and fewer Lactobacilli in CD patients than healthy controls.
Other research groups have focused their studies into the presence of possible pathogens in IBD, such as bacteria from the Mycobacteria and Listeria genus.
To date, the results from many of these studies are difficult to interpret and often contradictory. Imbalances in gut flora are generally found, supporting the theory that intestinal flora contributes to the pathogenesis of IBD, but the bacterial species involved often differs.
What Did This Research Look At
People with Crohns Disease and Ulcerative Colitis have a different make-up of the
bacteria living in their gut compared to healthy people. Probiotics, or beneficial bacteria, offer a potentially safe treatment option for people with Crohns and Colitis, but varying results have been seen in clinical trials.
In active Crohns Disease and Ulcerative Colitis, inflammation damages the cells that line the gut allowing microbes and toxins to enter, further advancing the disease.
Bifidobacterium is a beneficial gut bacteria that helps protects the cells lining the gut from damage caused by inflammation. People with Inflammatory Bowel Disease have less of this bacteria in their gut compared to healthy people. The researchers also developed a new technique for screening bacteria. Other researchers will be able to use this technique to identify bacteria with similar protective properties to Bifidobacterium. Finding these bacteria could lead to more potential treatment options for people with Crohns and Colitis.
This research project aimed to identify how Bifidobacterium protects the gut from inflammation.
The researchers identified many properties of Bifidobacterium that allow it to protect against inflammation. Most importantly they found that Bifidobacterium releases a number of biological compounds that can reduce inflammation.
What do researchers think this could this mean for people with IBD?
Who is leading the research: Dr Lindsay J Hall, Quadram Institute Bioscience
Read Also: Best Mattress For Pressure Ulcers