Types Of Compression Therapy
Compression therapy can speed up wound healing, as well as reduce swelling and pain. This type of therapy may be needed for months until the wound is fully healed. Ongoing use of compression therapy can also reduce the risk that an ulcer will come back.
Several types of compression therapy are available, including:
- Inelastic. This increases pressure on the wound while a person is walking or contracting the leg muscles, but not while at rest. The most common type of inelastic compression therapy is a moist bandage which hardens after drying. Because it is stiff, the dry bandage will not change when the size of the leg changes, which can be uncomfortable.
- Elastic. This type of compression therapy increases pressure on the wound both while moving and at rest. Both compression stockings and bandages can be used for this. Unlike inelastic compression therapy, this type can be removed at night, washed and easily replaced.
- Intermittent pneumatic compression. With this therapy, a pump is used inflate and deflate sleeves on the foot or leg. As the sleeve inflates, the pressure increases. Because the equipment is expensive and bulky, it is more commonly used for patients who are bedridden.
Recalcitrant Ulcers: Factors Prolonging Healing
Acute wounds physiologically heal within 4 weeks on the other hand, chronic wounds need a longer time to close, with an average healing time of 612 months for VLU. Moreover, it has been estimated that recurrence occurs in about 70% of VLU within 5 years of closure .
Several events occur to delay wound closure, including ulcer characteristics, concomitant diseases, patient characteristics, diagnostic delays and inaccuracies, therapeutic interventions, and environmental factors.
A well-known risk factor for recalcitrant ulcers is advanced patient age. In fact, elderly patients generally have reduced mobility as well as lesser compliance for compression bandages and garment treatments compared to younger patients. The VLU microenvironment is also characterized by a compromised cellular and biochemical machinery, where senescent fibroblasts fail to respond to proliferative stimuli .
Preexisting or underlying venous diseases, including all anatomic levels of venous system disease or deep venous thrombosis, are among the major risk factors for delayed healing.
Patients with higher body mass index and nutritional deficiencies also have a poor healing prognosis .
Additionally, a history of venous ligation or vein stripping, a history of hip or knee replacement surgery, ankle brachial pressure index < 0.8, and the presence of fibrin covering greater than 50% of the wound area have been associated with prolonged healing .
What Should I Do At My Appointment
Remember to remove any nail polish from your toenails before your appointment.
When you see the nurse or doctor, they should:
- Ask about your symptoms and how long you have had problems
- Examine your lower legs
- Do a simple test called a Doppler Ultrasound. This test compares blood flow in your ankle with that in your arm to find out if there are arterial blood flow problems in your lower leg. You may have to come back to have your Doppler test on another day or at another clinic.
- You may also be offered some other tests to check for other health problems that can affect your legs such as diabetes and anaemia.
You may hear different words to describe your wound such as ulcer, leg ulcer, sore, laceration, chronic wound and maybe others. Ask your nurse to explain their choice of word and what this may mean for you.
Don’t Miss: Is Soy Milk Good For Ulcerative Colitis
What Are Leg Ulcers
Leg ulcers are sores that develop on broken or injured skin. Usually, they are more prominent right above the ankles, on the inner side of your legs.
Other than skin injuries, leg ulcers may also develop as a result of an underlying medical condition. The diseases which may lead to the development of leg ulcers are discussed briefly below.
Hair Follicle Scalp Grafts

The hair follicle is a large reservoir of progenitor cells the hair bulge in a hair follicle has epithelial and melanocytic stem cells that can produce the interfollicular epidermis, hair follicle structures, and sebaceous glands and reconstitute in an artificial in vivo system to a new hair follicle. The isolated bulge epithelial stem cells can increase the hair density in patients with androgenetic alopecia. Gentile et al performed a placebo-controlled, randomized, evaluator-blinded, half-head group study that showed that hair regrowth with micrografts containing hair follicle mesenchymal stem cells may represent a safe and viable treatment alternative against hair loss.
Read Also: Best Antibiotic For Infected Leg Ulcer
Risk Factors For Leg Ulcers
- Age peripheral circulation becomes less efficient with old age.
- Varicose veins the one-way valves that stop blood from travelling backwards in the vein stop working. The pooling of blood stretches and distorts the vein.
- Cigarette smoking tobacco is known to constrict the vessels of the circulatory system.
- Arterial disease vein problems are more likely if the person already has other diseases of the arteries.
- Certain disorders these include diabetes and arthritis.
- Pressure sores bed-bound people are at risk of pressure sores, which are areas of damage to the skin caused by constant pressure or friction.
- Medication some cardiovascular medications can contribute to leg oedema and altered circulation.
Assessment Of The Patients And Wounds
Most CVLUs are not an isolated disorder but the manifestation of underlying conditions, such as hypertension, diabetes, and peripheral vascular conditions. History of comorbidities should be carefully consulted to make a confirmed diagnosis.
This 70-year-old female patient had suffered from chronic venous leg ulcers on both lower extremities for 40 years. Thirty years ago, a skin graft was harvested from her thigh without any anesthesia expecting for better survival of the graft. Unfortunately, the skin graft failed to grow, and she refused any skin harvest for skin graft. At this current time, her wound was prepared well enough for skin graft. A: Chronic venous leg ulcers on both lower extremities B: Prepared for skin graft.
The male patient had varicose vein and venous insufficiency for 15 years and ulcers for 1.5 years. A: Redness, warmth, pain, and edema with two ulcers were noticed on admission B: The inflation of the skin was relived after initial treatment C and D: X-ray showed calcification of the tissue around ulcers.
Ascending venogram shows the varicosities at lower leg and thigh, patency of femoral and iliac veins, and the degree of reflux while performing venography. A: Lower leg B and D: Thigh C: Femoral and iliac veins.
Read Also: How Do You Stop A Bleeding Ulcer
Signs And Symptoms Of Leg Ulcers
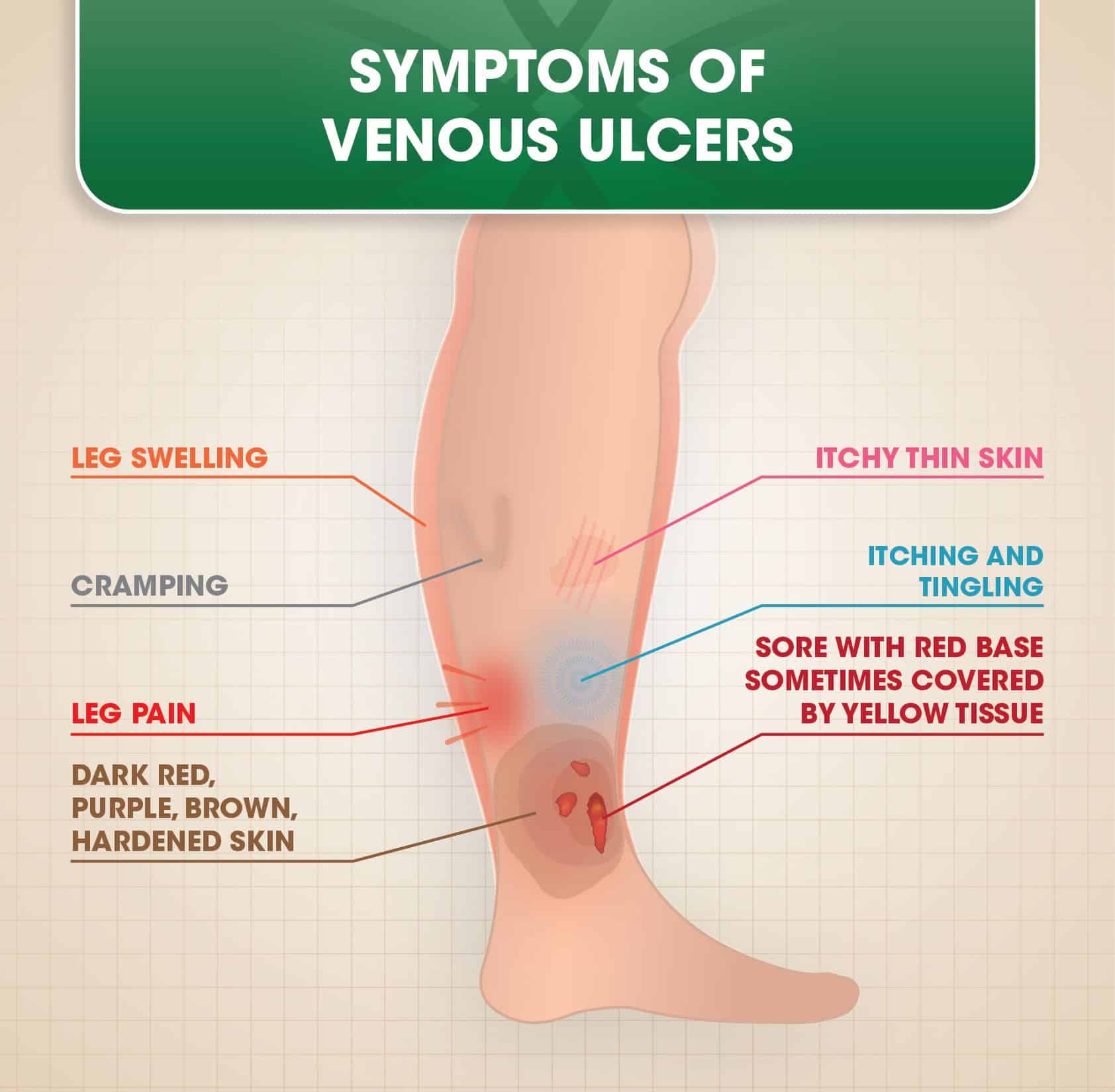
The most common symptoms that accompany leg ulcers are as follows:
- Swelling of the ankles
- Irritated or flaky skin
- Skin begins to harden and scale around the ulcers
These symptoms often vary in their severity. Although most leg ulcers usually disappear in a few days, some may be non-healing. It is always better to try and heal leg ulcers as soon as you can to prevent further complications. For that, you need to diagnose them first. The following are a few most common techniques used to diagnose leg ulcers.
Dont Miss: How To Heal Mouth Ulcers
What Types Of Wounds Can Alginate Dressings Heal
Alginate dressings usually do best on wounds that are actively giving out bodily secretions as the gel forms a shield around the sore to help soak up the secretions while keeping all other foreign bodies out of the cut, which lowers risks of infections. Alginate is also useful for wounds that are bleeding profusely as there are calcium fibers in the bandages which can break down and help slow the bleeding of a sore is bleeding heavily. Alginate dressings have long been used to dress wounds including fissures, hyper granulating tissue, interdigital maceration, heloma mole, and other lesions. Alginate dressings have also successfully been used to cover wounds on the parts of the body that are utilized the most such as on the feet. When it comes to healing venous ulcers, more studies are needed to see if Alginate dressings are effective.
If you do have venous ulcers or varicose veins, take a look at our Vein Score tool! After entering your symptoms and zip code, you will receive and vein score and a list of local vein physicians.
Medically reviewed by Dr. Susanne Woloson on 5-01-2020.
*Disclaimer: We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Medically reviewed by Dr. Susanne Woloson on May 5, 2020
Don’t Miss: What Will Help Stomach Ulcer Pain
What Are Venous Ulcers
As mentioned earlier, the most common and simplest definition of venous ulcers is that it is open sores that appear in your legs. Think of it as an open wound. Rather than heal and close like they normally do, they remain open and without the scab.
More Read
What Are Different Forms Of Green Kratom Available Online?
If your bodily function is working effectively, then it would simply be like a normal wound that closes eventually. However, since there are disruptions in your venous system and your legs are not pushing blood back to your heart, complications like ulcers start to arise.
It is also worth noting that venous ulcers are included in the CEAP classification used by doctors and specialists to determine the severity of a venous disease. Though the classification is not a static classification nor should be considered as disease progression, you should still keep in mind that out of the six classifications, two are for venous ulcers with one being the worst out of all the six. The two mentioned classifications are healed venous ulcers and active venous ulcers.
Active venous ulcer is the worst one out of the six because it is often accompanied by other symptoms aside from its unpleasant appearance. These symptoms can range from swollen ankles, discoloration or hyperpigmentation, leg pain, soreness, itchiness, tingling, and many more.
What Do Stasis Ulcers Look Like
Stasis ulcers are commonly located on the lower legs, usually just above the ankles. They are shallow, open wounds with uneven borders, and they can vary in size and shape. The base of the sore will be red, sometimes with an overlay of yellow tissue. The surrounding skin may discolor , and it may also be shiny, tight, swollen, and warm to the touch. Often, the whole leg will become swollen.
Recommended Reading: Can Ulcerative Colitis Cause Back Pain
You May Like: C Diff And Ulcerative Colitis Treatment
Risk Factors And Symptoms
The incidence of venous insufficiency rises with age, and is also linked to a family history of varicose veins, a sedentary lifestyle, or to jobs that require people to spend many hours on their feet. Venous insufficiency can also be caused by a partial blockage of the veins, for example by a blood clot .
The most common early symptom of venous insufficiency is chronically swollen ankles the feet and calves may also swell. The swelling can be accompanied by a dull aching, cramping, or feeling of heaviness in the legs and feet that becomes worse after prolonged standing.
As the condition progresses, people with venous insufficiency develop brown patches and deteriorating skin around the ankles. If venous insufficiency is not treated, venous ulcers may develop on the lower legs.
Doctors use an imaging test called a duplex ultrasound to determine if there is structural damage in the veins.
Read Also: Is Burping A Sign Of An Ulcer
How Are Leg Ulcers Treated
Treatment of leg ulcers typically involves compression bandages or stockings. Compression bandages or stocking provide pressure that may help restore the proper circulation of blood in your legs. Dressings, which are sterile bandages or wraps, may be placed on the sores to help aid in the healing process of leg ulcers. Your doctor may also prescribe antibiotics if your leg ulcer has become infected.
To help improve circulation in your legs, your doctor may also recommend that you raise your leg throughout the day for 30-minute intervals. Surgery may also be recommended as an alternative for restoring proper circulation in your legs.
Speak with your doctor to learn more about the available treatment options for leg ulcers.
Our heart and vein doctors at Heart Vein NYC have over 20 years of experience providing the New York City area with comprehensive, personalized vascular care for patients who suffer from leg ulcers or who have symptoms of a vascular condition. Contact our compassionate heart doctors if you believe you have a vascular problem and want to learn more about improving your vascular health. Call or schedule an appointment with Heart Vein NYC today.
You May Like: Air Mattress For Pressure Ulcer Prevention
Don’t Miss: What Foods Are Good To Eat With Ulcerative Colitis
Referral To A Specialist
In some cases, your GP or nurse may decide to refer you to a specialist in conditions affecting the blood vessels .
For example, you may be referred to a vascular specialist if your GP or nurse is unsure about your diagnosis, or if they suspect your ulcer may be caused by artery diseases, diabetes or rheumatoid arthritis.
After taking your medical history and examining you, the vascular specialist may need to arrange further investigations to plan your treatment.
Venous And Arterial Leg Ulcers
A leg ulcer occurs when skin breaks down, usually on the lower leg area, just above the ankle.
The majority of leg ulcers are caused by venous disease , others can be of arterial or mixed origin. If not treated correctly, a leg ulcer can become a chronic wound which requires longer healing time, and they have a tendency to reoccur.
You May Like: How Do You Get Mouth Ulcers
You May Like: What Is The Medication For Ulcerative Colitis
Dehydrated Human Amnion/chorion Membrane Allograft
An RCT compared dHACM allograft with multilayer compression only for CVLUs. Of 47 patients without complete healing during the initial study, wound size of 40% decreased in 20 patients < 40% ulcer area decreased in 24 patients. All 47 patients were treated with dHACM allograft for a mean of 46 d. Eighty percent patients in the 40% group had ulcer closure , and 33.3% patients in the < 40% group experienced ulcer closure at a mean of 103.6 d . Besides, dHACM allograft can be used as an adjunct to immunosuppressive therapy to reduce pain and heal the pyoderma gangrenosum ulcer in a patient with multiple comorbidities, including venous insufficiency and diabetes mellitus.
An RCT studied patients with nonhealing full-thickness CVLUs, and the ulcers treated weekly with dHACM allograft healed more significantly than those with standard wound care and compression . Another RCT study enrolled 84 participants, and venous leg ulcers treated with allograft for 4 wk had significant healing compared with multilayer compression therapy alone . A retrospective study showed that the average time to healing leg ulcers with dHACM grafts was less than that with conservative treatment . Another two retrospective cohort studies showed all wounds were closed effectively after the use of dHACM allograft.
Lead A Healthy Lifestyle
People who lead an unhealthy, sedentary lifestyle are far more likely to suffer from venous ulcers, as inactivity can impact circulation throughout your body, particularly your legs. As such, this can lead to blood pooling.
Also, weight gain is often associated with an unhealthy lifestyle, which puts more pressure on the veins in your legs. This can cause damage to the blood vessels, leading to issues like varicose veins and venous ulcers. By living a healthy lifestyle, you can prevent these issues from happening.
Also Check: Food For Ulcer Patient In Nigeria
What Causes A Stasis Ulcer
Stasis ulcers are a complication of venous insufficiency, which is a health condition that affects the veins. Healthy vein valves normally help blood return to the heart, but the vein valves in people with venous insufficiency are damaged or weakened. This can lead to blood pooling in the legs instead of flowing back toward the heart. The resulting fluid buildup beneath the skin can damage the skin layer, causing a stasis ulcer to develop.
Maintain A Healthy Weight
Having an elevated body mass index increases your likelihood of developing vein disease. Excess body weight strains tiny, one-way valves in your leg veins. Over time, this strain can cause veins to malfunction, leading to problems like varicose veins.
Weight loss and weight management are essential elements of venous ulcer prevention. Losing weight removes excess pressure on your veins, which can slow the progression of vein disease.
Recommended Reading: What To Take For Stomach Ulcers
Read Also: What Can Be Done For An Ulcer
What Causes Venous Ulcers
Your veins contain tiny valves that keep blood circulating throughout your body. These valves snap open and shut to move blood against the force of gravity back to your heart. In some people, venous diseases affect valve functioning. Other medical conditions, like diabetes, can also put you at risk for leg and foot ulcers.
The Role Of The Pharmacist In Educating Patients About Vsus
Since pharmacists are often perceived as one of the most accessible healthcare professionals, they have a critical role in the treatment and care of patients at risk of, or with, VSUs. This includes effective patient counseling and education, especially with regard to therapy for VSUs, proper use of medications used to treat VSUs, and reminders about preventive measures to decrease reoccurrence of VSUs. Since the incidence of VSUs is common in elderly and diabetic patient populations, pharmacists play a key role in identifying those patients at greater risk of developing VSUs. Pharmacists should also seize every possible opportunity to remind patients about the critical importance of adhering to therapy to enhance therapeutic outcomes and prevent further complications.
Pharmacists can also reinforce patient education with regard to the preventive measures for VSUs such as staying vigilant about oneâs overall health and adhering to the goals of therapy. Patients should be reminded of the importance of routine wound care and follow-up with their primary healthcare provider, monitoring the ulcer for signs of infection, and immediately seeking medical attention if the wound shows signs of worsening or not healing. Patients at risk for VSUs should be aware that with early diagnosis and implementation of and adherence to therapy, the condition can be effectively treated and healed to avoid complications.
Don’t Miss: Can I Live A Normal Life With Ulcerative Colitis