Foods To Help Treat Gastritis
Two foods that may help treat gastritis are broccoli and yogurt.
Broccoli contains a chemical called sulforaphane, which has antibacterial properties. It also contains antioxidants, which can help protect against cancer. For this reason, eating broccoli sprouts may help relieve or prevent gastritis and decrease the risk of stomach cancer.
Authors of an older study, published in 2009, found that participants with H. pylori infection who ate 70 grams more than half a cup of broccoli sprouts per day for 8 weeks had lower levels of infection and inflammation than those who did not eat broccoli.
In 2006, another team investigated whether eating about 2 cups of probiotic yogurt daily before using a combination of antibiotics could boost the ability of the medication to combat drug resistant H. pylori infection.
After 4 weeks, the researchers found that the participants who consumed the yogurt and antibiotics tended to eliminate the infection more effectively than those who only took antibiotics.
The results may have stemmed from the yogurts active cultures of beneficial bacteria that help improve the bodys ability to combat infection.
Also Check: How To Heal Ulcers In Large Intestine
Are Ulcers Common In Diabetic
What is the appearance of a diabetic ulcer? If the ulcer has progressed to a severe state, this should be visible. A foot ulcer appears as a circular red crater in the skin that is surrounded by thicker calloused skin. Severe ulcers may reach a depth of several centimeters, exposing tendons or bones. Other symptoms, on the other hand, may be more difficult to diagnose or may be indicative of another issue.
What are diabetic ulcers ? Diabetes ulcers are open lesions or sores on the soles of the feet. These ulcers afflict a large number of diabetics, and specialists estimate that around 15% of diabetics may acquire one or more over their lives.
Are diabetic ulcers reversible? Patients with diabetes and lower limb vascular disease often recover slowly, and a foot ulcer may take weeks or months to fully heal.
I was diagnosed with type 2 diabetes 5 months ago with an A1c of 11 and then 8.9 My doctor instructed me to take Metformin, which I despise since I know there are alternatives, such as a healthy diet and regular exercise. Therefore, I opted not to take Metformin and instead took
- * Multi vites vitamin
Abundant amounts of potable water
I also shed 11 pounds. I eliminate all types of rice from my diet
Cut out Bread , no chips, no soda,
I did My three-month test and my Ac1 level decreased from 8.9 to 6.5 without the use of Metformin.
What The Pain Feels Like
When your ulcer is acting up, its hard to ignore. Youll get burning pain between your breastbone and belly button. It may last a few minutes, or you could have it for hours. The problem may also get worse between meals, when you dont have any food in your stomach. It could even wake you up at night.
Also Check: Can Tylenol Cause Stomach Ulcers
Read Also: How To Cure Ulcer Naturally At Home In Tamil
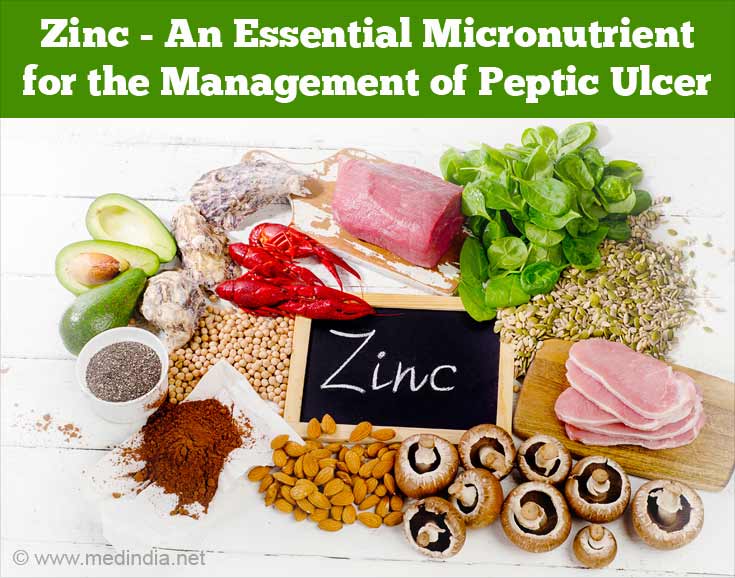
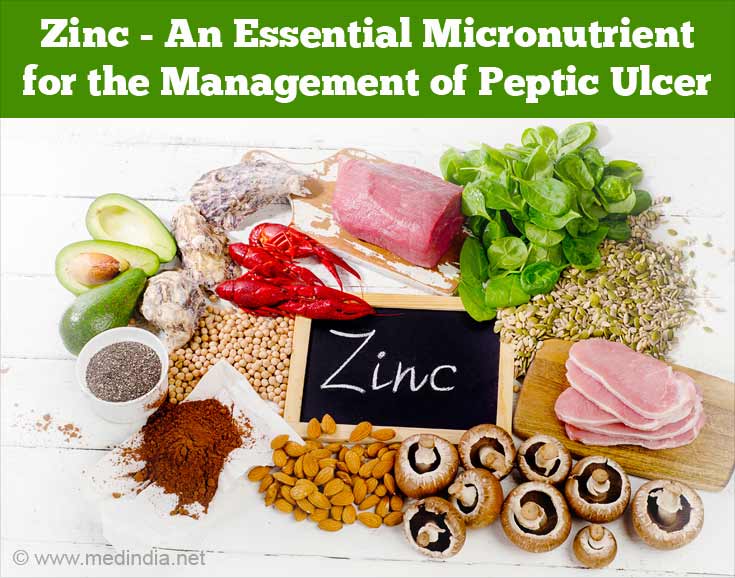
What Are Peptic Ulcers
Peptic ulcers, also called as stomach ulcers, are characterized by the occurrence of an open sore on the inner lining of the stomach. The sore may be on the proximal, middle or distal part of the stomach or in the duodenum, the initial part of small intestine, following the stomach.
Diseases of the gastro-intestinal tract such as peptic ulcers and dyspepsia are quite common among the urban population today due to improper eating habits and erratic lifestyle adopted due to the influence of technology. People today have chosen jobs involving prolonged hours of sitting in front of the PC and often skipping meals, which is quite common due to busy working hours.
Irregular meal timings combined with having large meals at a time all play a role in disturbing the functioning of the normal digestive system. Paying proper attention to regularizing meal timings & minding the portion size of meals can help reverse gut disorders such as peptic ulcers.
Ulcers are often the result of inadequate presence of the bicarbonate ions in the stomach lining. Hence, on account of inadequate bicarbonate ions to neutralize the H+ ions in the acidic secretions of the gut, the stomach acid has the capacity of corroding the stomach lining. This gives rise to ulcers.
Heart Burn And Diabetes
The term heart burn is very misleading, as it has nothing to do with the heart. It is a stomach problem that occurs when stomach acid comes into contact with the oesophagus. The oesophagus is the tube that food goes down when you swallow and ends at the stomach.
Diabetics can sometimes suffer with heartburn as a result of damage to the nerves that control the lower oesophogeal sphincter, or the valve at the entrance of the stomach.
This means that after a meal, especially if lying down, the lower oesophageal sphincter does not tighten sufficiently and can let some acidic stomach content back into the oesophagus that can burn and feel irritated or painful.
A condition caused by the same degeneration of the vagus nerve is gastroparesis which is the inability of the stomach to empty, and push food into the intestine. If this occurs, the stomach will stay fuller for longer, opening up more opportunities for heart burn.
- For more information, see our guide on diabetes and gastroparesis
It is possible to combat the symptoms of heart burn with antacids which can be bought at chemists or in a lot of supermarkets.
Recommended Reading: How To Heal Venous Stasis Ulcers
What Causes Diabetics To Develop Styes
Additionally, the condition makes your eyelids more susceptible to infection, which can result in styes. High blood sugar levels may also result in the development of chemicals that decrease immunological systems, making people with uncontrolled diabetes more susceptible to infections and at risk for styes.
What Are The Causes Of Peptic Ulcers
The most common causes of peptic ulcers has been found to be Helicobacter pylori infection which invade the intestinal lining and damage it while proliferating. Also, indiscriminate use of NSAIDs has found to precipitate peptic ulcers.
Alcohol & tobacco intake as well as consumption of oily, spicy foods may worsen the condition of peptic ulcers, but has not been found to cause them. The most common, first line treatment for ulcers is administration of antacids and proton pump inhibitors which dilute the concentration of acid secretions in the stomach or reduce the acid production respectively.
Also Check: Over The Counter For Ulcers
Foods To Limit When You Have Acid Reflux And An Ulcer
Some people who have an ulcer also have acid reflux. In some people, certain foods can relax the lower part of the esophagus, known as the lower esophageal sphincter or LES. A relaxed LES makes it easier for acid to back up into the esophagus and cause heartburn, indigestion, and pain.
Foods that may make acid reflux worse include:
- coffee
Really Ulcers Increase The Risk Of Diabetes
THE FACTS
Poor diet, a lack of exercise, excess weight and genetics are the usual risk factors for Type 2 diabetes. But a new line of research suggests that in some cases, there may be a surprising contributor: the stomach bacterium known as Helicobacter pylori.
People who acquire H. pylori typically in childhood are at a greater risk of ulcers and gastric cancer. But H. pylori also is thought to affect two digestive hormones involved in hunger and satiety.
The belief is that the bacterium increases levels of ghrelin, the hunger hormone, which is known to promote weight gain. At the same time, H. pylori is thought to lower levels of leptin, the satiety hormone, which reduces appetite and promotes calorie burning.
In a study published in The Journal of Infectious Diseases this year, researchers looked at more than 13,000 people in the National Health and Nutrition Examination Surveys. The data showed that people who had H. pylori in their systems also had higher levels of something called HbA1c, a compound considered a strong predictor of diabetes and metabolic syndrome, which includes high blood pressure, high blood sugar and an excess of certain fats in the bloodstream.
Scientists studying the link say more research is needed. But treating H. pylori, they say, may one day be a way to control or prevent Type 2 diabetes in some people.
THE BOTTOM LINE
Recommended Reading: What Should You Not Eat If You Have An Ulcer
Diabetes Linked To Ulcer
The same bacterium responsible for most stomach ulcers may play a role in the development of Type 2 diabetes among overweight and obese adults, researchers at NYU Langone Medical Center are reporting today.
And in the same way that antibiotics eradicate the bacterium and heal ulcers, antibiotics might eventually prove useful in diabetes prevention, they suggest in an article appearing in the Journal of Infectious Diseases.
Non-diabetic adults infected with Helicobacter pylori , tended to have higher blood sugar than adults without H. pylori, according to the study co-authored by Yu Chen, an associate professor of environmental medicine at NYU, and Dr. Martin J. Blaser, chairman of NYU’s department of medicine.
Chen and Blaser assessed blood sugar levels using measurements of glycosylated hemoglobin , a marker of excess glucose in the bloodstream that in recent years has become a key tool for diagnosing and monitoring diabetes.
Helicobacteri pylori is a complicated bacterium. Persistent H. pylori infections beginning in childhood have been linked decades later to ulcers of the stomach and small intestine, and a heightened risk of stomach cancer. Although H. pylori can inflame the stomach, many infected people have no symptoms.
Blaser called H. pylori a complicated and interesting organism that affects children and adults in entirely different ways. In previous work he and Chen found that H. pylori protects children against asthma and allergy.
Are Diabetics Susceptible To Abscess
Insulin injection abscesses are common in diabetic individuals and are often caused by Staphylococcus aureus. However, we must check for more species that may create difficulties in order to provide proper therapy. The purpose of this article is to describe a case of injection abscesses caused by an unusual mycobacterium, Mycobacterium chelonae.
Read Also: What Dies A Stomach Ulcer Feel Like
Green Tea And Flavonoid
Emerging research from China shows the potential protective effects of green tea and other foods that are rich in flavonoids against chronic gastritis, H. pylori infection, and stomach cancer. Specifically, these foods seem to inhibit the growth of H. pylori.
In addition, one recent laboratory study of green, white, oolong, and black teas indicated that these teas inhibit the growth of H. pylori but cause no harm to beneficial types of bacteria normally found in the stomach, including L. acidophilus, L. plantarum, and B. lungum. However, this was an in vitro study, which means testing occurred directly between teas and bacteria in the laboratory, and we cannot draw direct conclusions as to what would happen inside the human body between these two substances. Beneficial effects in the laboratory were best when tea steeped for a full five minutes.
Flavonoid-rich foods include garlic, onions, and colourful fruits and vegetables such as cranberries, strawberries, blueberries, broccoli, carrots, and snap peas.4,5
How Is Gastroparesis Treated
Gastroparesis is a chronic condition. This means that treatment usually doesnt cure the disease, but you can manage it and keep it under control. People who have diabetes should try to control their blood glucose levels to reduce the problems of gastroparesis.
Some people may benefit from medications, including:
- Reglan: You take this drug before you eat, and it causes your stomach muscles to contract to help move food out of your stomach. Reglan also helps cut down on vomiting and nausea. Side effects include diarrhea and, rarely, a serious neurological disorder.
- Erythromycin: This is an antibiotic that also causes stomach contractions and helps move food out. Side effects include diarrhea and development of resistant bacteria from taking the antibiotic for a long time.
- Antiemetics: These are drugs that help control nausea.
Surgery for gastroparesis
People with gastroparesis who still have nausea and vomiting even after taking medications may benefit from surgery. One type of surgery for gastroparesis is gastric electrical stimulation, which is a treatment that sends mild electric shocks to your stomach muscles. In this procedure, your provider inserts a small device called a gastric stimulator into your abdomen. The stimulator has two leads that are attached to your stomach and provide mild electric shocks, which help control vomiting. Your provider can adjust the strength of the electric shocks. The device runs on a battery that lasts up to 10 years.
Read Also: What Is The Best Medicine For Mouth Ulcer
Administration Of Vitamin C
Vitamin C was administered orally as previously described . Briefly, using an orogastric tube, each rat in Groups 2 and 4 was administered vitamin C at a dose of 200mg/kg body wt. daily for four weeks. Administration was done between 08:00 and 09.00 GMT each day. Rats in the control groups received 2mL of distilled water .
Diet Plan For A Stomach Ulcer
Prior to the 1980s, stomach ulcers were typically blamed on stress or spicy foods â and thus a bland diet was a common treatment. But we now know that ulcers aren’t caused by these factors.
Video of the Day
Instead, most stomach ulcers are a result of the Helicobacter pylori bacteria, and some are linked to long-term use of nonsteroidal anti-inflammatory drugs , such as ibuprofen and aspirin.
But that also means there is no specific diet that treats stomach ulcers. However, you may find certain foods worsen or ease your symptoms, and some foods may even help ulcers heal. Talk to your doctor and you can work together on finding the best combination of foods for you.
Don’t Miss: How Do You Get Ulcerative Colitis
How Should A Diabetic Foot Ulcer Be Treated
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing of the wound, the less chance for an infection.
There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Prevention of infection
- Taking the pressure off the area, called off-loading
- Removing dead skin and tissue, called debridement
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
Not all ulcers are infected however, if your podiatric physician diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
Preventing Infection
There are several important factors to keep an ulcer from becoming infected:
- Keep blood glucose levels under tight control
- Keep the ulcer clean and bandaged
- Cleanse the wound daily, using a wound dressing or bandage
- Do not walk barefoot
Off-Loading
For optimum healing, ulcers, especially those on the bottom of the foot, must be off-loaded. Patients may be asked to wear special footgear, or a brace, specialized castings, or use a wheelchair or crutches. These devices will reduce the pressure and irritation to the ulcer area and help to speed the healing process.
Applying Medication and Dressings
For a wound to heal there must be adequate circulation to the ulcerated area. Your podiatrist may order evaluation test such as noninvasive studies and or consult a vascular surgeon.
Managing Blood Glucose
Histology Of The Stomach
Routine histology of the stomach was carried out in parts of the isolated gastric tissues obtained from animal in each group. The tissues were fixed in 10% formalin solution, dehydrated in ascending grades of alcohol, and embedded in paraffin. Sections of 5m thickness were taken, stained with hematoxylin and eosin , and examined by a histopathologist under light microscopy.
You May Like: Vsl 3 And Ulcerative Colitis
How Common Are Stomach Ulcers
It’s not known exactly how common stomach ulcers are. They have become much less common since the 1980s because of much more effective treatments. So people with stomach ulcers now usually get better much more quickly.
The term ‘peptic ulcer’ is used to describe ulcers that are caused by too much acid in the stomach. This includes stomach ulcers and also ulcers in the first part of the gut known as the duodenum. Stomach ulcers are less common than duodenal ulcers.
Dont Get Burned By Fried Foods
Its hard to avoid fried foods theyre pretty much everywhere you turn in our face-paced world. Theyre also, unfortunately, quite delicious. However, as EveryDayHealth.com warns, Overdoing the greasy stuff can pack on the pounds and cause blood-sugar chaos.
Common fried foods include French fries, fried chicken, and potato chips, it adds. Keep in mind too that many of these items are deep fried in hydrogenated oils that are laden with unhealthy trans fats, it warns.
Recommended Reading: What Foods To Eat When You Have An Ulcer
Symptoms Of Stomach Ulcers
Although the most common symptom of a stomach ulcer is a burning or gnawing pain in the centre of the abdomen . Not all stomach ulcers are painful.
Some people experience:
Speak to your GP immediately if:
- your symptoms persist
- youre vomiting blood the blood can appear bright red or have a dark brown, grainy appearance like coffee grounds
- youre passing dark, sticky, tar-like stools
- you feel a sudden, sharp pain in your tummy that gets steadily worse
These could be a sign of a serious complication.
Also Check: How To Treat Mouth Ulcers
What Happens After Treatment
A repeat gastroscopy is usually advised a few weeks after treatment has finished. This is mainly to check that the ulcer has healed. It is also to be doubly certain that the ‘ulcer’ was not due to stomach cancer. If your ulcer was caused by H. pylori then a test is advised to check that the H. pylori infection has gone. This is done at least four weeks after the course of combination therapy has finished.
Recommended Reading: New Treatment For Ulcerative Colitis 2020