Scenario : Ulceration In Backwash Ileitis
There is no evidence in the literature that ulceration is part of the spectrum of backwash ileitis. The problem arises when the colon shows features compatible with UC, but the terminal ileum is involved by what appears to be backwash ileitis, except that it is accompanied by ulceration, pyloric metaplasia, or architectural distortion. These features, although not diagnostic of CD, are sufficient to raise the possibility of CD, despite the lack of other evidence in the colon. Pyloric metaplasia is seen frequently in ileal resections from patients with CD. It represents a non-specific reparative reaction in intestinal ulcers, and is not specific for CD. In a study of adults with definite evidence of CD, pyloric metaplasia was identified in 22.2% of the terminal ileal biopsies. A previous study with similar data showed an incidence of only 2.27%. The difference could reflect the duration of the disease, the extent of pre-existing terminal ileal ulceration, the opportunity for mucosal repair before biopsy, or the thoroughness of the endoscopic sampling and/or pathological examination. Pyloric metaplasia lacks specificity for CD, but may be a sensitive indicator of persistent ulceration with inflammation. When found in terminal ileal biopsies, it could support the diagnosis of CD in the appropriate clinical setting.
What Procedures And Tests Diagnose Crohn’s Disease And Ulcerative Colitis
Doctors diagnose ulcerative colitis by endoscopy . During this procedure the doctor can see and take pictures of the patients abnormal gut mucosa , and the presence of continuous disease . Other blood tests and imaging tests like CT scan or MRI are used, but these tests are not definitive.
Doctors use the same procedures and tests to diagnose Crohns disease. However, they also use small bowel studies, colonoscopy, and upper GI endoscopy to identify the abnormal gut mucosa that usually occur in multiple areas anywhere in the intestinal tract. These areas are not continuous, but are separated by normal areas of intestinal mucosa that distinguish them from ulcerative colitis lesions.
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
Symptoms And Signs Of Ulcerative Colitis
Patients typically have
-
Attacks of bloody diarrhea of varied intensity and duration interspersed with asymptomatic intervals
Usually an attack begins insidiously, with increased urgency to defecate, mild lower abdominal cramps, and blood and mucus in the stools. Some cases develop after an infection .
When ulceration is confined to the rectosigmoid, the stool may be normal or hard and dry, but rectal discharges of mucus loaded with red and white blood cells accompany or occur between bowel movements. Systemic symptoms are absent or mild.
If ulceration extends proximally, stools become looser and the patient may have > 10 bowel movements per day, often with severe cramps and distressing rectal tenesmus, without respite at night. The stools may be watery or contain mucus and frequently consist almost entirely of blood and pus.
Toxic or fulminant colitis manifests initially with sudden violent diarrhea, fever to 40° C , abdominal pain, signs of peritonitis , and profound toxemia.
Don’t Miss: Blood Clots In Stool With Ulcerative Colitis
Upper Gastrointestinal Tract Involvement
- The old dogma was upper GI tract = Crohn’s disease.
Characteristics of upper GI tract UC:
- Most common:
- Mixed basal inflammation and superficial plasmacytosis in the stomach.
- Unique:
- ~ 40% of UC + colectomy + pouchitis.
Another study compares UC, CD and control individuals:
- Gastritis:
- Younger individuals have significantly more gastritis and duodenitis.
A tabular comparison
| usu. no seen in pancolitis |
| Upper GI tract involvement |
“Minimal abnormalities” – features:
- Macrophages in the lamina propria.
- Lymphoid nodules.
- “Abundant” plasma cells in the lamina propria.
- Abundant is subjective.
COLON, BIOPSIES:- QUIESCENT INFLAMMATORY BOWEL DISEASE.- NEGATIVE FOR DYSPLASIA.
Biopsies All Submitted In One Bottle
COLON , BIOPSIES:- MODERATE CHRONIC ACTIVE COLITIS.- NEGATIVE FOR DYSPLASIA.- PLEASE SEE COMMENT.COMMENT:The sections show colorectal-type mucosa with focal cryptitis and rare neutrophilic cryptabscesses.Mild architectural changes, suggestive of a chronic colitis, are present. No granulomas areidentified. Lymphoid aggregates with germinal centre formation are present in multiplefragments. The lamina propria has abundant plasma cells throughout the fragments no fragments have apparent relative sparing. Paneth cells are present focally however, the significance of the paneth cells cannot determined as the biopsy sites are not known. The findings are compatible with inflammatory bowel disease and chronic active infectiouscolitides. Clinical correlation is suggested.
Recommended Reading: Best Way To Treat Mouth Ulcers
Scenario : Proximal Skip Lesions In Uc
Infrequently, one encounters in a colectomy specimen distal disease with features of UC, whereby the upper margin of the diseased distal mucosa may be separated from additional more proximal diseased mucosa by a grossly skipped area. The importance of the disease distribution in this scenario is not clear. One approach would be to ignore this atypical UC distribution if there is no other compelling evidence of CD, but at least not hasten into a firm diagnosis of CD.
When an area of caecal inflammation is present, the differential diagnosis of caecal involvement separated from disease of the distal colon or rectum by normal mucosa is UC with caecal patch versus CD with a skip area. It is important to ascertain that the intervening mucosa is uninvolved, and if so not to assume that the disease is CD. Sampling of the terminal ileum is helpful, because it is usually uninvolved in UC with a caecal patch. If biopsies of the terminal ileum and intervening colonic mucosa are available and unremarkable, a diagnosis of IBD consistent with UC is made. However, if terminal ileal and intervening colonic mucosal biopsies are not available, a diagnosis of IBD is made but importantly without favouring CD. The clinician is advised to obtain such biopsies in the future and to confirm or exclude the presence of other features of CD, such as small bowel involvement and perianal disease.
What Is The Difference Between Crohns Disease And Ulcerative Colitis
Both Crohns disease and ulcerative colitis are inflammatory bowel diseases , however, there are distinct differences between these diseases. This video developed by the GI Society with Dr. Mike Evans, illustrates the differences between Crohns disease and ulcerative colitis, the impact of these diseases, possible causes and prevalence.
Inflammatory Bowel Disease video courtesy of GI Society
Recommended Reading: What Are Some Symptoms Of An Ulcer
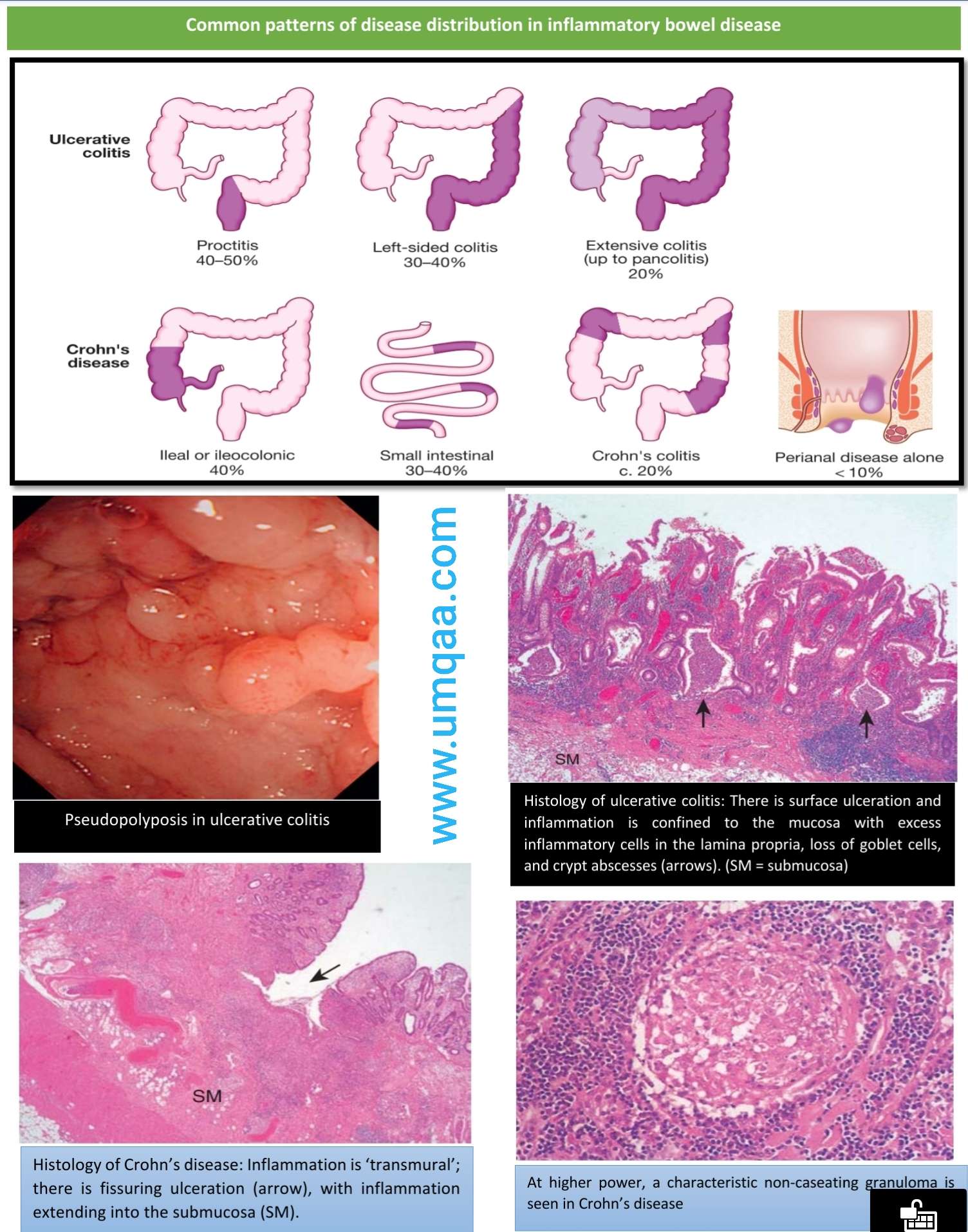
Histopathology Of Ulcerative Colitis
The histologic hallmark of UC is a diffuse superficial chronic active colitis. The mucosa is affected, while deeper layers of the bowel wall are spared . The degree and severity of active inflammation is dependent on disease activity and treatment and is histologically classified according to the extent of crypt involvement and the presence or absence of ulceration . The Montreal classification of UC is a clinical classification scheme that emphasizes the importance of disease extent and severity at diagnosis: E1 is inflammation limited to the rectum , E2 is inflammation limited to the splenic flexure , and E3 is pancolitis.
As its name implies, UC manifests as ulceration in severe disease. An ulcer is an area of markedly eroded mucosa with fibrin deposition, inflammatory cell infiltration, and granulation tissue formation. Ulceration exceeding 50% of the examined mucosa is referred to as fulminant colitis. Diffuse ulceration leaves polypoid portions of nonulcerated mucosa in its wake these are inflammatory pseudopolyps, not true neoplasms, but rather islands of relatively intact mucosa surrounded by ulcer. Filiform pseudopolyps take on an exaggerated, prominent, vermiform appearance.
Treating Crohns And Colitis
Its important to know that neither Crohns nor ulcerative colitis can be cured, though doctors will work with patients to manage symptoms. The two illnesses are generally treated with the same types of medication, although each patient may respond differently to the same drug. The goal of treatment is to reduce the inflammation, which in turn reduces symptoms, allows your body to repair damaged tissue, and helps slow the progression of the disease.
Today, many patients get a relatively new class of drugs, called biologics, which are live antibodies that are given to patients to help their immune cells fight the inflammation. Other classes of drugs include immunomodulators, which help tamp down the immune systems inflammatory response, and aminosalicylates, the oldest class of drugs, which are used to help keep the disease in remission. According to the Crohns and Colitis Foundation, immunomodulators can take up to six months to become fully effective, so doctors usually prescribe them along with fast-acting steroids that patients will ideally go off of once the immunomodulators reach their full potential. I absolutely think that with these new drugs, its a new era in the treatment of inflammatory bowel disease, says Dr. Cohen.
Read Also: Black Tarry Stools Ulcerative Colitis
Crohns Disease Vs Ulcerative Colitis Differences In Symptoms Causes And Treatment
Written byDevon AndrePublished onOctober 22, 2017
Crohns disease and ulcerative colitis are part of the group of conditions known as inflammatory bowel diseases . Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development although the exact cause is still unknown.
For those living with IBDs, their immune system mistakes food and bacteria in the gastrointestinal tract for an allergen or foreign substance, so it sends out cells to destroy it. The result of these attacks is chronic inflammation.
Although the exact causes of Crohns disease and ulcerative colitis are unknown, genetics and environmental factors are believed to play a role. Crohns disease and ulcerative colitis are often interchanged for one another, but we will outline the differences between the two, including symptoms, causes, and treatments in order to provide you with a better understanding of either condition.
When Surgery Is Needed
If medication isn’t reducing the inflammation and IBD progresses, surgery may be needed. This is where people with ulcerative colitis tend to fare better.
If the colon gets bad enough in ulcerative colitis, its removed and replaced with an internal pouch, which functions like a colon, says Cohen. According to the Mayo Clinic, colectomy surgery whether partial or full usually requires additional procedures that reconnect the remaining portions of the digestive system so they can still rid the body of waste.
However, things are looking up. A study published in December 2019 in the Journal of Gastrointestinal Surgery found that due to advances in medicine and medical care for IBD patients over the past decade, the number of hospitalized patients with ulcerative colitis who require a colectomy decreased by nearly 50 percent between 2007 and 2016.
According to the Crohns and Colitis Foundation, proctocolectomy with ileal pouchanal anastomosis usually called J-pouch surgery is the most common surgery performed on people with UC who have not responded to medication. Surgeons remove the rectum and colon and then create a temporary opening in the abdomen, called a loop ileostomy, which will allow waste to move from the small intestine into an ostomy bag that sits outside the body while the digestive system heals from the surgery. In some cases a stoma, or permanent opening in the abdomen that funnels waste into an external bag, is required, notes the Mayo Clinic.
Also Check: Can Diverticulitis Cause Ulcerative Colitis
Effects Of Treatment On Histology Of Ibd
Iatrogenic inflammatory changes that may be confused with IBD may represent the effects or bowel preparation compounds administered before lower endoscopy. Sodium phosphate, a commonly used oral cathartic agent, causes aphthoid ulcers or focal active colitis in the colon and rectum that might lead to an endoscopic diagnosis of CD, especially in quiescent IBD.
Crohns Disease Vs Ulcerative Colitis: Us Prevalence And Incidence Rate
The CDC estimated that one to 1.3 million Americans is affected by IBD. Generally, ulcerative colitis is found to be more common in males where Crohns disease is more common in females. Prevalence of Crohns disease in the U.S. is 26 to 199 per 100,000 persons,and ulcerative colitis is 37 to 246 per 100,000 persons.
Incidence rate of Crohns disease is 3.1 to 14.6 cases per 100,000 person years, and for ulcerative colitis it is 2.2 to 14.3 cases per 100,000 person years.
Don’t Miss: Can Ulcerative Proctitis Be Cured
The Role Of Biomarkers And Treatment Options In Uc
The adhesion of T lymphocytes from the peripheral circulation to the gut mucosa is a central step for the progression of the inflammatory process in UC . Different anti-adhesion agents have been suggested for UC treatment. Vedolizumab is a humanised monoclonal IgG-1 antibody that selectively inhibits 47 integrin and mucosal addressin cell adhesion molecule-1 interaction. It prevents lymphocyte infiltration from the blood into the inflamed gut tissue, reducing local inflammation . In addition to this effect, vedolizumab also reduces 47-dependent gut homing of non-classical monocytes, resulting in a decrease in alternatively activated M2-like macrophages in the gut . In contrast to other anti-adhesion drugs, the use of vedolizumab in UC patients did not increase the rates of opportunistic or enteric infections and there were no reported cases of progressive multifocal leukoencephalopathy . Following encouraging results in randomized, double-blind, placebo-controlled trials in the pivotal phase III GEMINI studies, vedolizumab has been approved by US FDA for the treatment of adult patients with active UC who had a poor response to standard therapies . Nevertheless, mononuclear phagocyte enrichment was detected in non-responder UC patients before vedolizumab treatment, which further increased post treatment , partly explaining why some UC patients do not respond as well to this drug.
When To See A Physician
Brief periods of bowel irregularity are common for most, with many taking a wait-and-see attitude. However, a number of indications serve as warnings and should prompt a visit with a physician. Such signs or symptoms include:
- Abdominal pain that doesnt ease within a day or two
- Multiple or recurrent signs of blood in the toilet bowl or in your stool
- Diarrhea that fails to respond to over-the-counter treatments or change in diet
- Chronic sense of fatigue
- Inexplicable weight-loss
A visit to your physician is a good idea for any change in bowel habits. If left untreated, both ulcerative colitis and Crohns disease can contribute to a number of potential complications including severe dehydration, bleeding, a perforation, as well as an increased risk of colon cancer.
Don’t Miss: What Not To Eat With Bleeding Ulcers
Indeterminate And Unclassified Colitis
In up to 5% of IBD cases, a definite diagnosis of either UC or CD cannot be established . Diagnostic uncertainty is usually an issue in children. However, disease involvement limited to the colon with a histological pattern of patchy acute and chronic inflammation with architectural changes, not consenting a final diagnosis, may be an issue in adults as well. In the literature several different terms have been used to cover such cases, including indeterminate colitis , inflammatory bowel disease unclassified , chronic inflammatory bowel disease unclassified and chronic idiopathic inflammatory bowel disease not otherwise specified. In order to allow comparison between different studies, the ECCO/ESP consensus report from 2013 supported an alinement on terminology that suggest the term IC should be limited to diagnoses based on histological examination of surgical specimens. Thus, the term IBDU is preferred in case of a patient with chronic colitis with clear signs of IBD based upon the clinical history, but where endoscopy and histology biopsies are inconclusive. Both IC and IBDU should be considered a temporary diagnosis, as disease progression over time often enables a classification of either UC or CD.
Difference Between Crohns Disease And Ulcerative Colitis Causes
As with many autoimmune diseases, the exact cause of either Crohns disease or ulcerative colitis is unknown. Some theorized causes of Crohns disease include the immune system being triggered by a virus or bacteria, and heredity as many patients with Crohns disease will also have a relative with the condition.
The immune system is also suspected to play a role in ulcerative colitis along with genetics and environmental factors. There seems to be some genes involved in the development of ulcerative colitis, and having more than four family members with ulcerative colitis increases your risk of developing it. Environmental factors include place of residence, especially because there appear to be higher rates of ulcerative colitis in urban areas, North America, and Western Europe. Air pollution, medications, and consuming certain diets have also been found to be associated with a higher risk of ulcerative colitis.
Read Also: Over The Counter For Ulcers
String Sign Vs Lead Pipe Appearance
- String sign: In Crohns disease, the lumen gets extremely narrow in places as a result of scarring, edema, and spasms. Contrast material in the lumen of the gut sometimes looks thinned out like a string.
- Lead-pipe appearance: In ulcerative colitis, mucosal scarring and sloughing destroys the normal architecture of the colonic mucosa, causing a lead pipe appearance.
Ulcerative Colitis: Barium enema demonstrates loss of haustral folds in the entire descending colon. The colon has a lead-pipe appearance. Published with permission from LearningRadiology.com.
Site Of Inflammation Differs Between Crohns Disease And Ulcerative Colitis
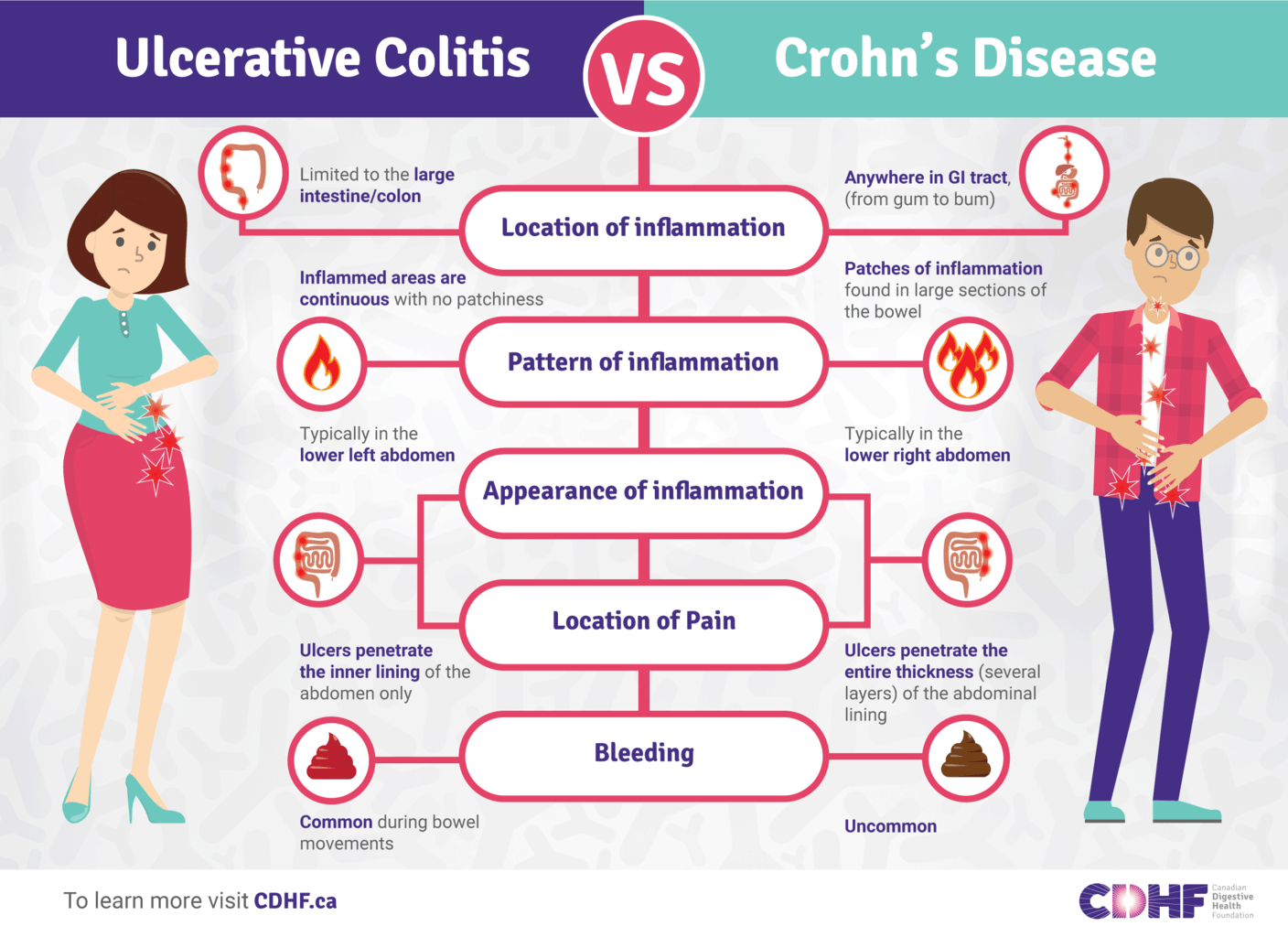
Crohns disease can affect any part of the gastrointestinal tract, including the mouth, esophagus, stomach, small and large intestines, rectum and anus. Ulcerative colitis is located in the colon, usually starting from the rectum. In Crohns disease, inflammation occurs in all layers of the intestinal wall and patches of this inflammation can be scattered throughout the GI tract. In contrast, in ulcerative colitis, inflammation occurs in the innermost lining of the intestinal wall and is a continuous stretch within the colon.
Recommended Reading: Ulcerative Colitis And Lung Disease