Communication Has Never Been Easier
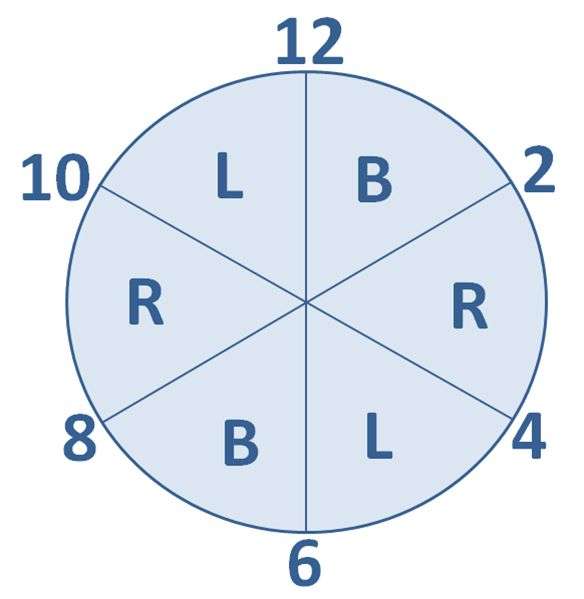
If you are searching for an economical, simple to use turning clock that can be set up in seconds choose the Safe Moves Turning Clock EZ! Using the 6 built in dial wheels choose between 2 hour or 4 hour turning routines based on the individual needs of the patient. Each dial wheel contains professional illustrations of Back, Right 30 Degree Side Lying or Left 30 Degree Side Lying clearly communicating to caregiver what position the patient should be in for the specified time period even if English is a second language!
The Safe Moves Turning Clock EZ integrates easily into care plans and makes it simple for supervisors to monitor staff compliance at a glance. Need an extra level of customization? The Safe Moves Turning Clock EZ can be written on with a dry erase pen to ensure the individual needs of your patient are communicated.
The Safe Moves Ez clock is re-useable and can be disinfected according to your infection control protocol.
Are Pressure Ulcers Preventable
Many clinicians believe all pressure ulcers are preventable, while admitting that some may be harder than others to prevent and require more aggressiveintervention. But the truth is some pressure ulcers may not be preventable. Why? Think back to basic anatomy and the organ systems: The skin is the largest organ of the body. If your patient is in multisystem organ failure with his kidneys, liver, and heart all failing, his skin is likely to fail, too.
Whether or not you view pressure ulcers as preventable, make sure to accurately document the patients condition and all interventions taken to prevent them.
Also Check: 8 Foods To Eat During An Ulcerative Colitis Flare
Why Heelift Boots Create A Cooler Drier Microclimate
There are a few features of Heelift® Brand Boots that help create the desired cooler, drier microclimate that prevents pressure ulcer development. As the above cut-away shows, HEELIFT® completely offloads the heel, allowing heat and moisture to escape so long as the patient is turned regularly. Additionally, the ventilation holes found in the HEELIFT® AFO, HEELIFT® Glide, and HEELIFT® Classic further help the flow of heat and moisture.
You May Like: How Do You Cure Ulcerative Colitis
You May Like: Fruits Good For Ulcerative Colitis
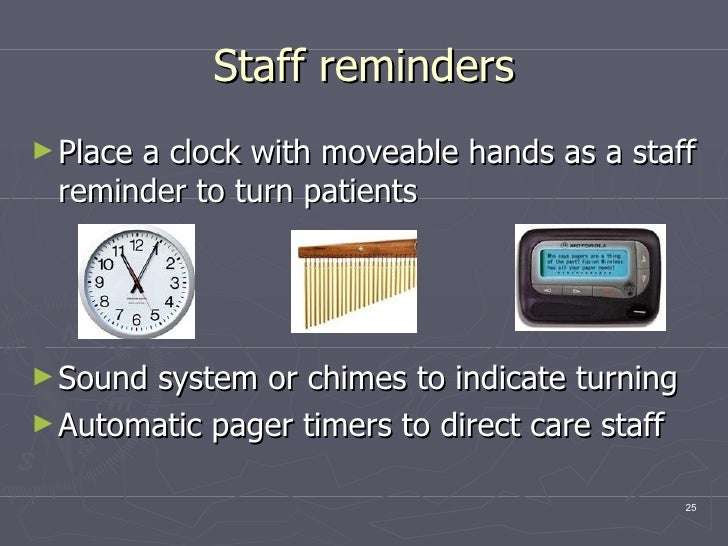
Turn Everyone And Move Study
The Turn Everyone And Move study13 was a 12-month paired facility 2-arm randomized intervention trial that tested the effectiveness of musical cues reminding LTC nursing and ancillary staff to help residents to move or reposition all residents, regardless of identified risk level, every 2 hours in 10 US LTC facilities. Staff and visiting family members received education on both PrU prevention and the intervention. Musical selections based on facility preferences were played over the facility public address system every 2 hours for the 12-hour daytime period. Intervention facility residents were 45% less likely than comparison facility residents to develop a new PrU. The researchers concluded that a broad approach involving customized musical cues that prompt multidisciplinary staff teams to encourage or enable all residents to move holds promise for reducing facility-acquired PrUs in LTC settings.13,26
Pressure Ulcer Prevention: A Turn And Positioning System Combined With Incontinence Care And Tailored/standard Repositioning
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : February 24, 2016Last Update Posted : March 9, 2018 |
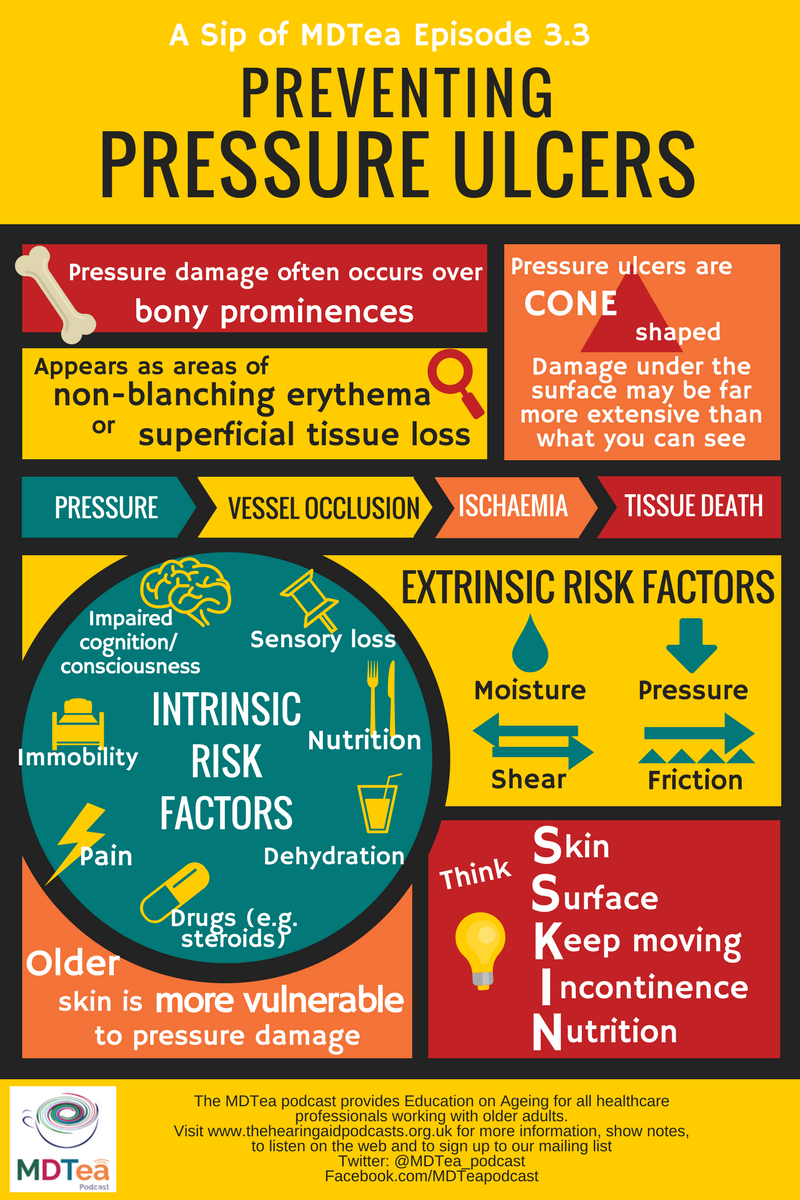
The prevalence of pressure ulcer in hospitals is 7,3% – 23%. The primary etiological factors are pressure or pressure combined with shear. Prevention is very important and comprises: preventive skin care including cleansing and protecting the skin from exposure to moisture, the systematic repositioning of the patient, the offloading of the heels from the surface of the bed, the use of adequate bed support surfaces and an adequate nutritional status. The development and implementation of a risk based prevention plan for individuals identified as being at risk is strongly recommended. Limited compliance exists towards pressure ulcer preventive interventions. 25,5% of the patients at risk receive fully adequate prevention in bed. The reposition frequence is adequate in 55% of patients at risk. There is a lack of rigorously performed research addressing the effectiveness of devices or risk based protocols to improve compliance. Health care budgets are limited, priorities should be set in the allocation of health care resources.
Read Also: Natural Cure For Peptic Ulcer
Reduce Friction And Shear
Friction is the rubbing of skin on an external surface, usually bed sheets. Friction to the most commonly affected areas can be reduced with protective devices. Heel and elbow cradles are typically made of egg-crate material and Velcro on.
Skin protecting dressings, such as films and thin hydrocolloid bandages can protect the skin from repeated friction but wont help reduce pressure.
The most important thing you can do to prevent injury from the friction is to make sure you dont create any yourself when youre repositioning your loved one. Use a draw sheet to help you lift your loved one off the bed when you lift and reposition.
Shear is created when the deeper fatty tissues and blood vessels are damaged by a combination of friction and gravity. The best way to avoid this type of injury is to avoid a semi-Fowler and upright position in bed. A semi-fowler position is where the head is raised less than 30 degrees and upright positions more than 30 degrees.
Now, you obviously cant avoid these positions all of the time. Many patients need to be semi-Fowler to help ease shortness of breath or prevent gastric reflux and all patients need to be in an upright position to eat safely.
To minimize the risk of shear injury in a semi-Fowler or upright position, take precautions to prevent your loved one from sliding down in bed. You can do this by raising the foot of the bed and propping the knees up with pillows.
Integrated Approach To Selection Of Cueing Innovations
We have integrated evidence-based cueing innovations from all 3 PrU prevention interventions into a unified framework for innovation selection and a logic model that can be used by LTC facility administrators, health care providers, and change agents to select the cueing innovations best aligned with their facilityâs core assumptions, resources, staff roles, and monitoring capacity for incorporation into a tailored intervention strategy for PrU reduction.
You May Like: Marshmallow Root For Ulcerative Colitis
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Read Also: Pepto Bismol And Ulcerative Colitis
Preventing Pressure Injury Through A Consistent Program
Of course in today’s health care, simply turning and repositioning a patient or resident at designated 2 hour intervals may help prevent pressure injuries, but it will not necessarily measure up for MDS coding, RUG scores, and payment purposes in long-term care, swing bed facilities, and hospitals. Also, during Federal and State surveys, pressure injury programs are investigated for ALL pressure injuries. With surveyors obtaining certification in wound care, we must enhance pressure injury prevention programs.
A turning and repositioning program must be consistent. The program must be documented, monitored, and evaluated, showing positioning and realigning of the body, and based on an assessment of the patient’s needs. The program should also be tailored to the patient’s time in or out of bed. Pay close attention to what your patient is doing all day long. Are they in the bed, sitting in a chair, or in a wheelchair? Pressure is pressure. That is the best perspective to have.
Also Check: What Foods Should You Eat If You Have An Ulcer
The Repose Foot/heel Protector
Repose foot protectors are designed specifically to minimise the risk of pressure damage to heels. They come in the form of splints made of Platilon, a polyurethane material with unique stretch, thermal and vapour-permeable properties. They are most effective when the patient is recumbent, semirecumbent or upright while on bed-rest, as the heels are supported above a void and therefore close to zero pressure, while the malleoli are protected by air-filled compartments.
The foot protectors are inflated using a hand-help pump. A valve ensures they are inflated to the correct pressure with no chance of over-inflation. This provides a pressure-reducing splint where the weight of the lower leg is redistributed over a wider area.
Turning Clock Ez Advantages
Economical solution for the prevention and treatment of pressure sores
Create customized turning and positioning schedules for at risk patients in seconds
Choose between 2 hour or 4 hour turning intervals
Visibly demonstrates best practice & due diligence to patients, families, caregivers, regulatory bodies & insurance companies
Easy beside reminder for care givers
Highly visible illustrations direct caregivers on proper positioning
Easy to use in multiple care settings hospitals, long term care, and community care
Supervisors can quickly and easily monitor compliance with wound care plans
Coated surface can be written on with dry erase marker
Easily wiped down for infection control protocols
Reusable
Don’t Miss: How Do I Know If I Have A Peptic Ulcer
Leverage Our Entire Pressure Injury Prevention Portfolio:
Learn more about our comprehensive solution the perfect fit for pressure injury prevention.
Helping you get CLOSER TO ZERO pressure injury incidence.2
Leaf Healthcare, Inc. was acquired by Smith+Nephew in 2019. About Smith+Nephew.
Use of this Web site is governed by the Terms of Use, Copyright and Disclaimer and Privacy Policy. This website is intended for health care professionals in the United States only. Not all products referred to may be approved for use or available in all markets. Please consult your local Smith & Nephew representative for further details on products available in your market. The information provided is for informational purposes only and is not intended to be medical advice. It does not replace the professional training, experience, and knowledge of the healthcare provider responsible for patient care, who must base treatment upon the unique characteristics of each patient. Every patients case is unique and each patient should follow his or her doctors specific instructions.
For detailed product information, including indications for use, containdications, effects, precautions and warnings, please consult each products Instructions for Use prior to use.
Endotracheal Tube Tie Repositioning
Plan/Do
Endotracheal tube ties were repositioned regularly to prevent device-related PI. We started with following the manufacturers guidelines. The package insert for the endotracheal tube securement device we use, the Hollister Anchor Fast, recommends that the endotracheal tube be repositioned every 2hours.19
Study/Act
After implementing this approach, device-related PI were reduced, especially stage 1 injuries.
Read Also: How To Know If You Have A Peptic Ulcer
The Implications Of Pressure Injuries
Its no secret that pressure injuries can become incredibly serious, from deep tissue damage all the way to sepsis, resulting in death. Developing pressure sores can lead to skin damage and infection, causing injuries that are, in many cases, preventable. They also place a significant legal strain on hospitals. According to the Agency for Healthcare Research and Quality, there are more than 17,000 lawsuits filed related to pressure ulcers a year, and the pressure ulcers themselves cost between $9.1 billion and $11.6 billion a year in fees.
With unnecessary patient suffering and legal issues both at stake, its important to create a culture of urgency within hospitals to reduce pressure sore cases among patients. By becoming quickly aware of the issues and monitoring skin from the beginning, this is much easier to do.
Pressure Injury Prevention Devices
The following devices are used to help offload pressure or reduce sheer to help reduce the incidence of pressure injuries/ulcers.
Offloading footwear This type of footwear consists of therapeutic shoes designed to provide pressure redistribution.3Protectors Protectors are devices that help reduce injury to the skin caused by friction or shear forces. The most commonly used locations are the elbows and heels.Positioners Positioners offload by suspending, elevating, or changing position of the body area.
Read Also: I Think I Have Ulcerative Colitis
Myths About Turning And Repositioning
Beware of the half truth. You may have gotten hold of the wrong half
We dont call them Pressure Injuries for nothing. Complex as they can be in both etiology and treatment, one element is common to all of them: Pressure. Turning and Repositioning is the linchpin to any and all effective pressure injury prevention programs. But as important as it is, there are many common misconceptions about Turning and Repositioning that have become entrenched in healthcare. These misconceptions encumber our ability to sustain effective prevention policies and programs for pressure injury prevention. A more clear understanding of this critical intervention can have a profound influence to the success of any facilities pressure injury prevention efforts.
As a wound care and bedside nurse, I have studied Turning and Repositioning of the bedbound patient exhaustively. From patients body mechanics to the nursing process to equipment design and usage, I have come to understand that there are many aspects of Turning and Repositioning that are often overlooked or misunderstood.The reader might identify and agree with my assessments, or maybe feel a little provoked to dispute my assertions. Either way, I hope this commentary will challenge all who share similar aspirations to stop pressure injuries to pause, reflect and step out of the proverbial preconceived notions box to think about how we may better approach this most important nursing intervention:
Myth #4. Turning is easy
REFERENCES
Pep Prevention Emergency Project Preventive Measures For Pressure Ulcers
PEP was a patient care innovation project, which has developed a new process to effectively prevent pressure ulcers among patients in the risk zone. When initiatives are already implemented in the emergency room the entire hospital is affected since patients are often admitted from there to the various hospital wards. This also applies to other care services, such as assisted living facilities. The process is now implemented atthe hospital.
The emergency department at Karolinska University Hospital, Huddinge, run the project in collaboration with Mölnlycke. The process involves most services at the hospital, as well as five ambulance companies.
Project manager: Jenny Delin.
Also Check: Ulcerative Proctitis Vs Ulcerative Colitis
Also Check: Difference Between Ulcerative Colitis And Hemorrhoids
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Strengths And Lessons Learnt
There are several strengths to this programme:
- Evidence-based healthcare practices were implemented.
- Results have been demonstrably sustained.
- Nurses were educated or had their knowledge refreshed in a multimodal way, using one-on-one interaction, small groups and online seminars.
- The entire approach involved the whole multidisciplinary team.
- Data were made highly visible by displaying it on each units quality board.
- Successes and challenges were presented at leadership meetings keeping the profile of the work high.
There were several lessons learnt during the course of this initiative. The first lesson we learnt is how vital it is to involve key stakeholders and a multidisciplinary team right from the start. Initially, this can be difficult but a good start leads to a successful and sustainable outcome. Second, we learnt that frontline staff should be aware of their own units data. Unless they are provided with their data, it is really impossible to create any sense of urgency. We provided real-time data to them and they were able to make striking improvement.
Involving our Respiratory Therapy department for medical device-related PI proved a success and we were subsequently able to involve them in other initiatives as well. This initiative has resulted in substantial team building.
Don’t Miss: Can Foot Ulcers Be Cured
The Case For Prevention
Pressure ulcer prevention entails two major steps: identifying patients at risk and reliably implementing prevention strategies for all patients identified as at risk. Prevention strategies include six key elements : conduct a pressure ulcer admission assessment for all patients, reassess risk for all patients daily, inspect skin daily, manage moisture, optimize nutrition and hydration, and minimize pressure. Facilities may wish to form a multidisciplinary team to develop a pressure ulcer prevention program.
Prevention Of Heel Pressure Ulcers In An Orthopaedic Unit
18 June, 2002
VOL: 98, ISSUE: 25, PAGE NO: 53
Anne Wilson, RGN, BSc, is tissue viability nurse, Royal Alexandra Hospital, Paisley
The development of hospital-acquired pressure ulcers on the heel is a well-acknowledged problem . In fact, after the sacrum the heels are the second most common anatomical site for the development of ulcers , and their incidence has increased steadily over the past few decades .
Although tissue breakdown is a complex multifactorial process, the focus with pressure ulcer development in the heels is on extrinsic factors such as pressure, shear and friction, with the most plausible explanation being the failure to relieve pressure. While many advances, such as pressure-relieving mattresses and beds, have greatly reduced the incidence of sacral ulcers . Krasner recognised that, even with pressure reduction, most support surfaces do not adequately relieve heel pressure.
Pressure ulcers may form when heel pressure on the mattress exceeds the capillary closing pressure and the heel position is not changed frequently enough . The heel is at increased risk of ulceration as it has a relatively low resting blood perfusion level if subjected to lower pressures than 32mmHg .
Cheney suggests this problem is compounded by orthopaedic surgical procedures requiring long periods in the operating room and in recuperation. To prevent the development of heel ulcers, therefore, predisposing factors must be identified, minimised and/or relieved .
Don’t Miss: Symptoms Of Having Ulcers In Your Stomach