Are You At Risk For A Foot Ulcer
-
Do you have a foot deformity? If so, you may have a higher than average risk of a foot ulcer.
-
Do your shoes rub the wrong way? Poorly fitting shoes are a leading cause of foot ulcers.
-
Can you feel your feet? Diabetes can cause nerve damage to the feet, making it difficult to feel cuts or scratches.
-
Do you have high blood pressure? You may not realize it, but controlling your blood pressure could actually help protect your feet as well as your heart.
-
Have you had a foot ulcer before? If so, youre at higher risk of having another one. Check your feet daily and call your doctor at the first sign of an injury.
-
Do you go barefoot? Wearing shoes both inside and outside can help protect your feet from injury.
-
Can you see your feet? People who are overweight or have diabetic eye disease should ask a family member or caretaker to examine their feet every day.
-
Do you smoke? Ask your doctor for help quitting. Your feet will thank you.
How Should A Diabetic Foot Ulcer Be Treated
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing of the wound, the less chance for an infection.
There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Prevention of infection
- Taking the pressure off the area, called off-loading
- Removing dead skin and tissue, called debridement
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
Not all ulcers are infected however, if your podiatric physician diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
Preventing Infection
There are several important factors to keep an ulcer from becoming infected:
- Keep blood glucose levels under tight control
- Keep the ulcer clean and bandaged
- Cleanse the wound daily, using a wound dressing or bandage
- Do not walk barefoot
Off-Loading
For optimum healing, ulcers, especially those on the bottom of the foot, must be off-loaded. Patients may be asked to wear special footgear, or a brace, specialized castings, or use a wheelchair or crutches. These devices will reduce the pressure and irritation to the ulcer area and help to speed the healing process.
Applying Medication and Dressings
For a wound to heal there must be adequate circulation to the ulcerated area. Your podiatrist may order evaluation test such as noninvasive studies and or consult a vascular surgeon.
Managing Blood Glucose
When Is It Crucial To Seek Medical Attention
If patients observe flesh that has turned black around a region that is numb, it is important to seek medical attention. This can be a sign of infection in the foot ulcer. In the absence of treatment, foot ulcers can cause abscesses. The infection can also spread to other regions in the legs and feet.
Doctors assess the infection and decide if they need to perform surgery or amputation or need to use synthetic skin substitutes to replace the lost skin.
The risk for diabetics to experience an amputation is 10 to 20 times more than non-diabetics. Close to 85% of all lower-limb amputations are complications from a foot ulcer.
You May Like: What Does Ulcerative Colitis Affect
Structural Deformity And Limited Joint Mobility
Foot deformities, which are common in diabetic patients, lead to focal areas of high pressure. When an abnormal focus of pressure is coupled with lack of sensation, a foot ulcer can develop. Most diabetic foot ulcers form over areas of bony prominences , especially when bunions, calluses or hammer-toe formations lead to abnormally prominent bony points. Foot deformities are believed to be more common in diabetic patients due to atrophy of the intrinsic musculature responsible for stabilizing the toes.20
Rigid deformities or limited range of motion at the subtalar or metatarsophalangeal joints have also been associated with the development of diabetic foot ulcers.26,27 Other mechanisms of skin breakdown in the insensate diabetic foot include puncture wounds and thermal injuries from, for example, hot water soaks.
What Are Arterial Ulcers
A condition called peripheral arterial disease can reduce blood flow to your extremities. When this happens, your foot tissue may start to die. The ulcers that form from reduced blood flow are called arterial ulcers.
The word arterial means relating to arteries. Arteries are blood vessels that transport blood from your heart to the rest of your body, including your feet and toes. Anyone can get an arterial ulcer, but people who smoke or have diabetes, high blood pressure or high cholesterol are at higher risk.
Unlike neurotrophic ulcers, arterial ulcers can form on many parts of your body, including:
- On the tips of your toes.
- Between your toes .
- The bony parts of your feet and toes that rub against bed sheets, socks or shoes.
Arterial ulcers are:
- An unusual walk that puts too much pressure on one part of your foot or toe.
- Friction when your foot or toe rubs against the toe box of your shoe.
Although they dont cause ulcers, foot and toe ulcers are often found alongside toe conditions such as hammertoe, mallet toe and claw toe.
You May Like: How Often To Reposition To Prevent Pressure Ulcers
How Are Foot Ulcers Diagnosed
The appearance of a foot ulcer is usually enough for diagnosis. However, your doctor will need to examine the ulcer to determine its cause, which will determine the course of treatment. Be prepared to answer questions about your symptoms, your medical history, and your foot hygiene habits.
During the physical examination, your doctor will look for signs of infection, such as redness and warmth). Your doctor will also look at the size, depth, and location of the ulcer, and look for any foot abnormalities.
After testing the sensation in your feet, checking your reflexes, and using a tuning fork to see if you can feel the vibration in your toes, your doctor may be able to tell whether you have neuropathy.
Your doctor may also feel the pulse in your feet. Weakened pulse may indicate poor circulation, which may require further testing with Doppler ultrasound studies.
If the findings suggest an underlying condition, your doctor may refer you to a specialist for further evaluation. Tests that may be conducted may include any or all of the following:
- Wound culture of purulent drainage or material from the ulcer base
- Radiograph if a bone infection is suspected
- Computed tomography or magnetic resonance imaging scans to evaluate an abscess
- Doppler or arteriographic studies to assess blood flow to feet
- Complete blood cell count
- Blood glucose and glycohemoglobin tests, in patients with diabetes
- A bone scan or bone biopsy
What Are Neurotrophic Ulcers
Neurotrophic ulcers occur primarily in people with diabetes, although they can affect anyone who has impaired sensation in their feet. They can be found anywhere on your feet, but they usually develop on the parts of your feet and toes that are most sensitive to weight .
Neurotrophic ulcers dont cause pain. But they can be serious if they arent treated promptly or they dont respond to treatment.
A neurotrophic ulcer might be the following colors:
- Any combination of those colors.
The thin borders of the ulcers are punched out, meaning that theyre taller than the surrounding tissues.
Recommended Reading: Foods To Stay Away From With Ulcerative Colitis
Types Of Diabetic Ulcers
There are several types of diabetic foot ulcers
- Neuropathic ulcers occur where there is peripheral diabetic neuropathy, but no ischemia caused by peripheral artery disease.
- Ischemic ulcers occur where there is peripheral artery disease present without the involvement of diabetic peripheral neuropathy.
- Neuroischemic ulcers occur where the person has both peripheral neuropathy and ischemia resulting from peripheral artery disease.
Arriving at the correct diagnosis and identifying the cause of a diabetic ulcer is critical since it affects the treatment plan.
What Is The Progression Of Foot Ulcers
Certain health conditions, such as diabetes, prevent the body from healing normally and contribute to the development of ulcers.
Foot ulcers in disabled or elderly persons are often discovered by a caregiver after the ulcers have progressed, this is because of decreased sensation in their feet due to nerve damage or because of poor vision and limited flexibility, which prevents proper inspection of the feet.
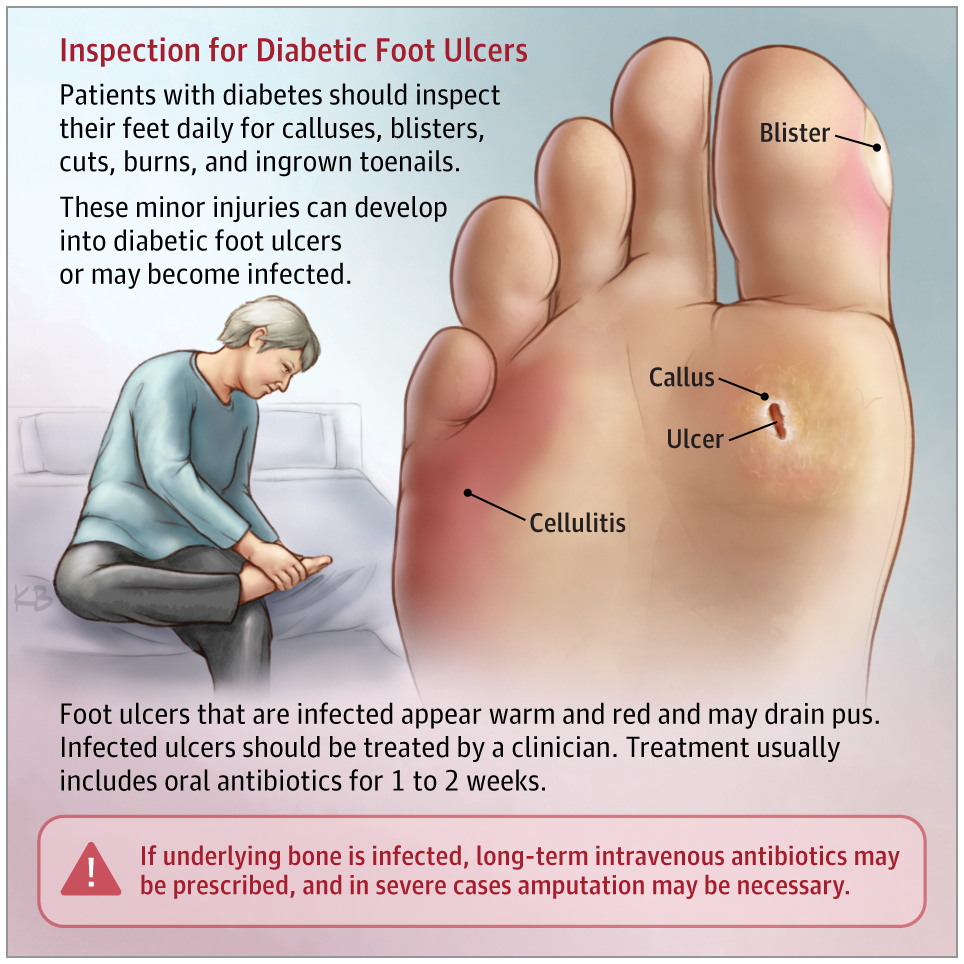
At first, a foot ulcer will involve only the skins surface and often looks like a shallow, red crater with a thickened, callused border.
As the ulcer progresses, it will involve all the layers of the skin. The crater will deepen, and the surrounding skin may begin to die and become infected.
Eventuallyafter weeks, months, or even yearsa foot ulcer may involve other structures, such as tendons and bones.
An infected ulcer can develop into:
- Cellulitis or an abscess
In the most severe foot infections, amputation of part or all of the foot or lower leg may be necessary.
Don’t Miss: Removable Cast Walker Diabetic Foot Ulcers
What Are The Risk Factors For Pressure Ulcers:
People with fragile skin are at additional risk, as are people whose nutrition is poor. Diabetes is also a significant risk factor for pressure sores on the feet.
One of the reasons pressure sores are so common among the disabled is that many such people have impaired sensation of pressure and touch due to spinal cord injuries. Because of this, they may not be alerted by pain or discomfort to the need to change position.
People who are bedridden for extended periods may lose a great deal of weight, which reduces the cushioning around their bones, making them more susceptible to pressure sores.
When To See A Doctor
If your sores are not responding to the over the counter drugs or home remedies, then it is your time to see your doctor. He/she may have more treatment options to offer but remember this will be determined by proper diagnosis. The bottom of the feet sores are cruel and painful sores that must be given great care and medication.
Recommended Reading: How Can You Get Ulcers In Your Stomach
Treatment Of The Foot Ulcer Depends On The Severity Of The Wound
|
Severity |
|
|
|
|
Not infected |
|
|
Mild infection |
|
|
Moderate infection |
|
|
Severe infection |
|
When To Call A Healthcare Provider

If the ulcer is large or deep, growing in size, incredibly painful, or if you have any signs of infection , you notice a bad smell coming from your ulcer, or youâre running a fever, call your healthcare provider right away.
Youâll also want to call your healthcare provider if your ulcer, no matter how minor, isnât showing signs healing after a week to 10 days.
In most cases, the ulcer will be dressed to protect the wound. However, if your ulcer is draining considerably, your healthcare provider may recommend leaving the wound uncovered. Dressing the ulcer if itâs draining considerably can impede healing.
If your ulcer is painful, pain medication can be prescribed. Antibiotics may also be prescribed either prophylactically to prevent infection or to treat an already infected wound.
Debridement is done to remove dead tissue from more serious ulcers. For deep ulcers or those that arenât healing after a long period of time, skin grafts may be needed. In the most severe cases, part of the foot, leg, or other appendage may have to be amputated.
Restoring good circulation is key in treating and preventing ulcers. This includes elevating the legs, wearing compression stockings, reducing pressure on ulcer-prone areas, superficial vein surgery. Leg ulcers, in particular, are incredibly likely to reoccur, so compression stockings are often needed to be worn for life.
Don’t Miss: Can Ulcerative Colitis Cause Blood In Stool
What Types Of Surgeries Can Help With Diabetic Ulcers
As podiatrists, we consider future foot function along with wound healing. If surgery is right for you, we will recommend a procedure that treats your pain or infection now so you can move more easily and with less pain.
Procedures we might discuss include:
- Debridement to remove dead or infected skin and tissue from the wound, which encourages healing.
- Skin grafts to reconstruct weakened or missing skin, which promotes healing and helps reduce the risk of infection. Skin can be taken from another part of the patients body, such as the thigh, or come from a donor it depends on each individual.
- Vascular surgery, which helps restore proper blood flow to the wound site, promoting healing and healthier skin.
- Shaving or removing bone to correct deformities that put pressure on the surrounding area, such as hammertoes, bone spurs, or bunions.
- Reconstruction of deformities such as flat or high-arched feet, which can cause areas of high pressure.
- Realigning or fusing joints to address biomechanical defects that increase pressure
- Lengthening tendons to release tension and take pressure off an ulcer, allowing it to heal, or prevent a new one from forming.
- Amputation of a toe or the foot if tissue is severely damaged or an infection will not stop spreading. Our limb salvage team exhausts all other options before recommending amputation.
Related reading:3D bunion surgery gets you back on your feet faster
Which Complications Of Pressure Ulcers Develop
The most serious complication that can occur as a result of a pressure ulcer on your foot or ankle is infection and sepsis. This occurs when bacteria enter the bloodstream through the compromised, ulcerated skin.
Infection then spreads throughout the body, endangering the patients life. Sepsis can also take the form of , a dangerous infection of the joints. If treatment is not administered, there is also the risk that gangrene could set in.
Even if sepsis does not occur, the patient is vulnerable to cellulitis infection of the skin, which can cause severe pain and swelling.
Read Also: What Foods To Eat When You Have A Stomach Ulcer
Nonsurgical Treatment For Diabetic Foot Ulcers
To help a diabetic foot ulcer heal, doctors at NYU Langone clean and disinfect the area. If the ulcer is infected, your doctor prescribes antibiotics to clear it up and prevent it from traveling to a bone in the foot.
Your doctor can refer you to an NYU Langone vascular specialist for additional medication if you have lower extremity arterial disease, a condition that impairs blood flow to the legs and feet and can cause an ulcer to heal more slowly.
NYU Langone doctors recommend regular wound care for foot ulcers, as well as other therapies.
Foot Ulcer Symptoms To Watch For
Initially, you may not be aware that you have a foot ulcer. You may have swelling, itching, or burning of the foot, or you may notice a rash, callus, redness, or brown discoloration of the skin.
A foot ulcer may not be painful in persons who have decreased nerve sensation in the lower leg, but this lack of pain can be misleading.
Foot ulcers most commonly occur on the side or bottom of the foot, which is another reason why an ulcer in this location can easily go unnoticed. They can also occur on a toe. Obvious signs of a foot ulcer are a foul odor and drainage of fluid.
You May Like: How To Calm Ulcer Attack
Prolonged Pressure On The Feet
As mentioned in the previous example, when shoes fit poorly, ulcers can occur. In people without nerve damage, this is usually due to severe atherosclerosis, or a deformity such as a fracture. Elderly patients often have difficulty or find it uncomfortable to examine their feet, ignoring moderate pain from pressure on the feet, which may result in the development of an ulcer.v
When Should I See My Healthcare Provider About Foot And Toe Ulcers
If you have diabetes, its important to see a podiatrist regularly. Whether you have diabetes or not, you should see a healthcare provider immediately if you find an ulcer on your foot or toe. Left untreated, it could get infected, leading to complications like amputations.
A note from Cleveland Clinic
It can be distressing to discover an open sore on your foot or toe. You might not know what caused it, it might not be healing and, if you have neuropathy from diabetes, you might not even feel it. Keep in mind that your healthcare provider can successfully treat your ulcer, especially if its found early. If left untreated, an ulcer can lead to serious complications.
If you have neuropathy caused by diabetes, remember that its important to check your feet and toes on a regular basis. Check your toes and feet every time you shower or when you go to put on your shoes. Contact your healthcare provider right away if you find an ulcer.
Recommended Reading: Venous Stasis Ulcer Right Lower Leg Icd 10
What Are The Symptoms Of Foot Ulcers
Most foot ulcers are located on the side or bottom of the footthe parts of the foot that carry weight when you are walking or standing or on the top or tip of a toe, where the toe can rub against shoes. Foot ulcers may also indicate poor circulation in the extremities, which in turn can be a symptom of diabetes.
These open sores can range from a shallow, red crater that only breaks the surface of the skin, to a deep crater that extends through the skin into the flesh below. In extreme cases, foot ulcers may even involve tendons, bones and other deep structures. The round crater can have a border of thickened, callused skin that develops over time.
Left untreated, foot ulcers can become infected and develop into:
-
An , a pocket in the flesh filled with
-
A spreading infection of the skin and underlying fat, known as
-
A bone infection, known as
- , an area of dead, darkened body tissue