Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience extreme tiredness , loss of appetite and weight loss.
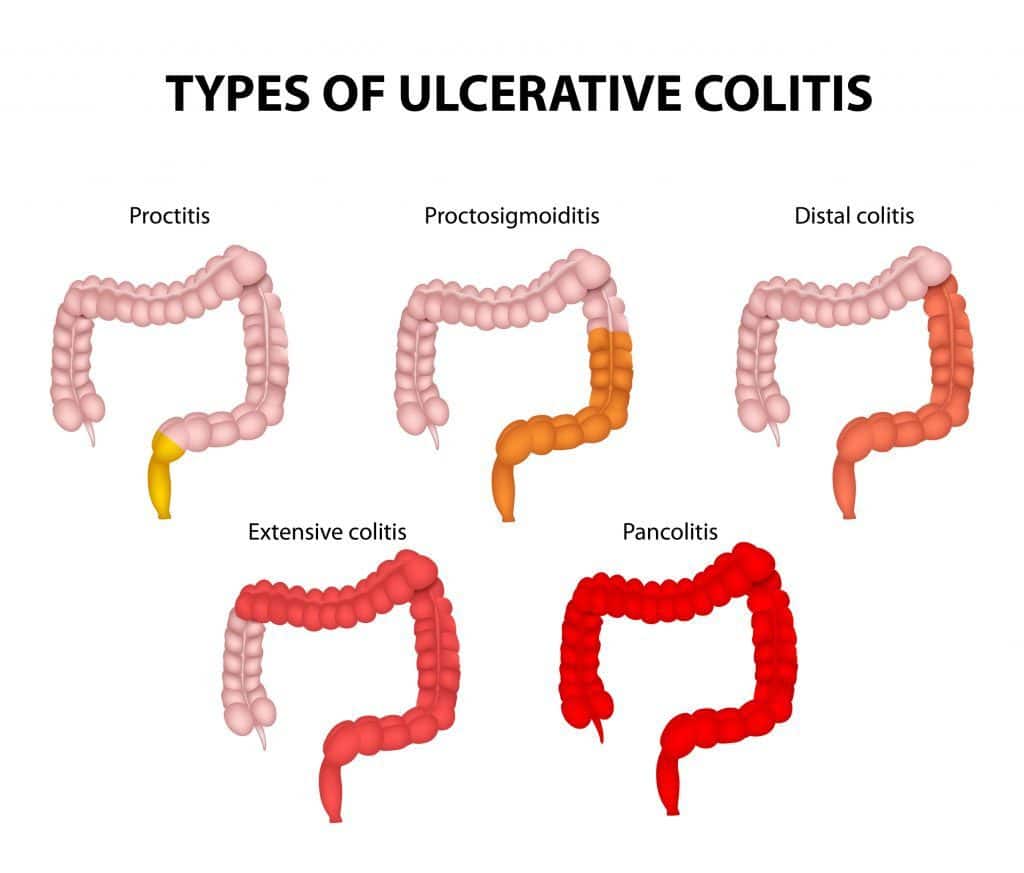
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is.
For some people, the condition has a significant impact on their everyday lives.
You May Like: What Causes Ulcerative Colitis Flare Ups
What Your Poop Means About Your Health When You Have Ibd
Content created for the Bezzy community and sponsored by our partners. Learn More
â¢â¢â¢â¢â¢
Cynthia Taylor Chavoustie, MPAS, PA-C
Medically Reviewed
â¢â¢â¢â¢â¢
â¢â¢â¢â¢â¢
â¢â¢â¢â¢â¢
Cynthia Taylor Chavoustie, MPAS, PA-C
Medically Reviewed
â¢â¢â¢â¢â¢
â¢â¢â¢â¢â¢
Whether we care to talk about it, everyone poops.
If youâre living with inflammatory bowel disease , which includes Crohnâs disease and ulcerative colitis, getting over the fear of bathroom talk isnât just about opening up about an embarrassing topic â it can actually help you manage your condition. Changes in our bowel habits can clue us into many issues related to IBD.
Hereâs the scoop on what your poop means â and when itâs time to talk with your doctor.
Why Is My Poop Coming Out Like Pebbles
Pebble like, hard poop only occurs when you are very constipated. The stool has sat in the large intestine and colon for an extended period. During this extended stay in the colon, water and nutrients are removed from the stool, causing it to harden and break apart into pebbles.
3 Related Question Answers About Lumpy Stool Pictures
Read Also: What Foods To Avoid With Peptic Ulcer
How Can I Find Support After An Ulcerative Colitis Diagnosis
When taking care of your physical well-being, dont forget that ulcerative colitis can take a toll on your emotional and mental well-being too. If it turns out your symptoms are ulcerative colitis, you can find a support group, or ask your doctor if they can connect you with a therapist or G.I. psychologist. Dr. Riehl, for example, works with patients on aspects of body image and even connects them with other patients who have experienced colectomy or ostomy . We talk openly about the impact that it can have on them from an intimacy perspective to how it impacts their self-identity, she says.
Since ulcerative colitis often starts at an age when people are thinking about their first job or starting a family, it can be particularly tough. One of the reasons that I and several of my colleagues went into this field is precisely because of thatso that we can hopefully make a difference in peoples lives early, and have them be able to lead productive and complete lives by putting their disease in remission, Dr. Sinha says.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Also Check: How To Treat Mouth Ulcers
What Is The Treatment For Ulcerative Colitis
Treatment involves medical and surgical treatment, depending on the severity of the disease. Patients would also require lifestyle changes and dietary modifications.
Medical treatment: Most patients require a combination of more than one medication. Medical treatment typically involves medications to suppress and/or modulate the immune system, painkillers, antibiotics, anti-diarrhea medications and nutritional supplements.
Surgery: Surgery can eliminate UC. It involves removing the entire colon and rectum followed by reconstruction.
Lifestyle and dietary modifications: Management of psychological stress and emotional support is important to prevent and reduce flare-ups. Moreover, regular exercise and a healthy diet are important. Doctors advise a diet with low fat, meat, vitamin B6, sulfur, and milk.
What Does Blood In Stools Look Like
Blood from your stool could look bright red, or it might be dark red or black.
How the blood looks depends on where it is coming from.
If the blood is mixed in with your stool, this suggests bleeding might be from higher up in the bowel.
If your stools are black and like tar, and they smell bad, this is also probably because the blood is coming from higher up in the bowel.
Read Also: Acute Ulcerative Colitis Treatment Guidelines
How To Fix A Crappy Situation
Theres no magical way to have perfect poops. Ultimately, controlling UC with that reduce inflammation in the GI tract and put you into remission is the best way to get your bowel movements looking more like a 3 to 5.
In the meantime, doctors recommend that you adjust your eating habits during flares to reduce diarrhea, control frequency and urgency, and bulk up stool. If youre in the middle of a bout of diarrhea, its also important to rehydrate with something thats got to avoid dehydration and potential electrolyte imbalances.
The main thing to do during a flare is to decrease food that produces a lot of gas, Dr. Higgins says. When people have an emergency, they have almost explosive stools because they have trouble even holding onto gas. A few gas-producing ingredients to avoid: simple sugars and carbonation. Putting less gas in and providing less food for the bacteria to generate more gas wont necessarily help with inflammation, but it will help with symptoms in the short-term, Dr. Higgins says.
Another thing to avoid: caffeine. It generally speeds up the intestinal transit, Dr. Higgins says, something which you dont need.
When Is The Mucus In The Stool Normal
As pointed out above, mucus is a slippery, natural substance that lines many cavities in the body. Often the mucus is not visible to the naked eye, but it is found in many body fluids.
- The mucus found in the stool is produced by cells in the lining of the digestive system. It is also found in other organs that need their uppermost cell layer to be kept moist. The mucus also serves as a layer of defense to prevent harmful germs from entering the body like those in the sinuses.
- The mucus also acts as a lubricant to these orifices, preventing them from drying out and cracking, which would make them vulnerable to attack.
- The mucus in the digestive tract helps stool pass easily through the intestine.
Note that having mucus in the body is an absolute necessity, but overproduction could indicate that there is a problem with the body.
Thus a packet of mucus in the stool, which is easily seen with the naked eye, can only be a sign of digestive problems due to the proliferation of bacteria or problems related to digestive enzymes. While this sign of increased mucus is not inherently harmful, it can serve as a clue for a more accurate diagnosis.
Recommended Reading: Can Urgent Care Treat Ulcers
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Don’t Miss: What Foods Are Good For Ulcers And Gastritis
How Do You Calm A Colitis Flare
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Read Also: Psc Liver Disease Ulcerative Colitis
What Are Ulcerative Colitis Treatment Options
Depending on the location and severity of your case of ulcerative colitis, there are different treatments that can help you feel better. For a long time, corticosteroids were the main form of medical treatment for IBD, but they can potentially have adverse effects when used long-term. With more research, options like immunosuppressants arrived. According to the Centers for Disease Control and Prevention , the newest type of medication approved for the treatment of IBD is biologics. These medications are made from living thingsrather than chemical compoundsand work to target proteins made by the immune system to reduce inflammation. If medication isnt effective, surgery is also an option.
Dr. Sinha emphasizes that keeping your health care team informed is key to managing ulcerative colitis. Having this regular communication helps facilitate labs, imaging, or endoscopy that may be necessary, he says. It also allows the providers to understand many other facets of the disease’s impact on the patient, such as the psychosocial impact.
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
Ulcerative colitis can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow as well as other kids their age and puberty may happen later than normal.
You May Like: What Will Help Stomach Ulcer Pain
What Tests Are Used To Find The Cause Of Blood In Stools
Your doctor will talk to you, examine you, and should arrange some tests to investigate the cause. The doctor will choose the right test for you based on your age, symptoms and medical history. Possible tests include:
- sigmoidoscopy a procedure where your doctor uses a camera to check inside your rectum and most of your lower large intestine
- colonoscopy a physician uses a camera that sits within a tube to examine your entire colon
- gastroscopy a tube is inserted through the mouth to look at the oesophagus, stomach and first part of the small intestine
Some of these tests are done under sedation and anaesthetic. Ask your doctor for more information.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
You May Like: What Causes Acute Ulcerative Colitis
Besides Is Lumpy Poop Good
Firm stools that are connected but still lumpy can also be a sign of constipation. This signals that your waste has hung around in the intestine long enough to become dried out, but not so long that its dry enough to break into smaller pieces, according to UnityPoint Health experts.
Pebble or pellet bowel movements arent usually a reason to worry, but they may mean stool is moving through your intestines at a slow pace
Digestive Changes In Ulcerative Colitis
Ulcerative colitis is a chronic condition, meaning it comes on slowly over a long period of time. Currently, there is no known cure for UC.
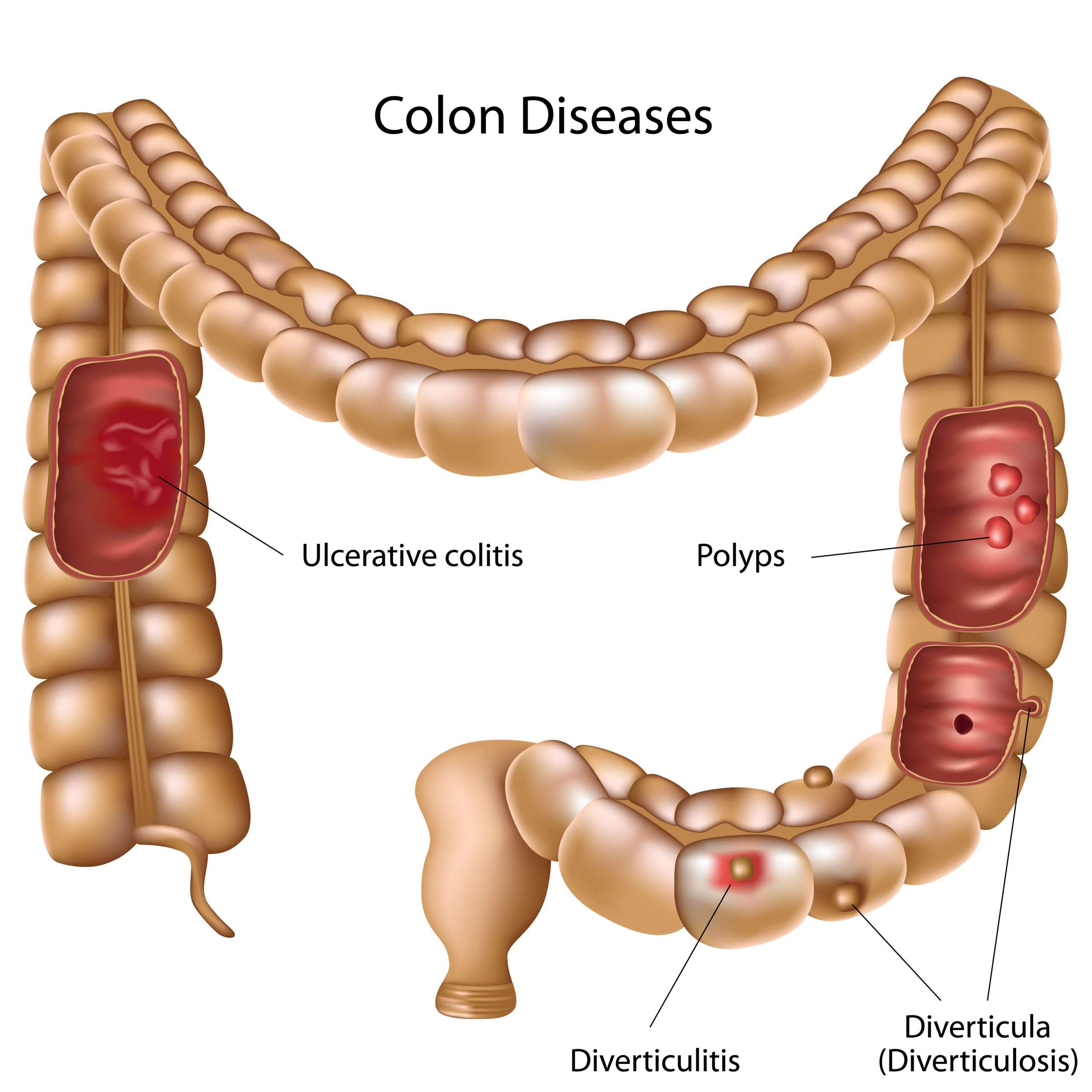
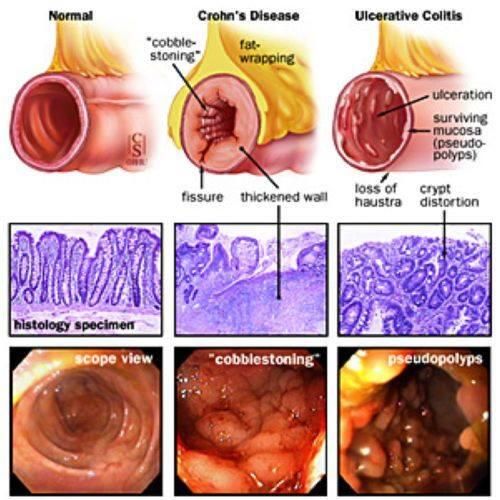
With UC, inflammation and ulcers develop on the lining of the large intestine . Sometimes the rectum is affected, as well.
This inflammation can cause changes in bowel habits, including urgency, diarrhea, blood or mucus in the stool, and abdominal pain. When your large intestine is inflamed, it contracts and empties often, which is why you may have urgent bowel movements and diarrhea.
When chronic inflammation damages the lining of your colon, ulcers can develop. The ulcers can bleed, leading to blood in your stool. If you regularly lose a lot of blood in your stool, you might develop anemia .
Though diarrhea is more common, some people with UC experience constipation. Inflammation limited to the rectum, known as ulcerative proctitis, may result in constipation.
Other symptoms of UC include painful bowel movements, nausea, vomiting, fatigue, unintentional weight loss, and fever.
Don’t Miss: Foods To Eat With Peptic Ulcer Disease
Are Probiotics Good For Dogs With Colitis
Probiotics such as FortiFlora contain live bacteria that can help heal the intestine and ease inflammation while improving the intestinal flora. Probiotics are safe to use and can be helpful for most animals that have been suffering from sporadic bouts of diarrhea or chronic colitis.
You Gotta Go Right Now
Dr. Higgins explains that a healthy rectum has a nifty stretching and storage function that allows for waste thats been produced throughout the day to be stored up. Then, when the rectum is full and its convenient for you to hit the bathroom, you can go relieve yourself.
Whats different about having a really inflamed rectum is that the walls thicken, so theres less space and they don’t stretch very well, Dr. Higgins says. Inflammation also makes the walls of the rectum very sensitive, so they detect what feels like very severe stretch even with small amounts of stool. This is what makes you get a really intense urge to gowhats known as urgency. You might have 10 to 15 seconds to get to the toilet in very severe cases, he adds.
Read Also: Ulcerative Colitis Lower Back Pain
Reducing Blood In Stools
prebiotic supplement may help reduce bloody stools and other symptoms of UC.
Participants taking the prebiotics supplement experienced significantly decreased abdominal pain and cramping. They also reported reduced nausea, vomiting, diarrhea, and blood in stools, although these effects were not statistically significant.
The study was small, so more research is needed to determine the best way to reduce blood in stools.
If a person frequently has bloody stools, a doctor may prescribe iron supplements to help prevent anemia.
What Is The Prognosis If My Dog Has Colitis
For most dogs diagnosed with colitis, the prognosis is excellent for a speedy recovery. Stress colitis is one of the leading causes of colitis in dogs. Treatment with a simple change in diet and medication to resolve the inflammation or infection in the colon is all that is required for most dogs. The majority of dogs experiencing stress colitis are back to normal within three to five days. Chronic, severe, or recurrent cases should have further diagnostic tests performed to determine the exact cause and proper treatment. For many dogs with chronic colitis, strict dietary control and careful use of medications keep the condition under control.
| Contributors: Malcolm Weir, DVM, MSc, MPH Ernest Ward, DVM |
Don’t Miss: What To Do When You Have A Stomach Ulcer
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
What Is A Normal Stool
- Color: The color of a normal stool should be medium to dark brown
- Odor: It is normal for the odor to be strong-smelling
- Texture: The texture of normal stool should be somewhere between soft and firm.
- Shape: Stool passed in a single piece or a few smaller pieces is considered normal. The shape should be long and sausage-like to match the shape of your colon.
- Frequency: The minimum bowel movements a person should pass per week is three. Normal bowel frequency is from once every other day to twice per day.
- Effort: Healthy bowel movements should be strain-free and painless
For the most part, stools vary from person to person, and you should have a good idea of what is normal for you. Most changes in bowel movements will clear up on their own in a few days, but there are some specific red flags that can indicate that there is a problem, such as Ulcerative Colitis.
Recommended Reading: Icd 10 Code For Ulcerative Colitis With Bleeding