Differentiating Lower Extremity Wounds
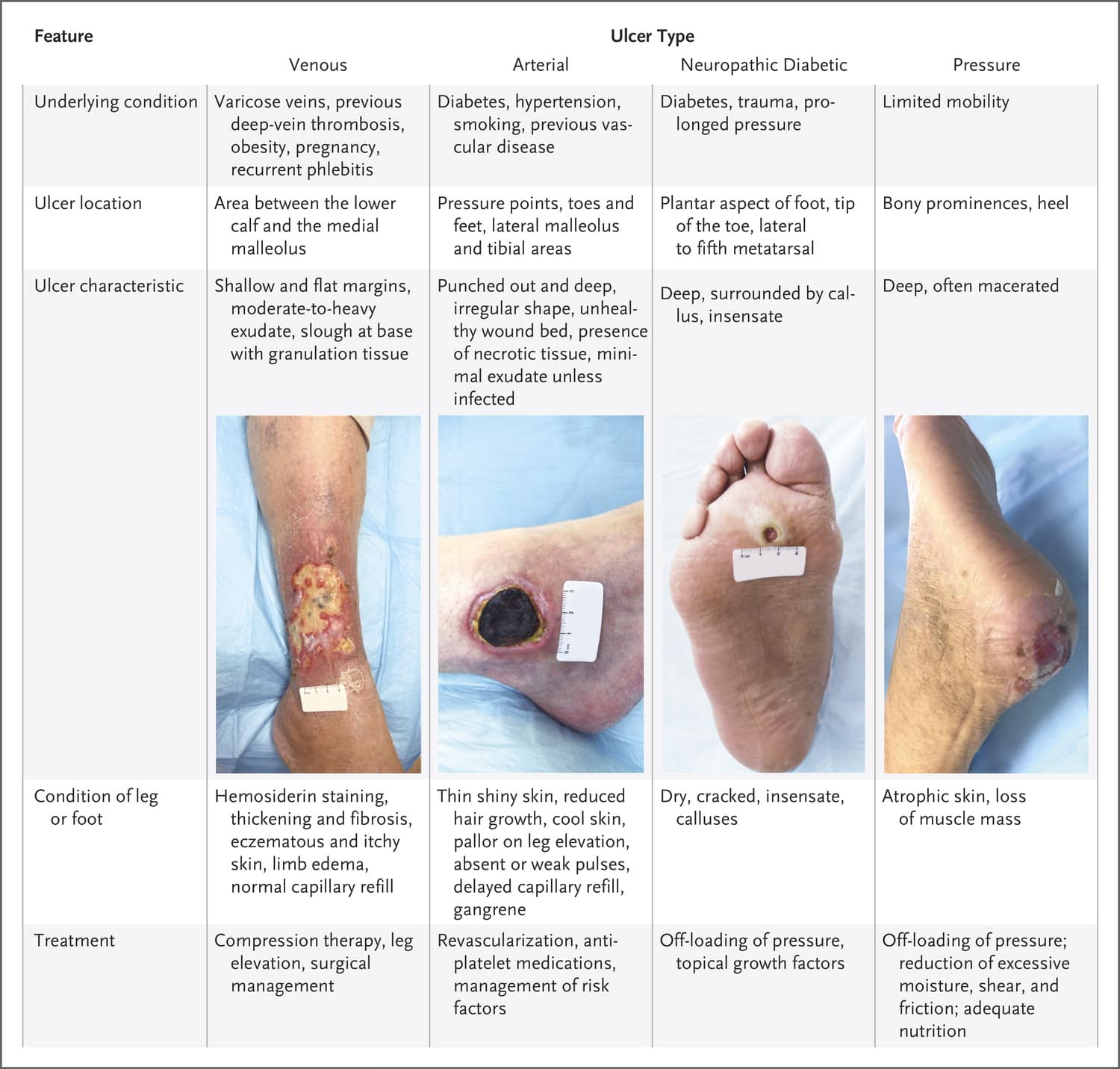
Understanding other lower extremity woundsarterial ulcers, neuropathic ulcers, and pressure injuriescan help nurses differentiate them from venous ulcers. A detailed clinical history and thorough assessment when evaluating lower extremity ulcers can aid diagnosis and guide treatment, which may differ depending on the type of ulcer.
Treatments for some types of wounds may be harmful for others. For example, if compression therapy is applied to a limb with arterial insufficiency that resulted in an arterial ulcer, blood flow can be reduced further, potentially leading to amputation.
Arterial ulcers
Arterial ulcers are small, have an irregular shape, and appear punched-out with a deep base. Typically, necrotic tissue is present with low exudate unless the wound is infected. The ulcers usually are located over the pretibial area, the lateral malleolus , or on the toes or heel.
Most patients report severe pain thats relieved when the extremity is placed in a dependent position and increased when the extremity is elevated. Assessment findings include abnormal distal pulses, cold extremities, and prolonged venous filling time. Arterial ulcers may be caused by tissue ischemia resulting from atherosclerosis.
Arterial vs. venous ulcer
The following table compares venous and arterial ulcers, which can occur as a result of peripheral vascular disease.
| Arterial |
Neuropathic ulcers
Pressure injuries
Causes Of Venous Leg Ulcers
Venous leg ulcers occur when the one-way valves of the veins fail to maintain the blood flow toward the heart and prevent any back flow. This problem with blood flow is known as venous insufficiency. The venous system in the lower limbs includes the deep, superficial and profound veins where the deep veins lie between the muscles, the superficial veins in the upper layers just below the skin, and the profound veins are located in between, connecting the other two types of veins. In damaged valves, the blood backs up and pools in the veins, building up pressure, which prevents nutrients and oxygen in the blood from reaching the body tissue. Eventually, the tissue breaks down and forms an ulcer.
Caring For Venous Ulcers
Venous ulcers need proper care and treatment to prevent infection and to heal. It’s important to have any venous ulcers checked right away by your healthcare provider.
Treatment may require focusing on the circulatory or vein problems that are causing the ulcers. Or it may mean removing some tissue around the wound. You may be asked to:
-
Clean the wound regularly
-
Apply a dressing to the ulcer
-
Avoid products that cause skin sensitivity
-
Wear compression stockings to prevent blood from pooling in the legs and to speed healing
-
Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
-
Take oral antibiotic medicines to prevent or treat an infection
-
Have allergy testing done
Wearing a compression wrap to keep blood flowing back up to your heart can also help ulcers heal more quickly. In some cases, surgery or a skin graft is needed to close up the opening in the skin.
Recommended Reading: Best Mattress For Pressure Ulcers
Rapid Wound Closure In 34 Days
Complete wound closure, defined as being fully epithelialized, was achieved among 11 patients and 13 wounds within a median of 34 days. The three remaining patients were unavailable for follow-up because one of them moved out of the country, and two died of unrelated reasons. However, those three wounds also demonstrated progressive healing when last seen. There were no significant adverse reactions in any patients.
These positive outcomes are the result of potentiation and synergy between cannabinoids, terpenes, and flavonoids, the scientists conclude.
The rapid wound closure of previously non-healing venous leg ulcers among elderly and highly complex patients suggests that topical cannabis-based medicines may become effective adjuvants in conjunction with compression therapy. It may also indicate that they may have an even broader role within the skin and wound management.
Sasha Bajilo
Topical Antimicrobials And Antiseptics

In chronic wounds, reduction of certain microbial species, such as anaerobic bacteria in order to limit undesirable odors or perhaps mixed communities of four or more bacterial species that impede healing, use of topical antibiotics may be justified .
Various studies on dressings incorporating antibiotics and antiseptics are reviewed, but no single consensus for any particular topical agent could be made. This is partly due to the different mechanism and spectrum of action of the antimicrobials. The most frequently used topical antimicrobials in wound care practice are chlorhexidine, iodine, silver containing products, mupriocin and fucidic acid. In the past, acetic acid, honey, hydrogen peroxide, sodium hypochlorite, potassium permanganate, and proflavine have been used.
Don’t Miss: How To Treat Peptic Ulcer Disease
What Is Daily Life Like With A Venous Ulcer
While youre undergoing treatment, there are steps you can take to promote healing. These include:
- Eating a healthy diet, which supports your bodys natural healing abilities.
- Keeping the ulcer and nearby skin clean.
- Periodically raising your legs when seated to avoid blood pooling.
- Staying active with gentle exercises, like walking.
A note from Cleveland Clinic
Venous stasis ulcers are wounds that are slow to heal. They typically occur in people with vein issues. Timely specialized care is necessary to prevent complications, like infections that can become life-threatening. Nonhealing ulcers also raise your risk of amputation. Venous ulcers can come back after treatment, which is why care often includes preventive therapies. Most people make a full recovery. But its essential to follow all care instructions.
Causes Of Venous Ulcers
Venous ulcers most often form around the ankles.
Venous ulcers typically occur because of damage to the valves inside the leg veins. These valves control the blood pressure inside the veins. They allow it to drop when you walk. If the blood pressure inside your leg veins doesn’t fall as you’re walking, the condition is called sustained venous hypertension. That increase in blood pressure causes ulcers to form on your ankles.
Venous ulcers may also be caused by other problems with your leg veins. These include:
-
Varicose veins. These are large, bulging leg veins. They occur when valves in the leg veins dont work well, allowing blood to collect in the lower leg.
-
Chronic venous insufficiency. Like varicose veins, this condition occurs when your leg veins cant pump blood back up to your heart. Blood then pools in your lower legs, causing your legs to swell. Since the blood can’t flow well in your legs, the swelling may be extreme. This extreme swelling can put so much pressure on your skin that venous ulcers form.
You May Like: Foods For Acid Reflux And Ulcers
Prevention Of Venous Leg Ulcers
To help prevent venous leg ulcers, these measures may be followed:
- Avoid long periods of standing or sitting
- Raise the legs above the heart and use compression socks as often as possible
- Maintain a healthy lifestyle that includes regular moderate exercise, a healthy diet and reduce body weight, if overweight
- Quit smoking, reduce alcohol consumption and try to stay active
- Inspect the lower limbs daily and look for any color changes or cracks in the skin
RELATED ARTICLES
Wound Dressing And Care
A venous leg ulcer is an open sore that can catch an infection from microbes very quickly. It is important to keep it clean at all times. Advanced Wound Care Dressings can help keep them free from infection as well as aid in faster wound healing. After dead tissue is removed and the wound is cleaned, it should be covered with a light, wound healing dressing. This can be easily done at home by following the instructions of a wound specialist regarding the method of cleaning and the number of dressings required.
Recommended Reading: How To Cure Ulcer Naturally
What Venous Ulcer Treatments Might I Need
The therapies that are best for you depend on the location and severity of the ulcer. Care typically includes frequent follow-up appointments to ensure treatments are working.
Venous ulcer treatments often include:
- Antibiotics if theres an infection.
- Compression bandages or stockings to improve circulation.
- Ointments that protect against germs.
- Pain relievers and other therapies to quiet overactive nerves.
- Procedures to remove debris and dead tissue.
- Referrals to specialists if you need help managing chronic conditions, such as diabetes.
- Special bandages and dressings to keep the ulcer covered.
- Wound cleaning daily to flush out bacteria and remove dead tissue.
Venous Leg Ulcers Are Painful Distressing And Affect Quality Of Life
Venous leg ulcers are painful, distressing and have a considerable impact on quality of life. Research into how pain can be better controlled in people with venous leg ulcers, and how quicker healing can be promoted, were among the Venous Top 10 Priorities identified by the NIHR James Lind Alliance Priority Setting Partnership Vascular conditions in 2021, while the Wounds Top 10 included questions about how to improve quality of life and about the best way to manage complex, hard to heal, leg ulcers.
Also Check: What Are The Signs Of Having A Stomach Ulcer
Cbd For Venous Leg Ulcers: The Treatment
Great results obtained in this study on CBD for venous leg ulcers resulted with the following methodology:
Treatments were carried out every second day and continued until complete wound closure,defined as the wound bed being 100% epithelialized. On their initial visits, all patients degrees of global medical complexity was calculated using both the M3 multimorbidity index tool and the Palliative Performance Scale score . Qualitative clinical assessments of their degrees of lipodermatosclerosis, edema, and peripheral arterial disease were also scored and documented. Following gentle cleansing with sterile normal saline, each patient underwent application of evenly applied thin layers of VS-12 to the wound beds, and VS-14 to a 4-6 cm radial cuff of peri-wound integument every second day. Tissues were then covered with one layer each of Jelonet and Mesorb. This was followed by the application of inelastic compression bandages, chosen based upon patient preferences, using a spiral technique, between the level of the metatarsal phalangeal joints and the infra-popliteal space.
Exudate In Venuous Leg Ulcer
Patients with venous leg ulcers generally have an increase in wound exudate when compared with patients with other forms of chronic skin ulcers . Poor management of wound exudate can have a negative effect on patient quality of life and is associated with damage to the wound bed and peri-wound region, increased risk of infection, delayed wound healing, and increased costs to health services .
The most important factor in reducing exudate levels is appropriate sustained compression therapy, not the dressing .
Read Also: Ulcerative Colitis How Much Blood Is Too Much
How Venous Leg Ulcers Are Treated
Most venous leg ulcers heal within 3 to 4 months if they’re treated by a healthcare professional trained in compression therapy for leg ulcers. However, some ulcers may take longer to heal, and a very small number never heal.
Treatment usually involves:
- cleaning and dressing the wound
- using compression, such as bandages or stockings, to improve the flow of blood in the legs
Antibiotics may also be used if the ulcer becomes infected, but they don’t help ulcers to heal.
However, unless the underlying cause of the ulcer is addressed, there’s a high risk of a venous leg ulcer recurring after treatment. Underlying causes could include immobility, obesity, previous DVT, or varicose veins.
Signs Of An Infection
A venous leg ulcer can be susceptible to bacterial infection. Symptoms of an infected leg ulcer can include:
A number of factors can increase your risk of developing a venous leg ulcer, including:
- obesity or being overweight this increases the pressure in the leg veins
- if you have difficulty walking this can weaken the calf muscles, which can affect circulation in the leg veins
- previous deep vein thrombosis blood clots that develop in the leg can damage valves in the veins
- varicose veins swollen and enlarged veins caused by malfunctioning valves
- previous injury to the leg, such as a broken or fractured bone, which may cause DVT or impair walking
- previous surgery to the leg, such as a hip replacement or knee replacement, which can prevent you from moving about
- increasing age people find it harder to move around as they get older, particularly if they suffer from arthritis
You May Like: Can I Donate Blood If I Have Ulcerative Colitis
Management Of Patients With Venous Leg Ulcers
It is well documented that the prevalence of venous leg ulcers is increasing, coinciding with an ageing population. Accurate global prevalence of VLUs is difficult to estimate due to the range of methodologies used in studies and accuracy of reporting.1 Venous ulceration is the most common type of leg ulceration and a significant clinical problem, affecting approximately 1% of the population and 3% of people over 80 years of age2 in westernised countries. Moreover, the global prevalence of VLUs is predicted to escalate dramatically, as people are living longer, often with multiple comorbidities. Recent figures on the prevalence of VLUs are based on a small number of studies, conducted in Western countries, and the evidence is weak. However, it is estimated that 93% of VLUs will heal in 12 months, and 7% remain unhealed after five years.3 Furthermore, the recurrence rate within 3 months after wound closure is as high as 70%.4-6 Thus, cost-effective adjunct evidence-based treatment strategies and services are needed to help prevent these ulcers, facilitate healing when they occur and prevent recurrence.
Other Treatments For Venous Leg Ulcers
Cochrane Reviews of several other treatments have highlighted large gaps in the evidence.
The Cochrane Review Therapeutic ultrasound for venous leg ulcers found that it is unclear whether therapeutic ultrasound improves ulcer healing and the review authors say that any effect is likely to be small. There is a Cochrane Clinical Answer on this review: For people with venous leg ulcers, how does therapeutic ultrasound affect outcomes?
The authors of the Cochrane Review Electromagnetic therapy for treating venous leg ulcers concluded that It is not clear whether electromagnetic therapy influences the rateThe speed or frequency of occurrence of an event, usually expressed with respect to time. For instance, a mortality rate might be the number of deaths per year, per 100,000 people. of healing of venous leg ulcers.
The role of Subfascial endoscopic perforator surgery for treating venous leg ulcers also remains uncertain.
There were no randomisedRandomization is the process of randomly dividing into groups the people taking part in a trial. One group will be given the intervention being tested and compared with a group which does not receive the intervention . trials meeting the criteria for inclusion in the Cochrane Review Extracorporeal shock wave therapy for the healing and management of venous leg ulcers .
You May Like: Humira Treatment For Ulcerative Colitis
For Ulcers Caused By Varicose Veins
A UK multi-centre randomised controlled trial, EVRA, found that For patients with leg ulcers caused by varicose veins, early interventionA treatment, procedure or programme of health care that has the potential to change the course of events of a healthcare condition. Examples include a drug, surgery, exercise or counselling. to treat the veins results in faster healing of ulcers than standard compression therapy alone . It also increases ulcer-free time and is highly likely to be cost-effective.
Treatment Options For Venous Leg Ulcers
Treating a venous ulcer is based on the status of circulation. Better circulation leads to easier treatment, better healing and fewer complications. Treatment can include raising the legs above the heart level as often as possible and wearing compression socks. These measures can improve circulation and prevent blood from pooling in the veins. Regular walking and exercising are also recommended to help improve circulation and encourage healing. Another important medical intervention is to treat the underlying cause of a venous ulcer, which may include improving the management and control of any chronic illnesses that are present.Sometimes extensive wound cleansing is needed. Antibiotics can be given orally or applied directly on the ulcer, along with a wet dressing or drying agents, as appropriate. In some cases, a graft is used to cover the ulcer to heal it.
Don’t Miss: How To Reduce Ulcer Pain
Wound Care & Hyperbaric Medicine Specialists Located In Dallas Tx Fort Worth Tx Overland Park Ks San Antonio Tx The Woodlands Tx & Little Rock Ar
The importance of identifying venous leg ulcers early and seeking professional treatment cant be emphasized enough. Venous ulcers are extremely difficult to heal, with half of all cases remaining open and unhealed for nine months or longer. The skilled team at Wound Evolution in Fort Worth, Dallas, San Antonio, Texas, and Overland Park, Kansas, offers holistic wound care, including advanced therapies that help your venous leg ulcer heal. At the earliest sign of an ulcer, call or book an appointment online.
Management Of Venous Leg Ulcers
- Corner stone of venous ulcer management.1,2,3 High compression is better than low, and low compression is better than none the best compression is the one the patient will wear.
- Compression therapy helps reduce the ambulatory venous pressure it improves the calf muscle pump function and decreases reflux in the malfunctioning veins,1 reducing edema.
- As edema is reduced in legs, a new compression system may be required based on size of limb do not fit for a compression garment until compression wraps have been used to decrease edema.
Compression therapy systems1,2:
Always provide instruction to patients to remove compression wrap if adverse reactions occur .
Cleansing
- Wash both legs with pH-balance soap and water1 every time compression wrap is removed, or instruct patient to cut off compression wrap and have a shower in which they wash leg prior to homecare visit.1
- After washing legs, moisturize legs with unscented or perfumed moisturizer.1
- Cleanse ulcer with at least 100 ml of cleansing solution with a PSI of 8-15 .
- Pat dry excess fluid and apply barrier to peri-wound skin, if required.
Debridement
- Removal of necrotic tissue from wound bed, select the debridement method most appropriate for the patient, situation and environment of care.
Dressings1,3
You May Like: Can Stomach Ulcers Cause Blood In Stool