Inflammatory Bowel Disease May Increase Ckd Risk
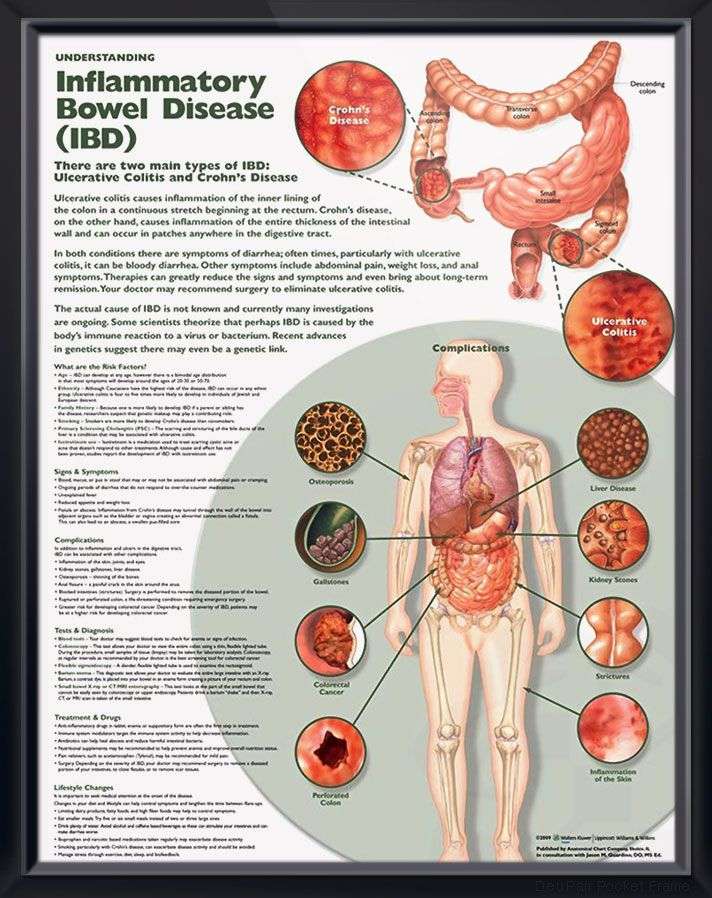
Inflammatory bowel diseases , such as ulcerative colitis and Crohns disease, or their treatments may increase the risk for chronic kidney disease , according to new research published in Clinical Gastroenterology and Hepatology.
Ravy K.Vajravelu, MD, MSCE, of the University of Pennsylvania in Philadelphia, andcolleagues conducted a retrospective study comparing 17,807 IBD patients fromthe United Kingdom with 63,466 matched control patients. Stage 3 or higher CKD,assessed by repeat measurements of estimated glomerular filtration rate ordiagnosis code, developed in 5.1% of IBD vs 3.5% of control patients, with age-standardizedincidence rates of 130.3 vs 91.3 per 100,000 person-years. The risk of CKD inpatients with IBD diminished with age, from a 7.9-fold increased risk of CKD byage 16 years to a 1.13-fold increased risk at age 77 years. The risk was onlyslightly lower for ulcerative colitis compared with patients who had Crohns disease.Active flare did not appear to influence eGFR.
Previous studies havelinked common non-biologic IBD therapies with impaired renal function. In thisstudy, neither 5-aminosalicylate nor methotrexate was associated with reducedeGFR. Azathioprine was associated with a slightly higher eGFR . Biologic medications, such as infliximab, adalimumab, andvedolizumab, are not usually prescribed by general practitioners in the UK, butthese medications have not been associated with CKD among IBD patients in priorstudies, according to the authors.
How Is Ulcerative Colitis Treated
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is. And it will depend on your intended family plans, such as getting pregnant.
There is no special diet for ulcerative colitis. But you may be able to manage mild symptoms by not eating foods that seem to upset your intestines.
Medical treatment may include:
- Medicines.Medicines that reduce redness and swelling in your colon may help to ease your belly cramps. More serious cases may need steroids, medicines that fight bacteria , or medicines that affect your immune system. Steroids aren’t a good choice for long-term treatment. Your healthcare provider will talk with you about medicines for long-term control. This may include pills, shots , or both. In addition, placing a medicine into the rectum can be very helpful in controlling your symptoms.
- Time in the hospital.This may be needed if you have severe symptoms. The goal will be to give you the nutrients you need, stop diarrhea, and replace lost blood, fluids, and electrolytes . You may need a special diet, IV feedings, medicines, or sometimes surgery.
- Surgery.Most people dont need surgery. But some people do need surgery to remove their colon. That might happen if you have heavy bleeding, are very weak after being ill for a long time, have a hole in your colon, or are at risk for cancer. You may also need surgery if other treatment fails. Or if the side effects of steroids and other medicines become harmful.
Kidney Disease And Ulcerative Colitis: Is There A Connection
Ulcerative colitis is one type of inflammatory bowel disease that affects the large intestine , causing inflammation and ulcers. Living with UC can be challenging and can increase your risk of developing other health conditions. When an individual has two or more conditions at the same time, its known as a comorbidity.
Comorbidities of IBD include kidney disease, cardiovascular disease, liver disease, cancer, arthritis, and migraine. Kidney diseases develop in 4 percent to 23 percent of people with IBD.
The most commonly reported kidney problems among people with UC are proteinuria , nephrotic syndrome, and end-stage renal disease . However, kidney problems are more prevalent in people living with Crohns disease.
One MyCrohnsAndColitisTeam member shared their experience with kidney issues. My kidney specialist moved me to stage 3 kidney disease, so I will fight on from here. Another member wrote, I also have kidney disease along with colitis.
| Engage with your doctor online and get answers to all your kidney-related IBD questions. |
This article will explain the connection between UC and kidney disease how its caused, risk factors, and ways to prevent or manage these conditions.
You May Like: Best Supplement For Gastric Ulcers In Horses
Does Drinking Water Help Uc
Its important to drink water when you have UC. Having enough fluids will replenish what you lose through diarrhea.
Water alone may not be enough. Your body also loses electrolytes like salt, potassium, and magnesium when you have diarrhea.
Drinking water plus electrolytes can help you stay hydrated. You can find that combination in the form of an oral rehydration solution at your local pharmacy. Sports drinks such as Gatorade and Powerade also contain electrolytes and fluid.
Pressure Or Pain In The Lower Back
In some cases, a stone may become stuck in the ureter. The ureter is the tube that carries urine from the kidney to the bladder. A blockage here causes urine to back up in the kidney, resulting in pressure and pain sensations in the lower back. These symptoms may occur on the left or right side, depending on which kidney is affected.
According to the University of Chicago, pain or pressure are usually the first signs of a kidney stone. In some cases, the symptoms may be very subtle and build up slowly. In other cases, they may come on suddenly, with no early warning signs. This pain can be severe and may lead to nausea or vomiting, or both. People often experience sharp, stabbing pain, and common measures such as rest or lying down do not relieve it.
Don’t Miss: Foods That Heal Ulcers And Gastritis
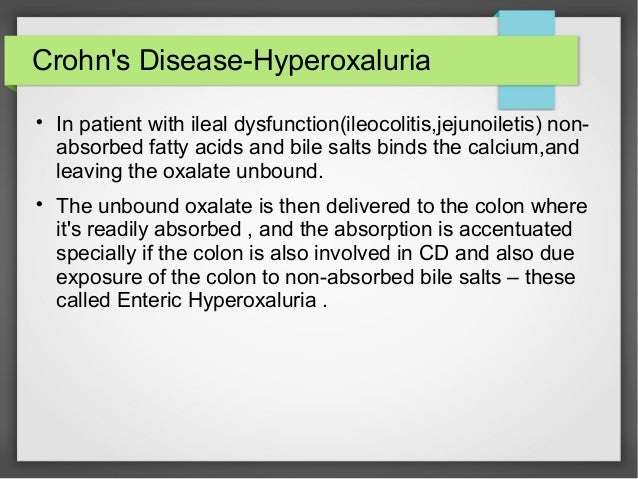
Other Complications Associated With Crohns Disease
Unfortunately, when you have Crohns Disease, whether mild or severe, this condition can impact your health in a variety of different ways aside from kidney stones.
This may include ulcers, inflammation throughout the digestive tract, malnutrition from lack of vitamin absorption, colon or colorectal cancer, bowel obstruction, and more. Its important to speak with your treating physician about any new or different symptoms that may pop up.
Occasionally, these issues may become so severe that surgery is required to remove or temporarily bypass diseased or obstructed parts of the bowel. This typically leads to a need for colostomy or ileostomy supplies.
At 180 Medical, we carry a wide variety of ostomy products and accessories to assist those who have been impacted by Crohns Disease to the point of needing ostomy surgery. Wed love the opportunity to help you find the right supplies for your individual needs. Contact us today!
Treatment By Disease Severity And Location
Mild-moderate distal colitis
- Oral aminosalicylates, topical mesalamine, or topical steroids
- Combination of oral and topical aminosalicylates is better than either alone
For refractory cases, oral steroids or IV infliximab can be used
Mild-moderate extensive colitis
- Oral sulfasalazine 4-6 g/day or alternative aminosalicylate 4.8 g/day
- Oral steroids for patients refractory to above therapy + topical therapy
- 6-MP or azathioprine for patients refractory to oral steroids, but not so severe as to require IV therapy
- Infliximab in patients who are steroid refractory/dependant on adequate doses of 6-MP/thiopurine or who are intolerant to these medications
Severe colitis
- Infliximab if urgent hospitalization is not needed
- If patient is toxic, should be admitted to the hospital for IV steroids
- Failure to improve in 3-5 days is indication for colectomy or IV cyclosporine
Indications for Surgery
- Absolute: Hemorrhage, perforation, documented or strongly suspected cancer
Also, surgery is recommended for severe colitis refractory to medical therapy
Read Also: How Do You Get Ulcers In Your Colon
Can Changing My Eating Habits Help Treat Ibd
Maybe. Researchers dont have enough evidence yet to show which specific diets, foods, or ingredients may make IBD symptoms worse or better. Some women say that changing the foods they eat helps relieve their symptoms during flare-ups. Most doctors recommend avoiding processed foods and foods with a lot of additives, such as carrageenan and maltodextrin .
Talk to your doctor about specific foods you may want to eat or avoid.21
Read Also: Natural Supplements For Ulcerative Colitis
How Does Blood In The Stools Appear
According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Dont Miss: What To Do When Ulcerative Colitis Flares
Don’t Miss: Over The Counter Ulcer Medication
Passing A Kidney Stone
Small kidney stones may pass on their own without treatment. A doctor may recommend drinking more fluids to help flush the stone out of the system.
In some cases, the doctor may prescribe the medication Tamsulosin. This drug relaxes the ureter, making it easier for stones to pass. Some people may also require over-the-counter or prescription pain relief medication.
According to the AUA, a person should wait no longer than 6 weeks to pass a small kidney stone. They should seek medical attention sooner if they experience worsening pain or an infection.
In some cases, a doctor may recommend surgery to place a ureteral stent to allow urine to bypass the stone, with or without removing the stone at the same time. According to the Urology Care Foundation, doctors usually reserve surgery for stones that may have caused or lead to infection or stones that do not pass and block urine flow from the kidney.
Urgent Care For Ulcerative Colitis
During a flare of ulcerative colitis, treatment is important to avoid complications. The most common complication is bleeding that can lead to anemia. With a severe flare, the colon may stop working and dilate . If not successfully treated, the colon may rupture and become a medical emergency. If treatment is not successful, surgery may be necessary. Usually, the entire colon is removed.
Recommended Reading: How To Test For Stomach Ulcers
Ibd Medications And Kidney Problems
The medications you take for IBD can sometimes cause issues with kidney function. Mesalamine and immunosuppressive medications like cyclosporine can sometimes change kidney function by causing the blood vessels in the kidneys to constrict, but this effect is very rare.
However, studies have found that other medications, such as aminosalicylates, methotrexate, and azathioprine, do not negatively affect estimated glomerular filtration rate , which is used to measure kidney function.
Also Check: How Long Does Pain Last After Kidney Stone Surgery
Colitis And Crohns Disease
Colitis and Crohns disease are Inflammatory Bowel Diseases where the intestines can become swollen, inflamed and ulcerated. The symptoms for these conditions include abdominal pain, loss of weight, diarrhoea, urgent need to go to the toilet, and tiredness. These symptoms will vary from person to person and can be more extreme for one person and not for another.
Diarrhoea caused by IBD is often accompanied by blood and mucus, especially with Ulcerative Colitis. The symptoms not only vary from person to person but may flare-up or improve/ go into remission unpredictably.
Treatments for IBD may include:
- Medicines. Most people with IBD take medicine to control their symptoms.
- Surgery. Surgery may be an option if medicine does not work to control your symptoms. Learn more about surgery for Crohns disease and surgery for ulcerative colitis.
- Steps you can take at home. Your doctor can talk to you about steps you can take at home to help control your symptoms and prevent flare-ups.
- Changes to your eating habits. Avoiding certain foods, changing other eating habits, and limiting or avoiding alcohol may help control your symptoms during flare-ups.
Some forms of psychotherapy, sometimes called talk therapy, may also help you cope with stress related to IBD symptoms and help make your pain less severe.14 Your doctor can refer you to a counselor or therapist, or you can find one at .
Recommended Reading: What Not To Eat During Ulcerative Colitis Flare Up
Medications For Ulcerative Colitis
The goal of medication is to control inflammation and heal the intestinal lining known as mucosal healing.
Medications used to treat ulcerative colitis include:
- Aminosalicylates, such as sulfasalazine and mesalamine , which reduce inflammation
- to treat bacterial infections
- Antidiarrheals to control diarrhea
- Biologic agents that can rapidly induce remission in patients with severe ulcerative colitis, defined as more than six bloody stool episodes daily
- Corticosteroids
- Immunomodulators that suppress the bodys immune response, such as azathioprine and 6-mercaptopurine
After beginning medication therapy, follow-up blood and stool tests for markers of disease activity, such as fecal calprotectin can help monitor the response to various therapies.
Data Collection And Study Endpoints
We collected data on patient demographics and on the medications used for IBD treatment, including 5-aminosalicylic acid , corticosteroids, immunomodulators , and anti-tumor necrosis factor -α agents . Medication use was defined as all relevant medications prescribed within 1 year of the diagnosis of IBD. We also collected information on comorbidities identified with ICD-10 codes, including hypertension , DM , dyslipidemia , congestive heart failure , ischemic heart disease , hyperuricemia, and gout . The definitions of these comorbidities were validated previously. The metabolically healthy condition was defined as the absence of DM, hypertension, and dyslipidemia. An underlying disease was defined as the presence of at least one of the following: DM, hypertension, dyslipidemia, congestive heart failure, ischemic heart disease, hyperuricemia, and gout.
Don’t Miss: Foam Dressing For Pressure Ulcer
Routine Screening To The Rescue
When the physician turned 60, he scheduled a colonoscopy, a recommended test to screen asymptomatic individuals over 50 for colon cancer. He had one at 50 it was completely normal. When it was time for his next exam, the doctor who did it the first time had retired, so he asked a friend, Dr. Erick Chan, a gastroenterologist, to perform the test.
He was still a little foggy from the anesthesia when Chan came by with what the physician assumed would be the usual report of normal results. He was wrong. I took some biopsies, and well wait to see what they show, Chan said. But I have to tell you, it didnt look normal. The test had been routine until Chan got close to the spot where the colon and the small intestine connect, a structure known as the ileocecal valve. Chan noticed that the valve looked a little asymmetric.
As Chan advanced his scope, he could see that the valve was distorted by scar tissue so much so that the connection was too narrow for his instrument to enter. Bringing his scope as close to the opening as he could, he saw that the tissue on the other side was an angry red and dotted with ulcers. They would have to wait for the biopsies to come back, but Chan suspected Crohns disease. Thats impossible, the man responded. He had no G.I. symptoms at all. No pain, no diarrhea, no blood in his stools. How could he possibly have Crohns?
You May Like: Diabetic Ulcer On Big Toe
Whats The Link Between Uc And As
Both UC and AS are inflammatory diseases. UC inflames the intestine, while AS inflames the spine.
A faulty immune response triggers inflammation in both diseases. Gene changes might be behind the immune misfire. People with IBD often have family members with AS. Scientists have found a few genes that might trigger both diseases, including HLA-B27. But just because you have the HLA gene doesnât mean youâll get AS.
Thereâs also a strong link between the gut and the joints. Scientists have found that bacteria and immune cells from the intestine can travel to the joints and cause inflammation there.
Donât Miss: Are Beets Good For Ulcerative Colitis
Read Also: Natural Ways To Heal Stomach Ulcers
Are There Any Special Dietary Requirements For Persons With Ulcerative Colitis
Although it seems plausible that a specialized diet might benefit patients with ulcerative colitis, there is actually no evidence to support treatment with dietary modification. Despite extensive research, no diet has been found to slow progression, treat, or cure the disease. It is recommended that patients stay on a balanced, healthy diet rich in fruits, vegetables, grains, lean meats, beans, fish, eggs, nuts. Patients should also try to limit foods with saturated fatshigh cholesterol. During flare-ups, patients should continue to eat as tolerated. The Crohns and Colitis Foundation of America recommends a bland diet with soft food during a flare including hot cereals, boiled eggs, mashed potatoes, steamed vegetables, canned or cooked vegetables to minimize discomfort.
S Boulajaad1* M Haida1 Ait Errami1 S Oubaha2 Z Samlani1 And K Krati1
*Corresponding author:Received: Accepted:Keywords
Abstract
The extradigestive manifestations of chronic inflammatory bowel disease most often affect the articulations, skin, eyes, liver and bile ducts. Renal involvement is rare, and manifests as kidney stones, glomerulonephritis, tubulointerstitial nephritis, and secondary amyloidosis. In this context of chronic inflammatory bowel disease, in particular ulcerative colitis, renal involvement is very often secondary to nephrotoxicity of the basic treatment of digestive pathology, and very rarely an authentic extradigestive manifestation of intestinal disease.
We report a case of IgA nephropathy as an extra-digestive manifestation of ulcerative colitis.
The objective of this study is not to neglect the IgA nephtopathy as an extradigestive manifestation of IBD which, even though rare, remains a condition to be looked for by clinicians during the follow-up of IBD.
Read Also: Support Surfaces For Pressure Ulcer Prevention
Recommended Reading: How Can I Ease The Pain Of A Stomach Ulcer