Risk Assessment And Prevention Of Pressure Ulcers
About this Guideline
Define early interventions for pressure ulcer prevention, and to manage Stage I pressure ulcers.
This best practice guideline assists nurses who work in diverse practice settings to identify adults who are at risk of pressure ulcers. This guideline focuses its recommendations on:
- Practice Recommendations including assessment, planning, intervention and discharge/transfer of care
- Educational Recommendations for supporting the skills required for nurses working with adults at risk for pressure ulcers
- Organization & Policy Recommendations addressing the importance of a supportive practice environment as an enabling factor for providing high quality nursing care, which includes ongoing evaluation of guideline implementation.
Revised: 2011
Nancy Parslow RN, CETN, MClSc Wound Healing – Team LeaderKaren Campbell RN, MScN, PhDChris Fraser HBSc, RDConnie Harris RN, ET, IIWCC, MScKathryn Kozell RN, BA, MScN, APN, CETNJanet Kuhnke RN, BA, BScN, MS, ET, PhDKimberly LeBlanc RN, BScN, MN, CETNSusan Mills Zorzes RN, BScN, MDE, CWOCN, CETNLinda Norton OTReg., MScCHLyndsay Orr PT, MCLSc Wound HealingFruan Tabamo RN, BPh, BTh, MCLScLaura Teague RN, MN, NP-AdultKevin Woo RN, PhD, GNC, FAPWCAFrederick Go, RN, MNBa Pham MSc, PhD – Advisory Panel Member
Fran MacLeod, RN, MScN – Team LeaderPatti Barton, RN, PHN, ETKaren Campbell, RN, MSN
Study Setting And Sample
The study was in Addis Ababa, the capital city of Ethiopia which contains 13 public referral hospitals . There are 34 private hospitals, 86 health centers and various NGOs and health institutions. The data in this study included nurses working from patient admission units in six randomly selected public referral hospitals . The units included were medical, surgical, orthopedics, intensive care unit, gynecology, pediatrics, dermatology, burn and oncology.
Nursing Diagnosis Impaired Skin Integrity Related To Pressure Ulcer
Ineffective peripheral Tissue Perfusion Pressure Ulcers occur when skin is in prolonged contact with an underlying bony prominence or other fixed objects. This can be due to improper positioning or activity restrictions. They are usually more severe than stage I and II pressure ulcers and can be dangerous if not treated properly. Pressure Ulcers are open wounds and should be cleaned regularly with mild soap, rinsed with clean water, and dried thoroughly.
Don’t Miss: What To Eat To Help Stomach Ulcers
Skin Integrity Nursing Care Plans
-Provide the patient with a scheduled play, pain management, and device change.
-Upon noticing the presence of redness or changes in skin temperature, notify the charge nurse immediately. This is to prevent further breakdown and eliminate serious complications such as infection.
-Adjust bed height or reposition the patient to prevent further pressure on the area.
-Assess precautions/contraindications: Review updated physician orders, laboratory and diagnostic studies, and current medication.
-Identify and eliminate/minimize the risk of exposure: Use standard precautions as appropriate for all patients, including transmission-based precautions when indicated.
Protect exposed areas from further damage: Use protective devices such as skin barriers or glove powder to reduce friction during patient repositioning and transfers.
-Instruct patient/family of home care to include:
Daily inspection for proper wound dressing and possible signs or symptoms of infection.
Change bandages as needed to maintain the integrity of the skin edges.
Keep wound area clean and dry. Use hydrogel dressings as ordered and according to the manufacturers recommendation.
Educate on the need to provide adequate nutrition and enough fluids for hydration to the patient.
We also have care plans for Cellulitis
Get the following premium features for free after ordering a custom nursing assignment from us:
- Formatting
Monitor the patients skin daily to ensure proper hygiene.
What Items Should Be In Our Bundle
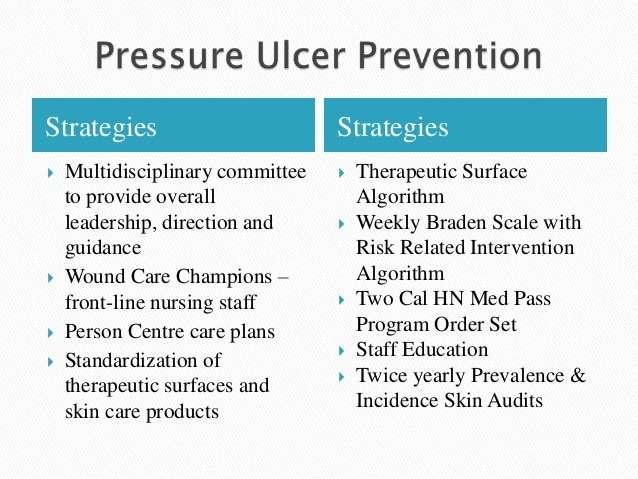
The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle. However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include. You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines .
Action Steps
Identify your bundle of best practices.
3.5.1 How do we customize the bundle for specific work units?
Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs. These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3.3.5.
Action Steps
- Identify the units that will require customization of the skin and risk assessment protocols.
- Modify the bundle, the assignment of roles, and the details of the unit to meet these special features.
Additional Information
You May Like: Ulcerative Colitis And Back Pain
Treatment For Decubitus Ulcer
Relevance To Clinical Practice
Nursing interventions should consist of evidence-based âbundlesâ and be adapted to patientsâ needs. To prevent pressure injuries among critically ill patients, nurses must be competent and highly educated and ensure fundamental strategies are routinely implemented to improve mobility and offload pressure.
Also Check: Side Effects Of Ulcerative Colitis
Pressure Ulcer Nursing Care Plans
A pressure ulcer is a localized skin injury where tissues are compressed between bony prominences and hard surfaces such as a mattress. They are caused by pressure in combination with friction, shearing forces, and moisture. The pressure compresses small blood vessels and leads to impaired tissue perfusion. The reduction of blood flow causes tissue hypoxia leading to cellular death.
Students Who Viewed This Also Studied
eduaction quality of life 214.pdf
St. John’s University
PHD212 Powders Calculation discussion .pdf
St. John’s University
Introduction to semi solid dosage forms C.pdf
St. John’s University
Dashboard and Health Care Benchmark Evaluation.docx
St. John’s University
St. John’s University HSA NURSING RE
eduaction quality of life 214.pdf
St. John’s University HSA NURSING RE
PHD212 Powders Calculation discussion .pdf
St. John’s University HSA NURSING RE
Introduction to semi solid dosage forms C.pdf
St. John’s University HSA NURSING RE
Dashboard and Health Care Benchmark Evaluation.docx
St. John’s University HSA NURSING RE
Case 1.docx
St. John’s University HSA NURSING RE
Dashboard Benchmark Evaluation.docx
Upload your study docs or become a
Course Hero member to access this document
Upload your study docs or become a
Course Hero member to access this document
You May Like: How To Get Remission In Ulcerative Colitis
All Ages: Care Planning
-
Develop and document an individualised care plan for neonates, infants, children, young people and adults who have been assessed as being at high risk of developing a pressure ulcer, taking into account:
-
the outcome of risk and skin assessment
-
the need for additional pressure relief at specific at-risk sites
-
their mobility and ability to reposition themselves
-
other comorbidities
-
patient preference.
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Temperature.
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
You May Like: Black Tarry Stools Ulcerative Colitis
Nursing Care For Older Patients With Pressure Ulcers: A Qualitative Study
Department of Geriatric Medicine, Odense University Hospital, Odense, Denmark
Department of Clinical Institute, University of Southern Denmark, Odense, Denmark
University College Absalon, Sorø, Denmark
Correspondence
Department of Geriatric Medicine, Odense University Hospital, Odense, Denmark
Department of Clinical Institute, University of Southern Denmark, Odense, Denmark
Department of Geriatric Medicine, Odense University Hospital, Odense, Denmark
Department of Clinical Institute, University of Southern Denmark, Odense, Denmark
University College Absalon, Sorø, Denmark
Correspondence
Department of Geriatric Medicine, Odense University Hospital, Odense, Denmark
Department of Clinical Institute, University of Southern Denmark, Odense, Denmark
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Read Also: How Do You Heal Leg Ulcers
Overall Theme: Prevention Of Pressure Ulcers Is Important In The Care Of Geriatric Patients
All the nurses interviewed stated that the topic of pressure ulcers was of essential importance in nursing care, in particular when caring for geriatric patients. It was expressed that skin care and observations hereof is considered as one of the fundamental nursing tasks in nursing geriatric patients.
During the interviews, four sub-themes emerged and all sub-themes were chosen according to how the nurses explained their experiences with perception and perception of pressure ulcers: Nursing resources on the ward, Basic nursing skillslift the duvet, Introduction of new nurses on the wardbedside teaching and Missing articulation of pressure ulcers.
Sample Size And Sampling Procedure
The sample size was determined using a formula of estimating a single population proportion for cross sectional study. Since the population size is less than 10, 000 , the final sample size was estimated using correction formula. The final sample size obtained including 10% non-response rate was 252. Then, the number of participants in each selected hospitals to obtain similar proportion of participants were determined using the population proportionate sampling . It is estimated using the formula: n=/N total, where, n=Proportion of nurses participate in the study in a given public hospital, nf=Final sample size obtained using correction formula , N=is the total number of nurses in the selected public hospitals .
Read Also: Hindgut Ulcers In Horses Treatment
Demographic Characteristics Of The Nurses
A total of 252 professional nurses were invited to participate in the study, 222 fully participated in the study, for a response rate of 78.7%. Among 369 nurses 128 were males. The mean ages of participants were 29 with minimum 20 and 61 years maximum. Most participants had a bachelors degree in , while 11% were enrolled in masters of Science degree in nursing. Nurses who are counted for their experiences in more than 10 years were 20.2% while majority of them 54% have 14 years of experience in nursing profession. Sixteen nurses reported that they had received and the largest proportion of them never received any training in PU prevention, while majority of them had not previously read research articles about PU compared to 31 who had read it. A limited number of nurses had attended PU training on conference. The majority of the participants were from medical ward as shown in Table .
Table 1 Frequency distribution of nurses socio-demographic variables
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
You May Like: How To Stop An Ulcerative Colitis Flare
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Additional Information
Tools
Practice Insights
What Is A Pressure Ulcer
A pressure ulcer is a break in the skin caused by unrelieved pressure. It can also be described as an area of tissue damaged or killed due to prolonged and intense contact with a hard surface, such as when someone lies down for too long without changing position.
- Prevent moist wound bed
- Provide oxygen to the pressure ulcer by keeping it exposed to air
- Treat underlying medical or surgical condition that caused the pressure ulcer
- Prevent excessive weight bearing on wounds
- Take good care of skin surrounding injured area
- Modify environment around the patient to prevent skin breakdown
Recommended Reading: What Does A Skin Ulcer Look Like
Pressure Ulcers In Palliative Care
The prevalence of pressure ulcers is higher in patients receiving palliative care than in the general population . There are estimated to be as many as 40 million people who require palliative care support worldwide . Palliative care is a concept associated with the end of life, and focuses on relieving symptoms and enhancing quality of life. The aim of palliative care may be to heal, improve symptoms or prevent deterioration. The need for palliative care has continued to rise in the UK due to the number of older adults with chronic conditions such as diabetes and heart disease .
Although wound healing may ultimately not be possible in patients who are terminally ill due to time restraints, suboptimal wound care and symptom management can cause unnecessary discomfort and have a devastating effect on the quality of a patients death . By managing pressure ulcer symptoms in patients receiving palliative care, improvement and even healing may be achieved .
Although patients may develop a pressure ulcer at the end of life, this does not mean that it should be accepted as a normal development . Patients with pressure ulcers may experience distressing symptoms such as pain that affect their appetite, prevent them from assuming a comfortable position and cause physical impairment .