Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
What Is The Best Medicine For Ulcerative Colitis
Treatment strategies for ulcerative colitis vary from person to person. Your doctor will base recommendations for medication on the intensity of your symptoms and severity of the disease. Drugs may be given as combination therapy or single drug therapy.
There are 6 types of medication used to treat UC.
Table: Medications for ulcerative colitis
| Drug | Oral or rectal | Examples |
|---|---|---|
|
Oral and rectal | |
|
Prescribed when previous medications are not effective |
|
|
| FDA-approved to treat moderate to severe | Oral | |
| Monthly shot or intravenous in a hospital setting |
|
|
|
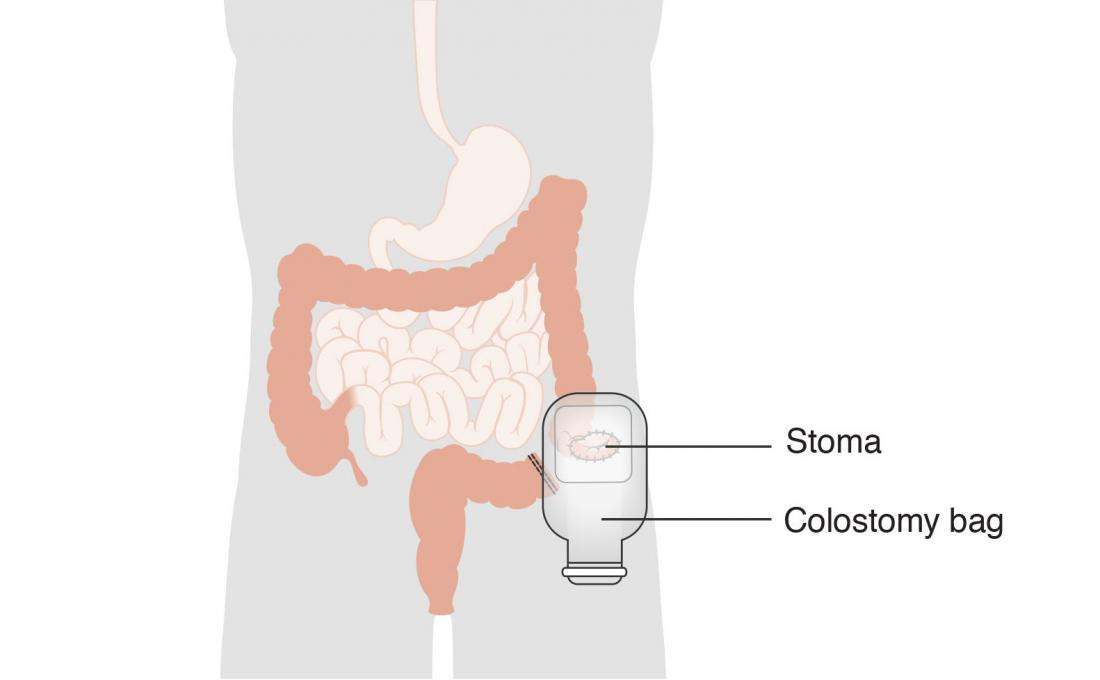
If your body stops responding to medications or if you have emergency complications, you may need to undergo a surgical procedure to remove the affected part of the colon.
Ulcerative Colitis Treatment: Surgery
If you did not respond to a medication regimen or you developed complications of colitis, you may be a candidate for surgery to treat ulcerative colitis.
Colectomy may be used in children with ulcerative colitis who experienced growth retardation. In all patients, elective colectomy can be a cure for ulcerative colitis. Almost always, the procedure is a total colectomy, meaning the entire colon is removed.
Surgical procedures include:
-
Total proctocolectomy with Brooke ileostomy. Removal of your entire colon and rectum. Your doctor will perform an ileostomy, which brings out your small intestine through the abdominal wall. Waste collects in an ileostomy bag. An ileostomy can be temporary or permanent.
-
Restorative proctocolectomy with ileal pouch-anal anastomosis. Removal of the entire colon and most of or the entire rectum. A new rectum is created from the small bowel.This procedure can be performed laparoscopically to ease recovery and reduce scarring.
Recommended Reading: L Glutamine Ulcerative Colitis Dosage
What Is The Treatment For Ulcerative Colitis
Treatment for ulcerative colitis depends on the severity of the condition and how often a patients symptoms worsen . The goal of treatment is to reduce symptoms, and induce and maintain remission .
Ulcerative colitis is usually treated with medication to induce or maintain remissions and improve quality of life. Surgery is a last-resort for patients who have severe inflammation and life-threatening complications.
Medications used to treat ulcerative colitis include:
- Anti-inflammatory drugs
Ulcerative Colitis In Children
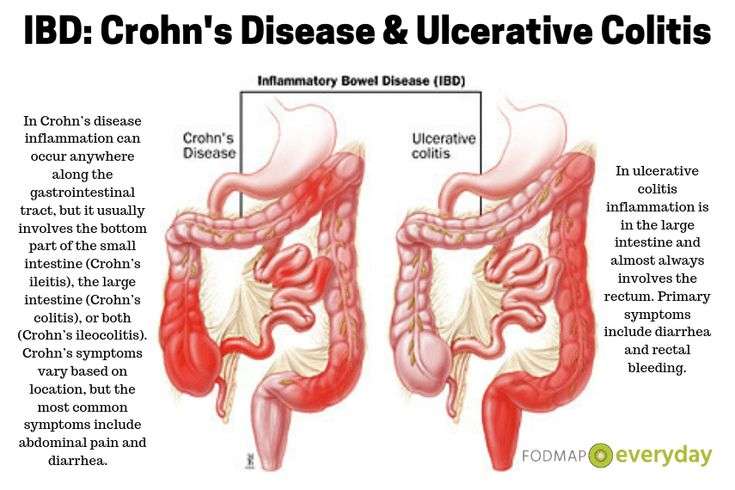
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Also Check: How To Test For Ulcerative Colitis
What Are The Prescription Medications For Uc
Medication for UC is designed to suppress your immune systems abnormal inflammatory responsewhich is causing symptoms. When inflammation is suppressed, it offers relief from common symptoms .
There are 5 main categories of medications used to treat inflammatory bowel disease like UC.
Given either orally or rectally, these drugs work to decrease inflammation in the lining of the intestines and are usually used to treat mild to moderate UC symptoms. Sulfasalazine and mesalamine are examples of 5-ASA medications.
Metronidazole, ciprofloxacin, and other antibiotics may be used when infections occur, or to treat complications of ulcerative colitis.
These suppress the immune system to reduce inflammation by targeting a specific pathway. Certain biologics work by targeting specific inflammatory proteins that play a role in inflammation called cytokines. Others work by preventing certain white blood cells from getting into inflamed tissues.
Prednisone, prednisolone, and budesonide are included in this type of medication. They affect the bodys ability to initiate and maintain an inflammatory processkeeping the immune system in check. While effective for short-term flare-ups, theyre not recommended for long-term use.
These modify the bodys immune system activity to stop it from causing ongoing inflammation. These drugs , and methotrexate) are usually used to maintain remission or for people who have only responded to steroids.
Medications To Treat Crohn’s Disease And Ulcerative Colitis
We work with our patients to develop treatment to control the disease taking patient preference and personal goals into consideration. We also work with your other providers to minimize drug interaction and make sure that IBD treatment does not compromise the care of your other health concerns.
A full-time clinical pharmacist is available for staff and patients alike to discuss treatment options and provide patient education and resources. You may see the clinical pharmacist one-on-one for the first doses of medication injections. The pharmacist can also work with you to quit smoking and can provide complete medication reviews to assist with medication compliance and understanding.
Also Check: Symptoms Of Ulcer In Female
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Testing For Ulcerative Colitis
Often, symptoms alone can provide doctors with the information they need to diagnose ulcerative colitis. Your doctor will perform a physical examination and take a complete medical history that includes a careful review of your symptoms. For this reason, it is important to be candid and specific with your doctor about the problems you are having.
There is no one specific laboratory test, X-ray or scope to diagnose ulcerative colitis, however, to help confirm the condition and rule out other problems, your doctor may send you to have one or more of the following tests:
Read Also: Worst Foods For Stomach Ulcers
Ulcerative Colitis Treatment Options You Should Be Aware Of
Ulcerative colitis can be unpredictable, which can make it challenging for physicians to determine whether a particular course of treatment has been effective. The main goal of treatment in UC is to reduce the signs and symptoms of ulcerative colitis by regulating the immune system, and to bring about long-term remission. While there is no cure for UC, treatment can help control symptoms so that patients can lead a fuller life. Treatment may include over-the-counter as well as prescription medications, lifestyle changes in stress management, diet and nutrition, and surgery.
Prescription medications typically include anti-inflammatory drugs, immune suppressants, and steroids. If these are not effective, -alpha inhibitors, or biologics, drugs typically given to treat certain types of arthritis, may be used.
Who Is At Risk Of Ulcerative Colitis
- Age: Ulcerative colitis may affect any age group, although there are peaks at ages 15 to 30 years, and again at ages 50 to 70 years.
- Race/ethnic background: Ulcerative colitis is more common among caucasians and in people of Ashkenazi Jewish descent.
- Family history: People with a first-degree relative with ulcerative colitis are at greater risk of developing the condition.
Read Also: How To Treat A Diabetic Ulcer
Can Probiotics Help Stop Flare
The answer to this question is likely no. A 2007 review of clinical studies on the use of probiotics for UC flare-ups found that probiotics do not shorten the duration of a flare-up when added to regular treatment.
However, the people in the studies taking probiotics reported fewer symptoms during the flare-up, and these symptoms were less severe. In other words, while probiotics did not end the flare-up faster, they seemed to make the symptoms of the flare-up less frequent and less severe.
Is Ulcerative Colitis Curable
Currently, theres no nonsurgical cure for UC. Treatments for the inflammatory disease aim to extend periods of remission and make flare-ups less severe.
For people with severe UC, curative surgery is a treatment option. Removing the entire large intestine will end the symptoms of UC.
This procedure requires your doctor to create a pouch on the outside of your body where waste can empty. This pouch can become inflamed and cause side effects.
For that reason, some people choose to have only a partial colectomy. In this surgery, your doctor only removes the parts of the colon that are affected by UC.
While these surgeries can help ease or end symptoms of UC, they can have adverse effects and possible long-term complications. Read more about these issues to determine if surgery is an option for you.
Read Also: What Does Asacol Do For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Diet And Lifestyle Changes
Although diet and stress do not cause ulcerative colitis, there may be times when changes in your lifestyle may help control your symptoms and lengthen the time between flare-ups. The following changes may help to ease your symptoms:
- Limit milk/dairy products. If you are lactose intolerant , milk and dairy products can produce symptoms of excess gas and diarrhea.
- Restrict intake of certain high-fibre foods: such as nuts, seeds, and raw vegetables.
- Limit intake of caffeine, alcohol, carbonated drinks and fatty foods. .
- Eat small, frequent meals, rather than large meals..
- Exercise regularly to promote movement of the colon and reduce stress..
- Minimize stress. Yoga, meditation and slow, relaxed breathing techniques can help people with ulcerative colitis manage stress..
Ask your doctor or pharmacist if one of these formulations may be right for you. It is important to take the probiotic in the dose and duration recommended by the manufacturer to achieve the best results.
Also Check: Do Enemas Help Ulcerative Colitis
Can Probiotics Help Prevent Flare
The use of probiotics for this purpose shows more promise.
Several studies have shown that probiotics may be as effective as traditional UC medications, including the gold-standard treatment mesalazine.
A 2004 German study followed a group of 327 patients with a history of UC, giving half of them mesalazine and the other half probiotics . After one year of treatment, the average time to remission and the quality of remission was the same for both groups.
Similar results have been seen in other studies. And another probiotic, Lactobacillus GG, may also be helpful in sustaining remission in UC.
Probiotics may help in treating UC because they address the actual cause of the condition.
UC is thought to be caused by problems with the immune system in the intestines. Your immune system helps your body fight disease, but it can sometimes lash out and target your own body in an effort to protect it from a perceived danger. When this happens, its called an autoimmune disease.
In the case of UC, an imbalance of bacteria in the large intestine is thought to be the perceived danger that prompts the immune system to respond.
Probiotics may help by providing good bacteria that help restore the bacterial balance in the intestine, eliminating the problem to which the immune system is responding. With the perceived danger gone, the immune system may soften or stop its attack.
If you would like guidance on finding a high-quality probiotic, talk to your doctor.
- garlic
Lifestyle Changes For Ulcerative Colitis
Its also important to control stress, as it can worsen UC symptoms and may trigger ulcerative colitis flare-ups. Exercise, meditation, yoga and biofeedback, a stress-reduction technique designed to reduce muscle tension and slow heart rate via a feedback machine, are often recommended to help ulcerative colitis patients reduce stress levels.
Recommended Reading: What To Eat When You Have Ulcers And Acid Reflux
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Recommended Reading: Foods To Avoid With Peptic Ulcer
Probiotics For Ulcerative Colitis: Do They Work
Probiotics are microorganisms that we take into our bodies to support our health. Typically, theyre strains of bacteria that can help improve our digestion, or so-called good bacteria. Probiotic products are intended to supply healthy, gut-friendly bacteria to populate the intestinal wall.
Probiotics are found in certain foods. They also come in supplements, which are available in a variety of forms, including tablets and capsules.
While many people take probiotics to support their general digestive health, theyve also been used to treat certain intestinal problems such as gastroenteritis and a condition called pouchitis. But can these good bacteria also be used to treat ulcerative colitis ?
UC is an inflammatory disease of the large intestine that causes bloody diarrhea, cramping, and bloating. The disease is relapsing and remitting, which means there are times when the disease is quiet, and other times when it flares up, causing symptoms.
Standard medical treatment for UC has two components: treating active flare-ups and preventing flare-ups. With traditional treatment, active flare-ups are often treated with corticosteroids such as prednisone. Flare-ups are prevented with maintenance treatment, which means using certain drugs long term.
Lets look at whether probiotics can help with either of these treatment needs.
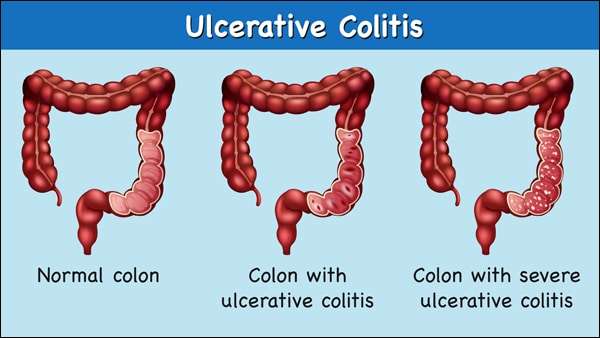
Symptoms Of Ulcerative Colitis
Most symptoms are related to the inflamed rectum. The inflammation does not allow the rectum to stretch or store properly. This affects a patient’s ability to sense what is in the rectum, making them feel the urgency to use the bathroom more often. Very little stool will pass during these many trips to the bathroom â sometimes just mucus and blood.
When inflammation spreads to the lower part of the intestine, people can feel paradoxically constipated. The reason for this is that the bowel above the inflammation is working fine, but when it gets to the inflamed area, it can’t stretch like it is supposed to. That can cause an internal back up, causing bloating and gas.
Some people may experience extraintestinal manifestations, which refers to inflammation in other parts of their body. The most common manifestation is symmetrical joint pain, which occurs on both sides of the body, often in smaller joints. Other less common types include skin and/or liver inflammation. Extraintestinal manifestations are connected to the bowel inflammation and will get better if the inflammation in the large intestine is treated.
Also Check: How Many People Have Ulcerative Colitis