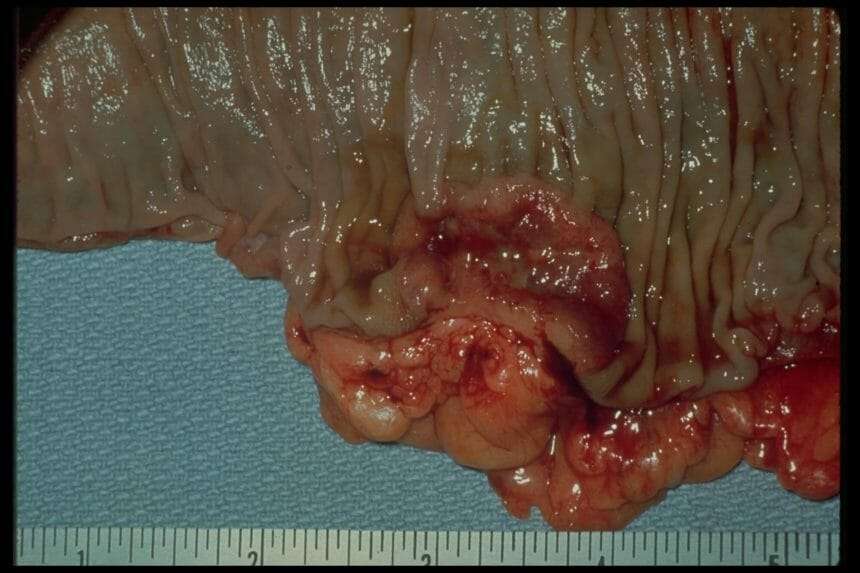
Ial Or Total Colon Resection
In a total resection, the entire large intestine is removed. While this is the only true cure for UC, it can reduce quality of life.
In a partial resection, colorectal surgeons remove the diseased region of the colon with a margin of healthy tissue on either side. When possible, the two remaining ends of the large intestine are surgically united, reconnecting the digestive system.
When this cant be done, the bowel is routed to the abdominal wall and waste exits the body in an ileostomy or colostomy bag.
With modern surgical techniques, its potentially possible to reconnect the remaining bowel to the anus, either during the initial resection surgery or after a healing period.
Closely Monitor Your Symptoms
A sudden return of your symptoms such as diarrhea, abdominal pain, or bloody stools are likely to be a sign that you are experiencing a flare-up, and your treatment may need to be adjusted. However, sometimes, the symptoms of a flare-up may be subtler and not immediately apparent.
This is why it is essential to keep track of even the smallest change you feel. Let your doctor know if you experience any of the following:
- If you notice blood in your stool
- If you are having more bowel movements than usual
- If you see a change in the amount or texture of your bowel movements
- If you feel tired or seem to have less energy than usual
- If you are losing weight or if you notice a loss in appetite
- If you notice any other symptoms such as mouth sores or joint pain
It is a good idea to maintain a symptom diary to help keep track of your day to day condition. This will also help you explain your symptoms in detail to your doctor.
More Drugs That Work On Your Immune System
Other types of medicines for ulcerative colitis target your immune system, too. Your doctor may call these immunomodulators. They may be good options if 5-ASAs and corticosteroids havenât worked well for you.
The most common ones are azathioprine , mercaptopurine , and cyclosporine . Due to the risk of side effects, doctors usually save cyclosporine for people who donât have success with other meds. They may also try methotrexate paired with folic acid.
Ozanimod is an oral medication and is the first sphingosine 1-phosphate receptor modulator approved for patients with moderately to severely active UC.
The goal is to lower inflammation in your colon.
These drugs can have side effects. They can damage your liver and make you more likely to get skin cancers, lymphoma, and infections. If you take them, your doctor will test your blood and check you for skin cancer regularly.
Cyclosporine is especially strong, but it works fast. Your doctor might prescribe it to get a severe flare under control, and then give you 6-MP or azathioprine afterward. The drug may cause kidney problems, gout, infections, and high blood pressure.
It can take several months for some of these drugs to work. So your doctor may give you a faster-acting medicine, like a low dose of a corticosteroid, to help in the meantime.
Recommended Reading: How Long Does A Ulcerative Colitis Flare Up Last
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
How Often Do I Need A Colonoscopy

Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: What Are Infusions For Ulcerative Colitis
Calcium And Vitamin D Keep Bones Strong
Kristi L. King, MPH, RD, a dietitian at Texas Children’s Hospital and a clinical instructor at the Baylor College of Medicine in Houston, says that low stores of calcium and vitamin D are the main vitamin and mineral deficiencies in patients with ulcerative colitis. When you have this condition, “the intestines and colon dont absorb nutrients in the same way they do for someone without the disease,” she notes, adding that many drugs commonly prescribed to treat colitis, such as prednisone, can also interfere with the absorption of calcium and vitamin D when used for prolonged periods of time. And, losing calcium and vitamin D will deplete your bone density and put you at risk of osteoporosis. Up to 60 percent of people with inflammatory bowel disease have lower-than-average bone density, according to the Crohns and Colitis Foundation.
You may not have any noticeable symptoms, but your gastroenterologist should regularly check for these deficiencies as part of ulcerative colitis treatment, King says. Over-the-counter supplements can help restore healthy levels. Making some changes to your diet will help, too.
Food Supplements For Ulcerative Colitis
A well-balanced diet is your first step to guard against malnutrition. You need to eat a variety of things from different food groups and make sure you get enough protein and calories. Work with a dietitian who can help you plan meals that meet your nutrition needs.
Even with a well-designed meal plan, you may still need some of these supplements:
Vitamin D. You need it to keep your bones strong. It also plays a role in how your immune system — your body’s defense against germs — works.
If you have ulcerative colitis, especially if you need steroids, you may be at risk for having low levels of vitamin D.
A good source of vitamin D is dairy foods, but a lot of people with UC cut back on dairy to help them curb symptoms of diarrhea.
Experts have different views on vitamin D supplements, so ask your doctor if it’s a good idea for you to take them.
Calcium. It’s a mineral your body uses to build bones, help your muscles contract, and send messages through your nervous system.
If your system doesn’t have enough calcium, your body removes it from the bones, which causes them to become brittle and leads to a bone-weakening disease called osteoporosis.
If you avoid calcium-rich dairy products or need certain kinds of medicines, you could be at risk for low levels of calcium. If your doctor recommends a calcium supplement, you’ll probably need 1,000 to 1,200 milligrams a day.
Read Also: How To Reduce Bloating With Ulcerative Colitis
Buyer Beware For Probiotics Users
In the U.S., probiotics are marketed as dietary supplements, so they havent gone through the same rigorous FDA testing as drugs.
This means we have no way of knowing for certain if a product has the bacterial strains or the concentration of bacteria that its label claims.
The higher-ups at the FDA are hoping to change this soon, but for now, we have to go by our own experience and hope for the best.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Recommended Reading: Can Ulcerative Colitis Go Into Remission
Treatment Of Ulcerative Colitis
Current therapies to treat patients with ulcerative colitis include aminosalicylates , steroids, immune suppressants, and biologic therapy . For some of these drugs, treatments are available in pill form, suppositories, enemas, injections under the skin, and intravenous infusions. Although medical treatment can be effective in controlling the symptoms of ulcerative colitis, patients must take medications continuously to prevent the symptoms from returning.
Although some patients require a ileostomy after colectomy, another surgical procedure can be performed in many patients later to reverse the ostomy called a restorative proctocolectomy or J pouch. This procedure allows patients to have bowel movements without an ostomy.
There have been many advances in surgery for ulcerative colitis. The most significant are development of restorative proctocolectomy and use of minimally invasive surgery .
Blood Tests Provide The Bottom Line
Dont guess when it comes to your nutrition. Get a complete blood count test done at least once a year, including testing your iron and ferritin levels . Your lab work will also reveal info about vitamin D, calcium, and vitamin B12 levels. If youre low in any of these or other nutrients, your doctor may suggest taking a supplement. Whatever your course of action, follow up with additional lab work in a few months to see if your deficiency has been corrected, says Javelli.
Read Also: Can Ulcerative Colitis Cause Blood In Urine
Possible Complications From Surgery
Part of bowel surgery involves creating a pouch near the anus, which collects waste prior to defecation.
One of the complications of surgery is that the pouch can become inflamed, which causes diarrhea, cramps, and fever. This is called pouchitis, and it can be treated with an extended course of antibiotics.
The other main complication of bowel resection is small bowel obstruction. A small bowel obstruction is first treated with intravenous fluid and bowel rest . However, a severe small bowel obstruction may need to be treated with surgery.
Although surgery may cure the gastrointestinal symptoms of UC, it may not always cure other affected sites. Occasionally, people with UC have inflammation of the eyes, skin, or joints.
These types of inflammation may persist even after the bowel has been totally removed. While this is uncommon, it is something to consider before getting surgery.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Also Check: What Does A Skin Ulcer Look Like
Medication Options For Ulcerative Colitis
Medication is the first line of treatment for ulcerative colitis. Your doctors recommendation for which medication will work best for you is based on the severity of your disease, your overall health, and other individual factors.
There are six major classes of medication used to treat ulcerative colitis.
Effective Treatment For Ulcerative Colitis
It is first of all necessary to understand what effective treatment looks like for Ulcerative Colitis. Overall, your doctors consider your Ulcerative Colitis treatment to be successful if you are able to form stools without urgency, cramping, or bleeding.
There are two parts to an effective treatment for Ulcerative Colitis. The first is controlling the symptoms, and the second part is to maintain that control over the symptoms. Both of these factors are very important to determine whether or not the treatment is effective and successful. If you are experiencing lesser flare-ups and are able to live a better quality of life than what you were living before you began the treatment, then these are some of the biggest signs that your treatment is working.
The effective management of your condition requires you to be aware of all the treatment options there are for Ulcerative Colitis. Medication for Ulcerative Colitis can come in various forms from enemas, suppositories, to pills and shots, to even intravenous infusion or a combination of these.
However, sometimes, a treatment just does not work for you, or it may stop working. If the medications are not helping in managing your flare-ups, then here is what you can do to start feeling better again.
Read Also: What To Do For Ulcer Pain
Go To Sleep Stomach: How To Sleep Better If You Have Ulcerative Colitis
A bout one-third of adults in the United States dont get enough sleep, according to the Centers for Disease Control and Prevention and for people who are dealing with the symptoms of ulcerative colitis, nodding off can be extra challenging. At one point, Jordan Wilson, a My Take Ulcerative Colitis contributor, found himself running to the bathroom as many as seven times a night.
After getting a J-pouch four years ago, Wilson sleeps easier still, he has to wake up at least once a night to use the restroom. What helps him: Eating dinner well before going to bed. I watch what I eat or eat lighter at night, he says. Or, it sounds counterintuitive, but sometimes Ill actually stay up later if I ate late. That way he can use the bathroom right before lying down for the night and then hope to get a solid four to five hours of sleep without disturbances.
For Laura Steiner, another My Take Ulcerative Colitis contributor, falling asleep can be trickier than sleeping through the night. When she has trouble nodding off, she tries to relax in bed. I get the heating pad out if I need to, maybe take some deep breaths and do some guided meditation, listen to some good music thats relaxing, read a book, she says. And generally that helps me fall asleep a little bit faster especially compared to playing on my phone, she adds.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Read Also: How To Treat A Diabetic Foot Ulcer On The Sole
It Helps Maintain Remission In Ulcerative Colitis
Clinical studies suggest the consumption of curcumin for maintaining remission in patients with ulcerative colitis.
In a review study conducted by Garg and his colleagues, clinical trials were conducted on patients with ulcerative colitis for a span of six months it was found that curcumin is a safe and effective therapy for maintaining remission in ulcerative colitis for a longer period.
An experimental study conducted by Hanai et al. evaluated the effects of curcumin as a therapy for ulcerative colitis. Eighty-nine patients with ulcerative colitis participated in the study.
Forty-five patients were administered with 1g of curcumin, once after breakfast and once after the evening meal. Rest of the patients were allotted to the control group.
Results of the study showed that out of 43 patients only 2 relapsed in the 6-month curcumin treatment group whereas 8 out of 39 relapsed in the placebo group.
With curcumin treatment disease activity was reduced and also these changes were evidenced by endoscopy tests.
At the end of the therapy, 10 patients in the curcumin group relapsed while 14 in placebo group. Researchers concluded that curcumin is a safe and effective therapy to maintain remission.
Another experimental study conducted by Singla et al. in 2014 suggested that curcumin is capable of improving remission in patients with ulcerative colitis. Patients were assigned to receive:
Curcumin enema plus oral mesalazine Placebo enema plus oral mesalazine