Foods For Ulcerative Colitis: What To Eat When You Feel Well
When youre symptom-free, it may not seem important to eat certain foods or omit others. However, weight loss, fatigue, and nutrient deficiencies are all common problems with ulcerative colitis, which makes following a healthy diet between flares critical.
Since some people with ulcerative colitis have a tough time eating fiber, fear of flares may keep them from eating nutritious fruits and vegetables, explains Tracie Dalessandro, MS, RD, CDN, a clinical dietitian in private practice in New York City and author of What to Eat With IBD: A Comprehensive Nutrition and Recipe Guide for Crohn’s Disease and Ulcerative Colitis.
However, thoroughly cooking and pureeing fruits and vegetables can make them easier to digest .
To combat fatigue and weight loss, Dalessandro recommends eating foods with the highest quality nutrients, such as high-quality proteins, fruits, and vegetables, and staying away from fried and highly processed foods that are low in nutrient quality and density.
People with ulcerative colitis may also benefit from taking supplements. Dalessandro gives the following advice:
- Get screened by a dietitian and then take suggested nutritional supplements
- Take a well-rounded multivitamin
- Take a probiotic or eat foods with natural probiotics, like certain types of yogurt, which can also help maintain a healthy balance of intestinal flora and improve digestion
Use A Registered Dietitian
A registered dietitian can help you plan meals that will provide the right amount of nutrients while allowing your gut to heal. They can help you set and obtain positive nutrition goals, determine if you need supplements, and maintain a weight that is healthy for you. All of these things will help keep your body functioning at it best.
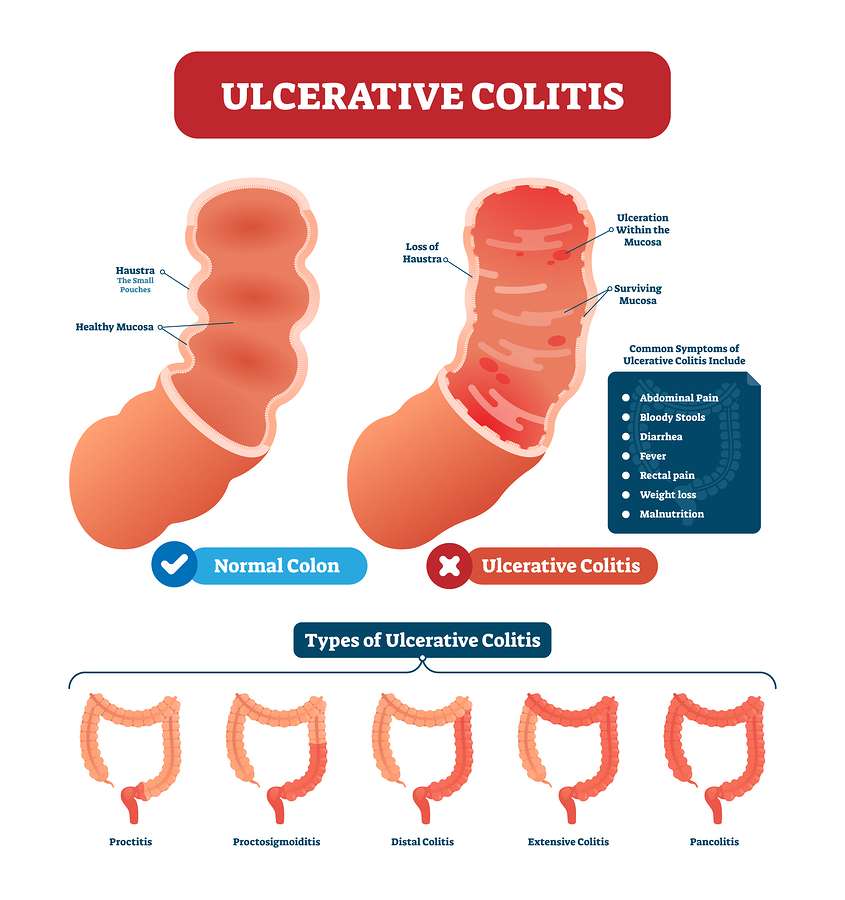
Ulcerative Colitis Symptoms And Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria .
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
You May Like: Specific Carbohydrate Diet Ulcerative Colitis
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Fermentable
- Monosaccharides
- Polyols
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
Common Trigger Foods To Avoid
Trigger foods can cause symptoms to manifest in ulcerative colitis patients. Most doctors recommend avoiding these items:
- Alcohol â Stimulates the intestine and triggers diarrhea.
- Caffeine â Another stimulant, caffeine speeds up the colonâs transit line and makes bowel movements more frequent. Itâs found in coffee, tea, and chocolate.
- Carbonated beverages â The carbonation can potentially irritate the digestive tract.
- Dairy products â As mentioned before, lactose-intolerance can manifest in UC patients.
- Dried peas, beans, legumes, fruits, and berries with pulp or seeds that are high in fiber can speed up the frequency of bowel movements.
- Foods with sulfur or sulfate â Gas production can be a problem for people with UC. Sulfate is found in beer, wine, some dairy products, eggs, stone fruits, bread, and cruciferous vegetables.
- Nuts and nut butter â These can make abdominal cramping worse, cause bloating, or cause diarrhea.
As with any diet or nutritional plan, maintaining a balance is vital. A clear discussion with a doctor about what a person with UC can and cannot eat is essential to ensure that they have the best nutritional intake to help them towards remission.
PicnicHealth is supporting new research into ulcerative colitis and Crohnâs disease. Learn more by visiting PicnicHealth.com.
Don’t Miss: Stomach Ulcer Foods To Eat
Focus On Healing Inflammation
The small intestine is where most of our nutrients from food are absorbed. Since the small intestine is involved with Crohnâs disease, this can be a significant hurdle to gaining and maintaining weight.
Even though ulcerative colitis is only in the large intestine, it does not mean that those with UC shouldnât focus on healing inflammation. Thatâs because inflammation can occur from gut permeability, bacterial and fungal overgrowths, food sensitivities, and more â not just from inflammation directly from having IBD. Additionally, inflammation in the large intestine presents its own concerns.
The more inflammation you have, the more your body will struggle to absorb nutrients. That hurts your chances of achieving an adequate weight.
I saw improvements in my weight when I made my diet simple but nutrient-dense. I left out some of the âfunâ gluten-free snacks I enjoyed and zeroed in on proteins, grass-fed butter and extra virgin olive oil, bone broth, teas, and herbs.
I even swapped out some of the products I used on my skin and in my home to eliminate them as a potential source of stress for my body.
To start healing inflammation, focus on eating an anti-inflammatory diet and incorporating the best foods for gut health.
In general, an anti-inflammatory diet is low in sugar and free of refined grains. The focus should be on whole foods like quality proteins, fats, fruits, vegetables, nuts and seeds as tolerated, and water as the main source of hydration.
How To Gain Weight Even If You Have Ibd
Some Crohnies and UCees need to gain weight. They may have had a flare or smoldering disease that never quite gets completely under control. The presence of inflammation increases the calorie needs, so Crohnies and Ucees need to take that into consideration when trying to gain weight.
Getting the ExtraCalories You Need
If you are trying to gain weight, you have to eat an extra 3500 calories to gain a pound. If you eat an extra slice of bread each day , you will generally gain a pound in 35 days. Add 2 tablespoons of peanut butter to the bread , and now it will only take you 12 days to gain a pound. What you are doing is making each bite count for moreby loading on the calories.
You can increase calories in many easy and healthy ways:
- Add cheese, seeds, and nuts to your salads
- Eat plenty of baked potatoes and load them with meat, cheese or whatever you’d like
- Add extra oils to your vegetables or potatoes when you cook
- Snack on handfuls of trail mix and dried fruit
- Don’t have a cracker without something on it
- Make a smoothie with Greek yogurt added
- Eat tropical fruits or add them to smoothies
- Drink a protein shake or nutritional shake in the evening
But remember to cut back once you’ve gained the weight you need. Your doctor and a dietitian can help. You’ll also want to discuss your difficulty gaining with your doctor, because it may mean that there is more that needs to be done to control your disease.
Read Also: How To Use Aloe Vera Gel For Ulcerative Colitis
More Information About Ulcerative Colitis
According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
The following diseases fall into the colitis/IBD category they all can be treated with a combination of medication and improvements to your eating habits:
Dont Leave Out Macros
Itâs important to evaluate what you are eating on a typical day and see how you can optimize the types and quantities of your food. Not eating enough macronutrients, including protein, carbohydrates, or fat, can be detrimental, especially if you are already underweight.
When youâre looking to gain weight, itâs not the right time to cut any macronutrients
Try to prioritize whole-food macronutrients. What I mean is, pick sweet potatoes over bread. Choose chicken, beef, and fish over protein powders. Opt for extra virgin olive oil, grass-fed butter , and coconut oil over vegetable oils. This provides nutrients that are much more easily usable and have health benefits.
Give yourself a mental checklist and make sure there is always protein, fat, and carbohydrates on your plate. You may want to work with a dietitian or nutritionist to make sure your portions are adequate for your goals.
You May Like: Hand Foot And Mouth Ulcers
Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Nutritional Requirements For Ibd: How To Plan A Diet For Ibd
-
Adequate Caloric Intake:
Meeting the bodys calorie demands is essential to prevent tissue wasting and weight loss caused by IBD. However, consuming adequate calories is challenging as loss of appetite is a symptom of IBD. Caloric needs may increase during times of stress. Including inflammation, fever and diarrhoea. If your weight begins to drop, try adding about 250 to 500 calories more per day.
-
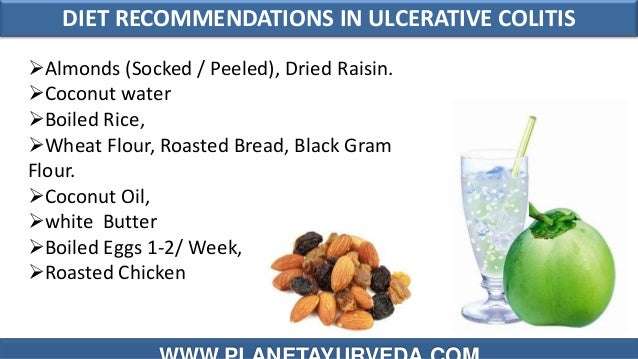
Select the Right Grains:
Consume wheat, broken wheat, rice, oats, barley and others grains. People with IBD should avoid whole grains or grains with husks as it may increase the IBD symptoms. Consume easy to digest grains during the flare stage. Rice, oats, quinoa are a good option.
-
Choose the Best Sources of Protein:
Animal proteins like fish, poultry, eggs, and dairy along with pulses and dals are recommended. During inflammation a high protein diet helps. Thoroughly cook the protein source and then consume to avoid any flatulence. Avoid bigger pulses like chana, rajma or whole urad, as it may induce flatulence. Using mung dal is better over using any other variety of dals.
-
High-fat Foods:
Due to fat malabsorption during IBD, avoid foods like butter, margarine and cream. It causes diarrhoea and flatulence. These symptoms are more visible in individuals with inflammation in the small intestine or removal of majority of small intestines. Include omega 3 rich olive oil, walnuts, fish or flax seed to reduce the inflammation caused by IBD.
Read- Health benefits of Flax seeds
Read Also: Do Enemas Help Ulcerative Colitis
The Difference Between Ulcerative Colitis And Other Digestive Diseases
Ulcerative colitis only affects the colon. Other types of Inflammatory Bowel Diseases include Crohns disease, which can affect the entire digestive tract, not just the colon. In addition, Crohns disease affects all layers and sections on the upper and lower intestines, while ulcerative colitis only includes the lining of the colon. Ulcerative colitis is not Irritable Bowel Syndrome , which is caused by abnormal muscle contractions in the GI tract that lead to symptoms that are similar.
The Best Foods To Eat And Avoid For Inflammatory Bowel Disease
Inflammatory bowel disease is a treatable, yet chronic and lifelong condition. IBD is a broad term that refers to the inflammation of the gastrointestinal tract and includes specific conditions such as ulcerative colitis and Crohns disease.
No plan has been proven to prevent or control IBD. But managing your diet can help manage your disease during flares and periods of remission. Be sure to talk to your physician or a registered dietitian about your nutrition needs and managing IBD.
Here are diet recommendations for managing IBD flares and remissions from UH Outpatient Nutrition Services.
Recommended Reading: What Foods Are Good For Ulcers And Gastritis
Uc And Lactose Intolerance
People with UC often think they have lactose intolerance, which means they can’t properly digest the sugar in milk and milk products, because some symptoms are similar. But UC doesnât make you more likely to have lactose intolerance. Your doctor can do a simple test to find out.
If you can, keep milk and dairy products in your diet. They are a very good source of calcium and vitamin D, which keep your bones healthy. Using steroids such as prednisone for a long time can thin your bones and make it harder for your body to absorb calcium, raising your chance of having osteoporosis.
If dairy products cause you discomfort, see if you can eat them in small amounts. Or try a lactase supplement to break down the lactose in dairy products.
If you just can’t stomach dairy products, your doctor may want you to take calcium and vitamin D supplements. Watch a video on how dairy affects ulcerative colitis.
Eat High Nutrient Foods
If you have IBD, you already know that processed convenience foods are not going to be the best choice for your diet. A better choice is foods that have a lot of nutrients in a smaller package. Foods that are considered nutrient-dense would be fruits and vegetables, beans, whole grains, dairy products, and nuts and seeds.
For those with IBD who find these specific foods problematic, other low-fiber choices include peanut butter, eggs, oatmeal, bananas, salmon, and tofu. The more “whole” your foods are, the more nutrient-dense your diet will be. Avoiding foods that come in bags or boxes is a good rule of thumb.
Recommended Reading: Ulcer Cause Blood In Stool
Make Your Own High Calorie Supplement
| Technique | |
|---|---|
|
|
|
Version 2 |
|
These are not complete meal replacements, but they are a quick and tasty source of calories and nutrients. You can substitute lactose free or items that contain soya . You can add whey protein powder to shakes to increase the protein. Experiment with a variety of different fruits, juices or syrups!
Top Tips for Increasing Calories in Your Diet
| Product | ||
|---|---|---|
|
||
|
Regular Mayonnaise |
|
|
|
Regular Sour Cream |
|
|
|
Iced Cream or Whipped Cream |
1/2 Cup ~ 145 kcal |
|
|
Dried Fruit, Nuts or Seeds |
1/4 Cup ~ 209 kcal |
|
|
Honey, Jam or Jelly |
|
|
|
Table Cream |
|
*kcal can vary by product, please look at label information for actual product information
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
You May Like: Crohn’s Disease And Mouth Ulcers
What You Should Do On A Regular Basis:
- Eat small, frequent meals.
- Consume a high calorie, high protein diet.
- Drink plenty of fluids, especially water.
- Eat a high fiber diet, including:
- 4 servings/day of whole grain breads and cereals
- 5 servings/day of fruits and vegetables