When To Call A Doctor
Its best to touch base with your doctor regularly when you have Crohns. Since the disease has no cure, you want to stay on top of your treatment to avoid flares as best you can.
If any of your symptoms suddenly get worse, try to call a doctor as soon as you can. You also want to make an appointment right away if you have persistent vomiting, symptoms of a fistula or intestinal blockage, or high fever.
Ner With A Licensed Ibd Dietitian For A Healthy Nutritional Diet Plan To Reduce Uc Flare
Do you have IBD but are confused when choosing the best food for ulcerative colitis? Or do you find yourself restricted to just a few foods? It doesnt have to be this way. Working one on one can be a great way to get to symptom reduction faster and reduce the stress of figuring it out on your own.
Partner withCrohns and Colitis Dietitians today and get professional help creating a nutritional therapy plan to help reduce the symptoms of ulcerative colitis.Contact us today at 306-7517 orget started on your nutritional plan by booking a consultation.
Resources:
Study Design And Participants
In the present cross-sectional study, the diet adequacy and food avoidance habits of UC patients in the UK were investigated. The study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the ethics committee of a UK Higher Education Institution. Written informed consent was obtained from all participants.
A total of ninety-seven UC patients were recruited across the UK from the National Association for Colitis and Crohn’s Disease registers by e-mail, posts in UC forums and social media sites. The inclusion criteria were as follows: aged 1865 years and no history of UC-related surgery.
Initially, four participants participated in a pilot study to ensure that the questionnaire and 24 h dietary recalls were readable and not distressing.
Don’t Miss: What Foods Are Good For Ulcers
Specific Carbohydrate Diet And Ulcerative Colitis
The specific carbohydrate diet was created to reduce the amount of carbohydrates in the intestines. There is some evidence that the SCD may improve ulcerative colitis symptoms.
The SCD is based on the idea that microbes in the gut that contribute to ulcerative colitis use carbohydrates as an energy source leading to the production of toxins that damage the intestine.
The SCD restricts all sugars except for monosaccharides . The SCD allows you to eat most fruits and vegetables, meat, eggs, and nuts. Processed foods, sugar, cereals and dairy products containing the sugar lactose are not allowed.
How Can Diet Help With My Symptoms
Making changes to your diet may help you manage some common symptoms of Crohns and Colitis, such as loose and runny stools, dehydration, bloating, wind, constipation, weight loss, tiredness, nausea and vomiting and pain. While changing your diet can help you manage your symptoms, it doesnt replace the medical treatment suggested by your IBD team.
Loose and runny stools
A common symptom of Crohns and Colitis is loose and runny stools, called diarrhoea. For some people, their diet has no effect on their diarrhoea. Others find that avoiding certain foods helps. You could use the food diary above to help you find out which foods might be causing your symptoms. Foods which sometimes make diarrhoea worse include spicy or fatty foods, high fibre foods, foods containing gluten and dairy foods. Drinks containing caffeine, sweeteners or alcohol can also make diarrhoea worse.Your IBD team or dietitian can advise you on how to manage your diarrhoea. They will want to make sure youre eating and drinking enough to get all the nutrients you need and to stay hydrated. In some cases, they may recommend medicines to help.Our guide Diarrhoea and constipation has more information about what causes diarrhoea and possible treatments.
Dehydration
If your body doesnt have enough water, you can become dehydrated. This might happen if you dont drink enough fluids or if your body loses too much fluid, for example, if you have diarrhoea or vomiting.You may be more likely to get dehydrated if:
Also Check: Good Foods To Eat With Stomach Ulcer
The Worst Foods For Those With Ulcerative Colitis
- by Colorectal Surgery Associates
- May 5, 2020
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.
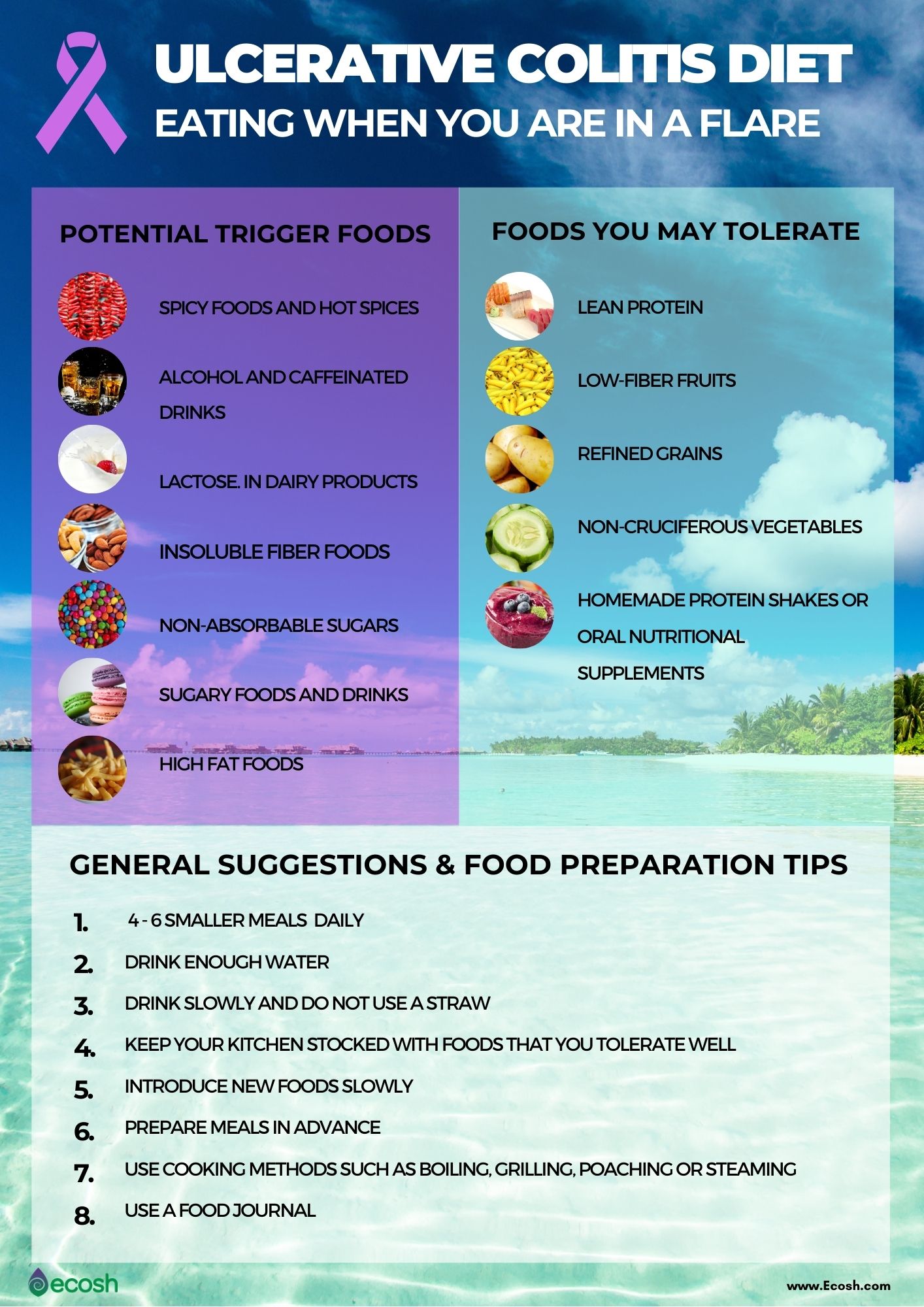
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
You May Like: Medication For Ulcerative Colitis Flare Up
Vegan Diet And Ulcerative Colitis
A healthy well-balanced diet containing all food groups is recommended for ulcerative colitis. While high fat foods such as butter and cream may impact on ulcerative colitis there have been no studies so far that show vegan nutrition offers more benefits than a balanced diet including animal products.
Does Keeping A Food Diary Help
It may be helpful to keep a food diary in order to help you and your nutritionist plan out a diet plan.
Keeping a food diary involves recording what you eat and any symptoms you may experience in the hours after. This can then be used to narrow down any specific foods or food groups that trigger your symptoms.
Often finding the right diet plan is a process of elimination. This can be done by cutting out one particular food from the diet for a period of time and observing whether symptoms resolve during that time. Alternatively many food groups can be eliminated and individual foods introduced back one at a time to try and identify those that trigger your symptoms.
Recommended Reading: Ulcerative Colitis Abdominal Pain Relief
Ulcerative Colitis Diet Plan
Ulcerative colitis is a chronic, inflammatory bowel disease that affects the colon and rectum. If a person has ulcerative colitis, sores develop inside the colon. These are called ulcers.
It is not known what exactly causes ulcerative colitis, but researchers believe that it may be caused by a problem with the immune system. There are several things that may trigger a flare and worsen the condition. Foods are one of them. Certain foods may not be suitable for some people.
Read about causes of ulcerative colitis.
Researchers are learning about the role of diet and gut bacteria in causing the disease ulcerative colitis. The Academy of Nutrition and Dietetics and the Crohns and Colitis Foundation of America accept that fiber is helpful for your colon. Fiber should only be reduced if you experience acute problems such as flare-ups.
When you experience flare-ups, a low-fiber diet may be considered to help you recover quickly. But if your doctor has not recommended a low-fiber diet to manage the disease symptoms, you should follow a high-fiber diet only.
Caffeine Carbonated Beverages Alcohol
Beverages that speed up the rate of digestion like coffee and caffeinated teas should be avoided. Carbonated beverages may also irritate your bowels further, so these are best avoided as well. Furthermore, alcohol is a known stomach and bowel irritant, so save the alcoholic beverages for when you are feeling better, as well.
Also Check: What Do You Do For An Ulcer In Your Stomach
Lay Off Sweets And Sugar
One of the ways scientists suspect that sweets and sugars are not good for those with UC is that they studied what those from Japan ate 20 years ago: a diet high in rice and low in sweets and sugars. Since that time, sweets and sugars have been on the rise in Japan as well as UC. While this may paint only part of the picture, other studies have shown that high consumption of soft drinks has been associated with UC.
What Causes Ulcerative Colitis

The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitiscan run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress, and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
Read Also: What Is A Gastric Ulcer And What Is Its Cause
What If Youve Had Surgery For Uc
If youve had surgery for UC, such as an ileostomy , your GI may give you specific guidelines regarding your diet and nutrition. For example, they may recommend you eat extra foods with vitamin B12 or take a supplement since removal of the ileum can make it hard for you to absorb the B12 you need. A lack of this vitamin can affect the health of your nerve and blood cells.
Its also extra important to stay hydrated if youve had surgery for UC, so make sure youre drinking lots of water and eating foods with a high-water content. Talk with your health care team and registered dietitian to understand how your surgery may affect your dietary needs.
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesn’t exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
You May Like: Is Ulcerative Colitis A Chronic Disease
Signs And Symptoms Of Ulcerative Colitis
The most common UC symptom is bloody diarrhea or pus in the stool. Besides, other symptoms include:
- Sudden and frequent need to poop
- Cramping bowel pain
- Canker sores
- Pain or bleeding with bowel movements
Although ulcerative has no cure, knowing what to eat with colitis can effectively mitigate the on-and-off cycle of these symptoms, and can aid in the reduction of inflammation and risk of flare.
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Also Check: Best Vitamins For Ulcerative Colitis
Reintroducing Your Usual Diet
Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet – after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method – this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet – this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements – which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
Back Up: What Is Ulcerative Colitis Exactly
Ulcerative colitis is a type of inflammatory bowel disease that causes ulcers and sores in the lower quarter to third of your digestive tract. Typically, these ulcers are found in your rectum or in the inner lining of your lower intestine . This can cause bloody diarrhea, the most common symptom of ulcerative colitis, but you might also experience things like abdominal cramping, constipation, and a general sense of fatigue. Weight loss and a loss of appetite can also crop up, per the U.S. National Library of Medicine.
Diana Whitehead, M.D., director of the Inflammatory Bowel Disease Center at the Greater Baltimore Medical Center, explains that though ulcerative colitis has a strong genetic component, symptoms are often set off by a triggering event that activates inflammation in the lower intestine. Basically, your immune system is not doing what it should do, which is to protect you, but its gone kind of into overdrive, Dr. Whitehead says. In other words, even though the exact causes of ulcerative colitis arent fully understood, experts consider it to be an autoimmune condition thats set off by this overreaction in the gut.
Don’t Miss: Wet To Dry Dressing For Pressure Ulcers
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Is There A Specific Ulcerative Colitis Diet

There is no specific diet for ulcerative colitis. A healthy well-balanced diet containing all food groups is recommended.
Foods containing sulphites such as processed foods should be avoided as well as high fat foods such as butter and cream, and fried or greasy food.
Often food intolerances accompany ulcerative colitis. If this is the case then the corresponding foods should be excluded from the diet.
Recommended Reading: How To Know If Have Stomach Ulcer
Ulcerative Colitis Diet Facts And Tips
- There is no specific ulcerative colitis diet
- Overall a healthy well-balanced diet is recommended
- Limit dairy products containing lactose if youre lactose intolerant
- Avoid high fat foods such as butter, coconut, margarine, and cream, as well as fried, or greasy food
- Keep a food and symptom diary to help create an individual diet plan
- Be aware your dietary needs may change during a flare-up and throughout the course of your condition