What About Other Supplements For Treating Ibd
Prebiotics, probiotics, fish oil, and flaxseed oils may be helpful. More testing still needs to be done. Some patients have found that these help maintain a healthy gut or reduce symptoms. Others do not see any changes in their symptoms.
Prebiotics are a type of fiber that helps keep the bowels healthy. These promote the friendly bacteria in the gut. Onions, garlic, bananas, asparagus, avocado, and some whole grain cereals are good food sources of this fiber.
Probiotics are living bacteria that keep your gut healthy. They are referred to as the good germs. You can find them in products like yogurt and the label will say Live, Active Cultures. The brand, VSL #3 can help those with ulcerative colitis and pouchitis.
Vitamin D: Low Vitamin D may cause more severe IBD which puts patients at an increased risk for surgery, hospital stays, colon cancer, and C-diff infection. Taking a vitamin D supplement improves disease activity and quality of life.
contain omega-3 fatty acids that may help IBD symptoms. If your body can handle fish, try eating fish like salmon, cod, and tuna several times a week. You can also find fish oil and flaxseed oil in capsule form.
Turmeric or curcumin can act as an anti-inflammatory. Eating the spice in food or a capsule form may be helpful.
Talk to your doctor before starting any supplement.
To find out more about IBD, visit:
Is There Any Diet That Helps Ibd
Yes, an all-liquid diet of nutrients, called an elemental diet, has been shown to reduce inflammation in the intestines. However, most people cannot tolerate it because it is given overnight through a tube that runs through the nose to the stomach. There are other diets that reduce the amount of different types of sugars that cause bacteria to create gas in the intestine, which can lead to a lot of symptoms of pain, bloating, and cramping. The best proven diet is the FODMAP diet.
Toasted Potato Bread With Scrambled Eggs And Spinach
Whole-grain foods are a good source of fiber, which normally helps reduce constipation and supports overall health. The high levels of fiber in whole grains may be hard to digest during an ulcerative colitis flare.
Potato or sourdough bread is usually easier to tolerate for people with ulcerative colitis. Top with scrambled eggs for a good source of protein.
Add sautéed spinach for a healthy dose of iron.
You May Like: If You Have An Ulcer Where Does It Hurt
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
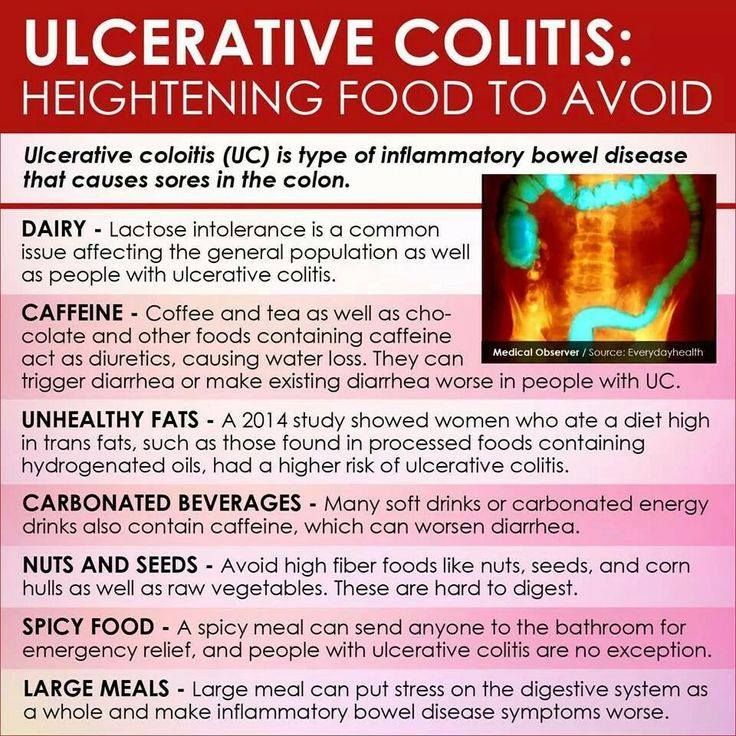
Foods Rich In Sulfur And Sulfites
Foods like beer, wine, shellfish, some dried fruits, white bread, and cured meats containsulfur, producing excess gas in the colon. Even without these foods, UC patients produce more hydrogen sulfide than usual, and they have difficulty breaking the gas down due to inflammation of the colonic wall. Hence, ingesting more foods with sulfur causes more damage to the colon.
Don’t Miss: Dog Skin Ulcer Home Treatment
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Add In Meal Replacement Shakes As Necessary
Many experts recommend meal replacement shakes or nutritional supplements, like Ensure Plus or Boost, to help with weight maintenance. Liquid supplements like these take up very little volume and are easy on the stomach, but they contain a relatively high amount of calories and protein.
I eat every two or three hours, even if its a couple of crackers, and drink a meal replacement shake. This helps me maintain my weight, said a member.
Note that these shakes often contain dairy products, so talk with your doctor for their recommendation, especially if you are sensitive to dairy or are lactose intolerant.
Don’t Miss: Stage 1 Pressure Ulcer Treatment
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
A Healthy Crohns Disease Diet
Not everyone with Crohns disease has the same food triggers, Taylor says, so you might need to do some sleuthing to figure out what works for you. Try keeping a food journal jotting down what you ate and any symptoms you notice to look for clues about the foods that make your stomach unhappy.
When you arent having symptoms, though, try to eat a balanced diet. You dont want to regularly shun healthy foods like whole grains, veggies or beans. Malnutrition can be a problem for people with Crohns disease, so only avoid these foods during a flare-up, she says.
Managing this lifelong disease can be a challenge, and a dietitian can help you manage your diet.
Crohns is different for every person, so work with someone who can help you design an individualized plan, Taylor says. If you have a dietitian in your corner, theyll be available so that when you have a problem, they can steer you in the right direction.
You May Like: Are Ulcerative Colitis And Ibs The Same
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
What Foods Should I Eat If I Have Ulcerative Colitis
Many people with ulcerative colitis can eat a normal diet, but during flare-ups your diet may need to be altered to help reduce your symptoms.
Eating during a flare up
When you are experiencing a flare-up, eating a temporary diet of low-residue or low-fibre foods may reduce the amount and frequency of the stools you pass and allow your colon to heal.
Foods to eat during a flare-up include:
- Low-fiber fruits: bananas, cantaloupe, honeydew melon. Cooked, pureed, canned or peeled fruits. Avoid skins and seeds.
- Lean protein sources: fish, lean cuts of pork, white meat such as chicken, soy, eggs, firm tofu and smooth nut butters
- Refined grains: sourdough, potato or gluten-free bread, white pasta, white rice and oatmeal
- Seedless, skinless vegetables: fully cooked, peeled vegetables such as asparagus tips, cucumbers, potatoes and squash
- Oral nutritional supplements or homemade protein shakes
Eating when in remission
When symptoms have lessened or subsided, many people with ulcerative colitis can resume a more normal, well-balanced diet and reintroduce foods slowly.
Slowly reintroduce:
You May Like: Can You Take Tylenol With A Stomach Ulcer
You May Like: Home Remedies For Stomach Ulcers During Pregnancy
Should Supplemental Vitamins Be Taken If So Which Ones
Again, that depends on the extent and location of the disease. As noted above, vitamin B-12 is absorbed in the lower ileum. That means that people who have ileitis or those who have undergone small bowel surgery may have a vitamin B-12 deficiency because they are unable to absorb enough of this vitamin from their diet or from oral supplements. To correct this deficiency , a monthly intramuscular injection of vitamin B-12 may be required. Folic acid deficiency is also quite common in patients who are on the drug sulfasalazine. They should take a folate tablet, 1 mg daily, as a supplement. For most people with chronic IBD, it is worthwhile to take a multivitamin preparation regularly. If you suffer from maldigestion or have undergone intestinal surgery, other vitamins-particularly vitamin D-may be required. Affecting as many as 68 percent of people, vitamin D deficiency is one of the most common nutritional deficiencies seen in association with Crohns disease. Vitamin D is essential for good bone formation and for the metabolism of calcium. Supplementation of this vitamin should be in the range of 800 I.U./day, especially in the non-sunny areas of the country, and particularly for those with active disease. Together with vitamins A, E, and K, vitamin D is a fat-soluble vitamin these tend to be less easily absorbed than water-soluble vitamins. Consequently, they may be absorbed better in liquid rather than pill form.
Should I Take Extra Vitamins And Minerals
Yes, you should take a complete multivitamin with minerals.
If you take steroids or limit your intake of dairy products, you should also take extra calcium and vitamin D .
If you are take sulfasalazine you may need to take folic acid.
Iron and vitamin B12 deficiencies are common with IBD, so you may need to have blood tests to measure these nutrients.
With prolonged diarrhea, you may also need magnesium, zinc and potassium supplements. An electrolyte drink, such as Drip Drop, may help add these nutrients back into your body.
Check with your doctor if you are concerned about your nutrition.
You May Like: What Can Cause Ulcers In The Intestines
Can Ulcerative Colitis Cause Me Constipation
Some individuals with Ulcerative Colitis experience constipation. No matter which symptoms you experience, learn how to prevent and treat your Ulcerative Colitis constipation before it affects your quality of life.
In general, Ulcerative Colitis causes inflammation in the large intestine and the rectum. When the inflammation associated with UC is concentrated in the rectum, you are likely to feel constipated. This happens because the inflammation in the rectum makes it difficult to pass stool out of your body. This form of Ulcerative Colitis is called proctitis. For individuals with proctitis, constipation may be accompanied by bleeding and a sense of urgency that are usually experienced with diarrhea. However, because the inflammation associated with proctitis is concentrated to the rectum the large intestine can successfully absorb water, which prevents diarrhea.
- Association / Trigger with other Gastrointestinal Symptoms: including gas and stomach pain, which may further complicate Ulcerative Colitis.
Read our full discussion of Ulcerative Colitis and constipation here.
Is Ulcerative Colitis A Genetic Condition
One of the most significant risk factors for Ulcerative Colitis is family history. Scientists believe that individuals inherit genes that put them at risk for Ulcerative Colitis. At some point in life, environmental factors trigger the immune systems to attack the large intestine and the disease sets in.
Researchers estimate that between 10 and 25 percent of people with Ulcerative Colitis have an immediate family member with IDB. It is also believed that if one parent of a child has IBD, the child has a two percent risk of also developing IBD at some point in life. If both parents have IBD the risk for the child increases. Ulcerative Colitis is also more prominent in individuals who have more distant relatives that suffer from Ulcerative Colitis. Research also indicates that in individuals with a family history of Ulcerative Colitis, the age of disease onset tends to be earlier.
More specifically, studies have been conducted on both identical and fraternal twins who have Ulcerative Colitis. If one twin has Ulcerative Colitis, their identical twin will also have Ulcerative Colitis about sixteen percent of the time, while their fraternal twin will have Ulcerative Colitis about four percent of the time.
Despite all these statistics, it is important to note that most individuals with Ulcerative Colitis do not have a family history of IBD.
Read our full discussion of Ulcerative Colitis and Genetics here.
Recommended Reading: Signs And Symptoms Of Ulcerative Colitis Flare Up
Ulcerative Colitis: Lets Talk
Colitis, Ulcerative Colitis, and Crohns are often used interchangeably but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohns Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohns disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Don’t Miss: What Are The Signs Of A Bleeding Stomach Ulcer
Will Ulcerative Colitis Affect My Stool
Changes in bowel movements are one of the key markers of Ulcerative Colitis. UC stool shape, color, and smell can be quite different than your average bowel movement. If you have Ulcerative Colitis, your immune system essentially attacks healthy cells in your digestive tract, which causes inflammation in your colon and rectum. Below are some key indicators that you may have Ulcerative Colitis based on your stool.
- Color: You might notice bright red, maroon or black color indicating the presence of blood. You may also notice more mucus in the stool than normal.
- Odor: The odor of the stool may be increasingly foul compared to the typical smell.
- Texture: Presence of UC typically causes loose, watery stools. In reference to the Bristol stool chart, UC stool texture will most likely resemble types 5 through 7.
- Frequency: Inflammation can cause increased motility and frequency of bowel movements. Many people experience frequent urgency and diarrhea.
- Effort: People with UC may experience burning or painful stools.
Always consult your primary care doctor. They can refer you to a local GI specialist if needed
If diagnosed, you may want to seek a specialist for your specific disease in your area
Maintain A Balanced Diet
Like many digestive disorders, what works for some may not work for others. It can be difficult to say exactly what should be avoided for each person. However, those in the know agree that if you are living with UC it is extremely important that you drink plenty of liquids and maintain a healthy, balanced diet.
You May Like: Signs Of Ulcerative Colitis In Child
Don’t Miss: Can You Get An Ulcer In Your Intestines
What Should I Eat And Drink
Eat a high-calorie, high-protein diet. Strive for a balanced diet with foods from all food groups .
The food you eat should be based on what you like and what your body can handle.
Lactose intolerance is common in people with Crohns disease, but some people do not have issues when eating dairy products.
Try eating smaller, more frequent meals and snacks
If it is painful to eat or you are losing weight, try supplements like Boost, Ensure, and Breakfast Essentials .
Your fluid needs are increased with chronic diarrhea and acute flares. Drink more fluids during flares .
When your disease is active, a low-fiber, low-fat diet may reduce symptoms.
Ulcerative Colitis: This Is Why You’re Here Right
- Why did you get Ulcerative Colitis? The short answer is that scientists still don’t know. Genetics are a major risk factor, but some people without a family history develop the condition
- Ulcerative Colitis is caused by an autoimmune response from your body
- Your symptoms may include:
- GI: loose and urgent bowel movements, bloody stool, abdominal pain and cramps, persistent diarrhea
- Non-GI: appetite loss, weight loss, nausea, low energy, anemia
- There are flares and periods of remission throughout disease course UC is different from other types of colitis because tiny ulcers form, causing long term inflammation
You May Like: Aloe Vera Good For Ulcerative Colitis