Ibd And Liver Disease
Inflammatory Bowel Disease is often associated with other diseases that develop alongside intestinal and perianal involvement. These other diseases are called extraintestinal manifestations of IBD. Extraintestinal organ systems that may be involved with IBD are listed in below. The associations of these manifestations with IBD have been recognized for many years but are not well known in terms of the mechanisms, or cellular changes that occur in the development of the disease.
Risk Factors For Fatty Liver Disease
NAFLD is a condition of increased accumulation of fat in the liver from causes other than alcohol consumption, according to the Inflammatory Bowel Diseases study. It’s associated with metabolic risk factors, such as abdominal obesity, insulin resistance, and hypertension. Previously, wed see IBD patients that were thin and werent able to gain weight because of their disease, but now we see people with both obesity and IBD, much more than previously, says the lead author of the study, Bincy Abraham, MD, the director of the inflammatory bowel disease program at Houston Methodist Hospital in Texas.
A population study published in May 2019 in the journal Gastroenterology identified nearly 160,000 patients with Crohns disease. Of those, just 2.4 percent had NAFLD and less than 1 percent had nonalcoholic steatohepatitis , a specific type of NAFLD in which a buildup of fat causes inflammation and damage to liver cells. Still, nearly half of all patients who had both CD and NAFLD were obese, and 60 percent of people with both CD and NASH were obese. When compared with people who have CD but not NAFLD, patients who had both diseases were much more likely to also have diabetes, hypertension, or to be obese. According to a study published in May 2018 in the Indian Journal of Endocrinology and Metabolism, 70 percent of people who have type 2 diabetes also have NAFLD.
Practical Takeaways And Future Directions
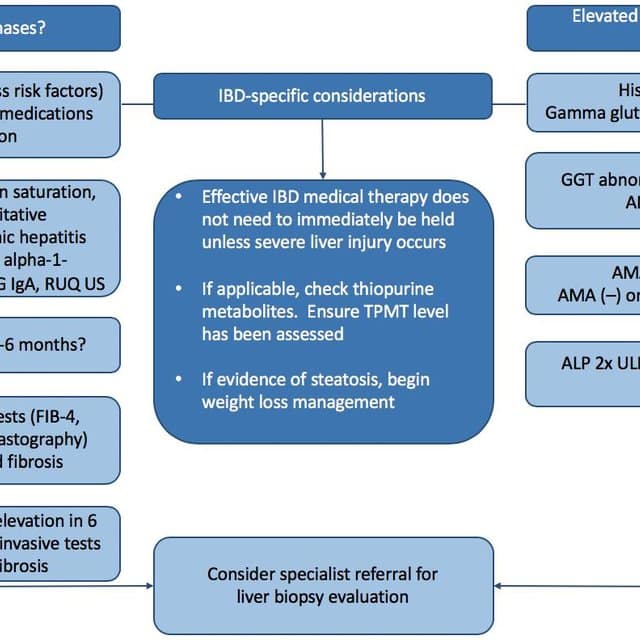
Regarding the findings clinical applications, we need to recognize that fatty liver disease is common in IBD, Dr. Regueiro says. This is particularly important as we monitor patients for liver disease and prescribe medications that are metabolized by and may affect the liver.
We should screen regularly for liver disease in our IBD patients, at least with liver function blood tests, he says. In the future we may use imaging modalities or other biomarkers to assess for liver disease in our IBD patients.
Going forward, Dr. Regueiro and team are launching a large, prospective study to evaluate the phenotype of IBD patients at Cleveland Clinic.
One goal is to understand the -omics of their disease, he says. Were interested in looking for disease patterns through big data and natural language processing, and applying translational research in proteomics, metabolomics, genomics, microbiomics, and immunologic processes to our patients.
Were hoping that these discoveries will lead to precision medicine for our patients and better treatment.
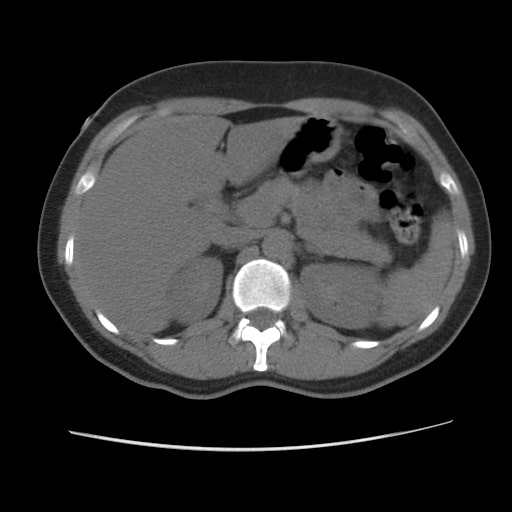
Histological image of nonalcoholic cirrhosis courtesy of Lisa M. Yerian, MD.
Don’t Miss: Over The Counter Drugs For Ulcers
Univariate And Multivariate Analyses
To assess whether LTA is an independent risk factor for developing complicated disease behaviour, we performed univariate and multivariate analyses. The univariate analysis identified the presence of LTA, location of disease, and CRP as risk factors for developing complicated disease behaviour.
Table 2 Univariate analysis for the LTA and development of complicated disease behaviour and hospitalizations
The multivariate analysis showed that the presence of LTA was associated with a higher risk of developing complicated disease behaviour, as were ileal location and isolated upper disease, whereas CRP at diagnosis was not .
Table 3 Multivariate analysis for the LTA and development of complicated disease behaviour
Using the multivariate analysis, the presence of LTA and the presence of B2 behaviour were found to increase the risk of hospitalizations. Patient age at diagnosis > 17 years reduced the risk of hospitalization . B3 behaviour , sex , and BMI did not influence the risk of hospitalization.
For surgery, when all patients were analysed, the presence of complicated disease behaviour at diagnosis was identified as a risk factor.
However, when patients with complicated disease behaviour at diagnosis were excluded, the presence of LTA and either ileal or upper GI location were associated with a higher risk of surgery.
Rate Of Liver Disease Twice As High In Ulcerative Colitis Patients
Study from DDW 2019 found that rates of nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, and nonalcoholic cirrhosis was more than double in patients with UC.
Benjamin Click, MD
Patients with ulcerative colitis may be at an increased risk of nonalcoholic fatty liver disease , nonalcoholic steatohepatitis and nonalcoholic cirrhosis , according to a study presented at Digestive Disease Week 2019.
In an analysis of more than 62,000,000, investigators from the Cleveland Clinic found that prevalence rates of NAFLD, NASH, and NC among patients with UC were more than double that of the general population.
After observing what appeared to be an increasing prevalence of liver disease in patients with UC in their own practices, investigators sought to determine if UC patients were at an increased risk of NAFLD, NASH, and NC.
“It’s becoming an increasingly common finding in my clinical practice, it’s also increasingly recognized that with ulcerative colitis the increased gut permeability and the inflammation that goes along with the disease process, as well as the medication we use that carry certain hepatotoxicity, may convey an increased risk for chronic liver disease in our patient populations,” explained Benjamin Click, MD, study author and associate staff gastroenterologist at the Cleveland Clinic in an interview with MD Magazine.
Related Content:
Recommended Reading: Prednisone Dosage For Ulcerative Colitis Flare Up
Motivation For The Studies
Some concerning trends prompted the research. Fatty liver disease is increasing in prevalence in the United States and we were interested in determining if IBD is a separate risk factor for nonalcoholic fatty liver disease , Dr. Regueiro says.
We know that IBD has been associated with primary sclerosing cholangitis, and that many of the medications we prescribe affect the liver. However, he adds, the contribution of IBD to NAFLD is not known and we hypothesize may be an underrecognized extra-intestinal manifestation of IBD.
To find out more, Dr. Regueiro, lead author Muhammad Talal Sarmini, MD, and their colleagues studied diagnosis codes in Explorys Inc. electronic medical records. This commercial database covers 26 major integrated healthcare systems nationwide.
From more than 62 million patients, they identified 159,290 people diagnosed with Crohns disease and 125,380 diagnosed with ulcerative colitis between 1999 and 2018. Next, the researchers looked for people with newly diagnosed NAFLD, nonalcoholic steatohepatitis or nonalcoholic cirrhosis more than 30 days following their CD diagnosis.
Albumin And Prothrombin Time Assessment: Are We Really Testing Liver Function
Determining serum albumin levels and assessing prothrombin time are often considered tests of liver function. This is mainly because hepatic synthesis of albumin tends to decrease in end-stage liver disease, and an increase in prothrombin time depends on the decreased synthesis of liver-derived coagulation factors. In fact, albumin is produced by hepatocytes, and prothrombin time depends on the activity of clotting factors I, II, V, VII and X, which are produced in the liver. However, neither test is specific for liver disease, since albumin serum levels may decrease in patients with nephrotic syndrome, malabsorption or protein-losing enteropathy, or malnutrition, and prothrombin time may be prolonged by warfarin treatment, deficiency in vitamin K and consumptive coagulopathy.1,4,5,82 The finding of hypoalbuminemia and no other alterations in liver tests virtually rules out the hepatic origin of this abnormality.
You May Like: How To Treat A Diabetic Foot Ulcer On The Sole
Mild Increase In Aminotransferase Levels
A minimal or mild increase in aminotransferase level is the most common biochemical alteration encountered in everyday clinical practice. In addition to considering the when and where of the alterations, there is a series of first-line tests that can be performed on all patients because of their clinical relevance and the high prevalence of the diseases screened by these tests . Extrahepatic causes of aminotransferase alteration should be ruled out by considering the clinical context of enzyme abnormality. Although some reviews dealing with liver enzyme alteration suggest repeating tests as a first measure in order to rule out laboratory error, we do not feel that a second, normal result is enough to exclude the presence of disease, and we recommend that a first-line, clinically guided screening for the most prevalent causes of chronic liver disease be started together with repetition of the test . In fact, chronic hepatitis C infection is characterized by a pattern of aminotransferase levels fluctuating around the upper reference value. For patients who are taking drugs known to cause liver injury or who have evidence of alcohol abuse, a second, confirmatory check of aminotransferase levels after alcohol or the medication has been stopped can be a suitable option patients who have evidence of alcohol abuse also need to be carefully assessed for the risk of underlying chronic damage.
A Review Of Liver Disorders In Inflammatory Bowel Disease
Niraj James Shah
Department of Medicine, Division of Digestive Diseases, The University of Mississippi Medical Center, USA
Nitin K Gupta
Director of inflammatory Bowel Disease, School of Medicine, Department of Medicine, Division of Digestive Diseases, The University of Mississippi Medical Center, USA
Brian B Borg
Director of Hepatology, Medical Director of Liver Transplant, School of Medicine, Department of Medicine, Division of Digestive Diseases, The University of Mississippi Medical Center, USA
DOI: 10.15761/CCRR.1000352.
Also Check: What To Eat To Help Ulcers
Fatty Liver Disease And Crohns
Fatty liver disease is the most common liver complication for people with Crohnâs. There are two kinds: alcohol-related fatty liver disease and nonalcoholic fatty liver disease. It develops when extra fat is deposited in the liver. Your doctor may recommend weight loss and better control of your blood cholesterol levels to help your body get rid of the extra fat in your liver.
Liver Conditions Linked To Ulcerative Colitis
There’s more than just proximity between your colon and your liver. Find out about ulcerative colitis and liver disease risks.
Yaroslav Danylchenko/Stocksy Everyday Health
Liver disease can be a complication of inflammatory bowel disease , such as ulcerative colitis or Crohns disease. The liver, which processes the food you ingest, can develop inflammation if IBD isnt treated appropriately. Unfortunately, some drugs used to treat IBD may also damage the liver.
According to a study published in 2019 by the American Gastroenterological Association, the prevalence of nonalcoholic liver diseases in patients with UC was more than double that of the general population. Considering the increased risk, it makes sense to take precautions. Laura Raffals, MD, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota, recommends that people with UC have their liver enzymes checked annually. Its also wise to be aware of the common symptoms of liver disease so you can address the problem before it gets worse. According to the Crohns & Colitis Foundation, these symptoms include the following:
- Fatigue or low energy
- Pain or a feeling of fullness in the upper right abdomen
- Fluid retention
Here are five conditions related to the liver or ducts that transport bile that may develop alongside ulcerative colitis.
Don’t Miss: Low Dose Aspirin Ulcerative Colitis
Liver Function Test Alteration
The transient or persistent elevation of liver tests is frequent in IBD. In a recent study of 306 patients with IBD, 19.6% presented with abnormal liver test results.5 In up to 60.0% of the patients the alterations were mild and spontaneously returned to normal values. The most frequent cause of transient alteration in liver tests is secondary to DILI , while fatty liver is the most frequent cause of persistent transaminase alteration and even chronic liver disease .1
Characterization Of Study Cohort
Among 497,404 participants in the UK biobank, we identified 2377 individuals with CeD, 1738 with CD and 3684 with UC . The CeD or UC cohorts were slightly older than controls and the CD cohort. 65% of individuals with CeD and 48% of the UC cohort were female compared to 54% of controls . Participants from all disease subgroups reported lower average alcohol consumption than controls. Individuals with CeD and CD had a lower average BMI than controls .
You May Like: What Is Severe Ulcerative Colitis
Damage To The Bile Ducts And The Gallbladder
Liver-related complications tied to your Crohnâs diagnosis can also affect bile ducts and your gallbladder. Those organs all work together with your digestive tract. Bile ducts are thin tubes that go from the liver to the small intestine. They deliver a fluid called bile to help your small intestine digest the fats in food.
Primary sclerosing cholangitis affects the bile duct system of the liver. It is uncommon in people with Crohnâs: Less than 3% of people with Crohnâs have it. But it can be very serious. Inflammation causes scarring within the bile ducts and can lead to liver damage. If severe scarring of the liver happens, which is called cirrhosis, you might need a liver transplant.
Complications of PSC include infection of the bile ducts and cancer of the bile duct system. People with PSC are also at a higher risk for colon cancer, so your doctor may recommend yearly colonoscopies.
Gallstones are common in patients with Crohnâs disease. Instead of staying liquid until it is needed for digestion, bile sometimes hardens to form stones within the gallbladder. These gallstones block the ducts that bile is supposed to travel through. This can cause pain, nausea, and vomiting. Your doctor may recommend surgery to remove the gallbladder.
Symptoms Of Liver Complications With Crohns Disease
Often people with Crohnâs disease who also have liver damage may not be aware of any additional symptoms. Usually the first and only sign of a liver problem is found in routine blood tests. But tell your doctor if you:
- Have low energy or fatigue
These symptoms may be signs of advanced liver damage.
Don’t Miss: Is There A Cure For Ulcers
When To Get Help For Liver Pain
Symptoms such as pain in the upper right side of the abdomen, itching, jaundice, and fever could be an alert for a potential liver complication, says David Bernstein, MD, chief of hepatology at Northwell Health in Manhasset, New York. If you experience these issues, contact your doctor for an evaluation. Blood tests can usually confirm liver disease, but additional testing using an ultrasound, X-ray, or liver biopsy may be necessary to make a specific diagnosis. Treatment may include vitamin supplementation and modifying your diet to prevent nutrient deficiencies.
Additional reporting by Agata Blaszczak-Boxe.
Ulcerative Colitis And Liver Enzymes Elevated
12/21/2016 · Liver disease can be a complication of inflammatory bowel diseases , such as ulcerative colitis or Crohns disease. The liver, which processes the food you ingest, can develop
3/25/2013 · Moving past raised liver enzymes along with UC . My specialist has noticed that my blood results have shown really high levels of liver enzymes , and they have consistently risen each time Ive had blood tests Ive had an ultrasound on my liver
7/30/2007 · Proportion of Patients with Elevated Aminotransferases Observed in Clinical Trials with Crohns Disease and Ulcerative Colitis Open in new tab Patients with symptoms or signs of liver dysfunction should be evaluated for evidence of liver injury.
10/18/2008 · Ulcerative Colitis New Topic Reply Previous Thread Id cut back if you can at least until you find out which liver enzymes are elevated and why. Or until perhaps they start lowering on their own or due to improvements in areas of stress, diet or alcohol intake. Make sure your doctor does bloodwork regularly to see whether they are going up
7/1/2012 · Introduction The association between primary sclerosing cholangitis and ulcerative colitis is well recognised. The prevalence of PSC in patients with UC has been reported widely and ranges from 2.4% to 7.5%. The mean annual incidence rates were between 0.9 and 1.3 cases per 100 000 person years. Patients with UC may frequently be found to have abnormal liver biochemistry.
You May Like: Diet Plan For Ulcerative Colitis Flare Up
Causes Of Cirrhosis Of The Liver
In people with IBD, cirrhosis could be caused by autoimmune hepatitis or primary biliary cirrhosis. Autoimmune hepatitis is associated with a dysfunctional immune system. Primary biliary cirrhosis is an inflammation of the bile ducts that can inhibit bile from leaving the liver and going to the small intestine. When the bile gets backed up it can cause further damage to liver tissues. Primary sclerosing cholangitis, which is largely associated with ulcerative colitis, can also overlap with autoimmune hepatitis .
Relation Between The Presence Of Lta At Diagnosis And The Disease Course Of Crohns Disease
In total, 27% of patients developed complicated disease behaviour during 5 years of follow-up. Twenty-three percent had surgery for CD, and 42% of patients were hospitalized during the first 5 years of follow-up after diagnosis.
In patients with LTA, 33.6% developed complicated disease behaviour, compared to 14.7% of the patients without LTA . Similarly, patients with LTA were significantly more often hospitalized. Although the number of patients undergoing surgery did not differ between groups, the type of surgery did differ between groups: more often, a small bowel resection was performed in LTA patients.
Suppl. Table 4 shows the relationship between each liver test and the risk factor for developing complicated disease behaviour, hospitalization, and surgery. Whereas GGT was elevated most often, an elevated level of AP was associated with an increased risk of complicated disease or hospitalization. In Suppl. Table 5, we show that the risk for patients with two abnormal liver tests of developing complicated disease behaviour was higher than that for patients with one abnormal test. However, the presence of more than two abnormal tests did not further increase the risk.
Fig. 1Fig. 2Fig. 3
You May Like: Ulcerative Colitis Bleeding No Pain