Risks Of Pressure Sores In Hospital
A pressure sore is a painful wound that affects the skin and the flesh under it. If you sit in a chair or lie in a bed a lot, over time, the weight on the bony parts of your body stops blood from flowing.
Pressure sores can particularly occur over bony areas such as:
- hips
- tailbone
- heels.
Pressure sores can begin to form in as short a time as two hours and can be serious, potentially leading to infection that spreads to the bloodstream, if untreated.
Pressure sores are more likely to develop in people who are undernourished or who leak urine or faeces involuntarily . Being undernourished makes the skin thin, dry, rigid, and more likely to tear or break. Being incontinent exposes the skin to moisture from urine and faeces, which can lead to irritation and pressure sores.
Where It Starts: The Hospital Bed
When preventing pressure sores in hospitals, hospital beds themselves are determining factors. This is where XSENSORs ForeSite Intelligent Surface system comes in.
The system works using either a mattress overlay or an integrated mattress for hospital beds, embedded with thousands of sensor cells that continuously monitor patient body surface pressures. A bedside monitor displays real-time pressure images and clearly identifies parts of the body under sustained elevated pressure. A turn clock tracks the time between patient repositioning, and alerts staff to adjust their rotation.
This, ultimately, leads to every medical professionals goal: quality patient care and positive patient outcomes. With the support of XSENSORs technology, medical staff can focus on patient care where it is most needed, putting their energy into essential clinical activities, and not into preventative efforts that are unnecessary such as waking sleeping patients to rotate them, if they arent truly at risk of developing pressure sores.
Through providing caregivers with consistent information, XSENSORs ForeSite IS increases the integrity in continuity of care, helps avoid pressure ulcers from forming and may improve healing time for existing wounds to also reduce the length of hospital stays due to pressure ulcers.
The system comes with:
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
You May Like: What Does Asacol Do For Ulcerative Colitis
Treating And Reducing The Risk Of Pressure Ulcers After Leaving Hospital
Our skin is the most important barrier against infection so we need to look after it carefully. Sometimes, for a variety of reasons, people who are unwell develop pressure ulcers. At Great Ormond Street Hospital , we recognise that children can develop pressure ulcers too. This information sheet explains about the steps you can continue to take at home to reduce the risk of your child developing a pressure ulcer. It also explains how to manage a pre-existing pressure ulcer at home.Pressure ulcers happen when there is constant pressure on an area of skin because a person is not able to move or change position. Some medical devices can cause pressure ulcers, for instance CPAP masks, nasogastric tubes or splints. Pressure ulcers can also form when there is friction against the skin, for instance, rubbing on a bed sheet. Moisture can also make it more likely for a sore area to start. Areas that can be affected in children include: the back of the head, ears, heels, elbows, base of the spine and the nappy area.
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Don’t Miss: Blood Clots In Stool With Ulcerative Colitis
Examples Of Good Practice
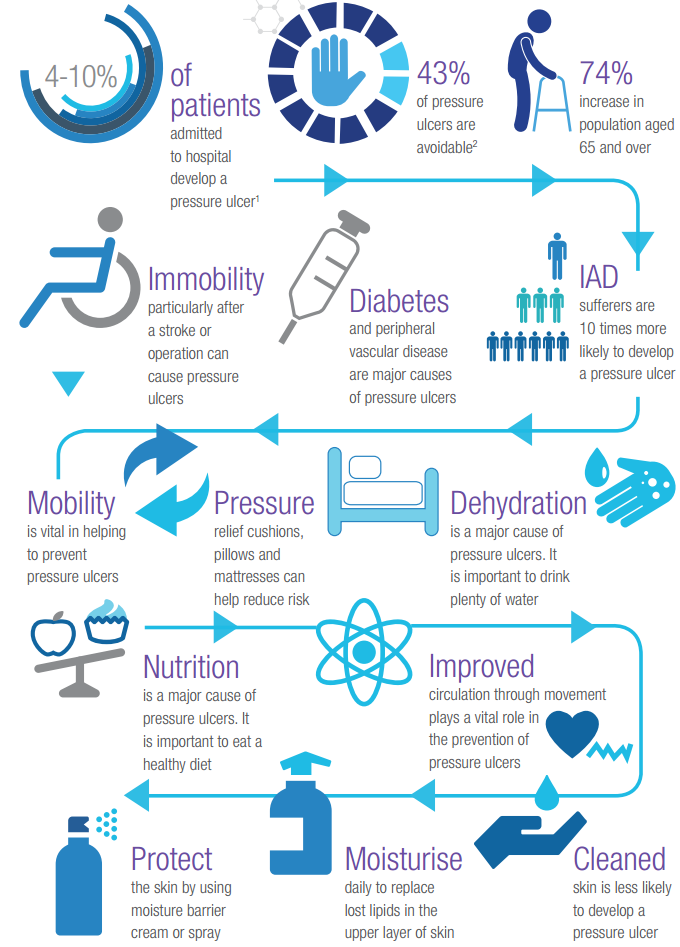
SSkin offers 5 simple steps to prevent and treat pressure ulcers.
Stop the Pressure provides details of many pressure reduction and pressure prevention initiatives across England.
PUinfo App by Buckinghamshire New University provides information to prevent pressure ulcers for people at risk and their carers.
The Eatwell Guide shows the proportions in which different types of foods are needed to have a well-balanced and healthy diet.
React to Red has been developed by the University Hospitals Coventry and Warwickshire NHS Trust, encouraging patients, carers and families to react to red skin over bony areas and ask for help and advice from a healthcare professional.
How Can Friends And Family Help
Caregivers might sometimes provide too much help. For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat.
If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals. This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly. This also includes regularly changing diapers or incontinence pads.
You should tell the nurses or doctors immediately about any red or sore areas of skin. They can then take a closer look at the affected area. It is always important to take pressure off that part of your body.
Don’t Miss: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
Preventing Pressure Ulcers In Operating Rooms
Preventing Pressure Ulcers also known as decubitus ulcers and bed sores is one of the most common complications of extended bed rest in surgery centres, hospitals and long-term care facilities. They occur when continuous pressure reduces blood flow to a part of the body, leading to a breakdown of the skin in that area. Rubbing and irritation from moisture can make the problem worse.
In Canada, research estimates that pressure ulcers are present in 26% of healthcare settings. That number is highest in non-acute and long-term care facilities and lower in community care centres. Though generally not recognized as a widespread problem, lack of resources and awareness among caregivers have been cited as barriers to reducing the prevalence of pressure ulcers.
Symptoms and Severity
Pressure ulcers occur in areas of the body that rub against bedding or mobility devices such as wheelchairs. This can include the hips, buttocks, elbows, ankles, back, legs and other areas. Pressure ulcers can be identified by a characteristic redness in the early stages and, later, by the presence of blistering and open sores. The severity of a pressure ulcer is measured on a four-stage scale:
Depending on the severity of the issue, treatment of a pressure ulcer can involve simply cleaning and treating the wound, followed by a course of antibiotics to prevent infection. In extreme cases, surgical debridement or even amputation of the affected areas may be required.
Who Is Vulnerable?
Questions To Drive Equipment Availability And Reduce Time To Therapy
If youre considering renting specialty equipment, remember to vet your rental provider to ensure youre getting high-quality, patient ready equipment. In the process, there are a few things to consider.:
If youre still in the evaluation process, here are some more questions you should ask third-party rental providers during your assessments.
You can also visit our Resource Center to learn more.
Recommended Reading: How Do They Check For Ulcers
Implementing A Prevention Plan
Preventing pressure ulcers can be nursing intensive. The challenge is more difficult when there is nursing staff turnover and shortages. Studies have suggested that pressure ulcer development can be directly affected by the number of registered nurses and time spent at the bedside., In contrast, however, one recent study suggested that there was no correlation between increasing the nurse-to-patient ratio and the overall incidence of pressure ulcers. Donaldson and colleagues noted that this particular study was limited by the fact that the researchers could not affirm compliance with ratios per shift and per unit at all times. Given that the cost of treatment has been estimated as 2.5 times that of prevention, implementing a pressure ulcer prevention program remains essential.
A key component of research studies that have reported reduction of pressure ulcers is how to sustain the momentum over time, especially when the facility champion leaves the institution. It is clear from the evidence that maintaining a culture of pressure ulcer prevention in a care setting is an important challenge, one that requires the support of administration and the attention of clinicians.
Key Aspects Of Pressure Ulcer Prevention
Standard practices aimed at preventing pressure ulcers include:
- Risk assessment to identify at risk patients in combination with a skin assessment)
- Skin and tissue assessment to look for signs of early pressure damage
- Preventive skin care to promote skin integrity and protect the skin from damage
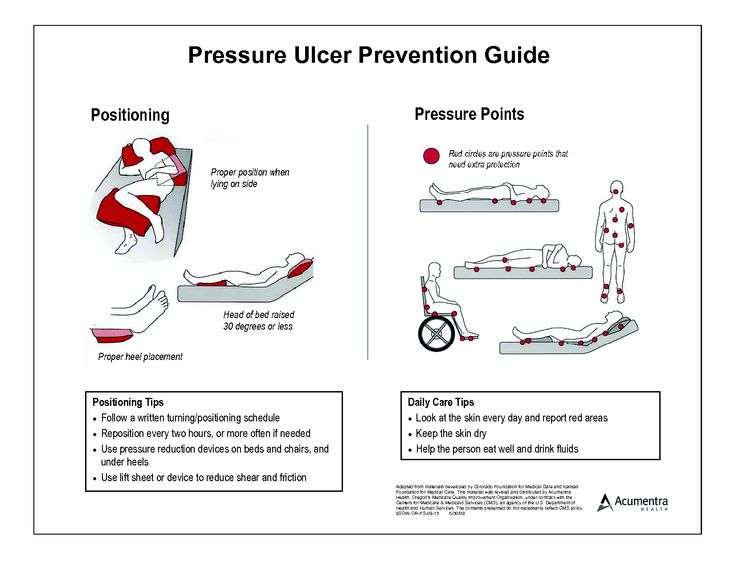
- Use of support surfaces to reduce the magnitude of pressure
- Keeping the head of the bed at or below 30 degrees elevation in order to reduce the risk of shear
- Use of prophylactic dressings to areas frequently exposed to friction and shear
- Turning and repositioning patients to reduce the duration of pressure
- Providing nutrition and hydration to maintain tissue tolerance for pressure
Read Also: Yea Sacc For Horses With Ulcers
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Temperature.
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Also Check: Colon Cancer Symptoms Vs Ulcerative Colitis
Equipment For Relieving Pressure Sores
XSENSORs Continuous Skin Monitoring technology is specifically geared towards helping clinicians effectively position patients to prevent dangerous pressure exposure . By integrating hospital equipment that monitors patient skin and predicts problem areas from the outset of the stay, its much easier to mitigate risks and stop pressure sores before they start.
Family And Individual Level
Healthcare professionals can have an impact on an individual level by:
- recognising the important role individuals, families and carers have in preventing and managing pressure ulcers
- engaging individuals, carers and families in what to look for and how pressure ulcers can be prevented
- using appropriate literature with visual images to explain how quickly pressure ulcers can develop
- educating the individuals and caregivers about the causes, assessment and management of pressure ulcers
- using appropriate terminology recognising and informing patients that pressure ulcers is another term for bed sores
- encouraging individuals to move independently whenever possible
- directing individuals to appropriate healthcare professionals if they suspect a pressure ulcer is forming or is present
- looking out for skin discolouration or soreness, particularly in areas where bones are close to the skin
- repositioning or turning patients frequently at least every 2 hours for those patients who need help
- using moving and handling aids to help reposition individuals who require assistance moving
- performing regular skin inspections to check areas at risk and document pressure areas at least once a day
- checking that patients with pressure ulcer risk factors are registered with a GP and receive primary health care support to minimise the risks
- providing holistic health assessments for people at risk of developing pressure ulcers
Don’t Miss: Foods You Can Eat With An Ulcer
How To Prevent Pressure Ulcers Or Bed Sores
Pressure ulcers are a common problem in palliative care patients. Decreased mobility, increased time spent in bed, and altered nutrition make these patients prime targets for skin breakdown. Pressure ulcers are painful. As a caregiver, one of the most important things you can do to keep your patient comfortable is to prevent one from developing.
Severity Of Pressure Ulcers
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
Also Check: Surgical Management Of Ulcerative Colitis Ppt
What Other Kinds Of Aids Are Available
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while.
Pressure ulcers often occur on peoples heels. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used. But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn’t been much research on aids such as special positioning cushions or special cushions for people to sit on either.
Educating Healthcare Staff To Prevent Pressure Ulcers
Background
Pressure ulcers, also known as bed sores or pressure sores, are often experienced by those who find it difficult to walk and spend long periods of time sitting or lying down. Pressure ulcers can range from patches of discoloured, painful skin, to open wounds that can take a long time to heal. Pressure ulcers are prone to infection and have a great impact on people’s health and well being. To stop these ulcers from developing in people who are at risk, healthcare staff need to be well informed about how to prevent them. It is important to understand what type of information healthcare staff need, how it might best be delivered to them and whether education can prevent pressure ulcers from developing.
Review question
We reviewed the evidence about the effect of the education of healthcare professionals on the prevention of pressure ulcers. We explored all types of education regardless of how it was delivered as long as it focused on preventing pressure ulcers. Healthcare staff included all staff working in pressure ulcer prevention from any professional background. Settings where the care was provided included hospital inpatient and outpatient departments, community clinics, patients’ own homes, and residential or nursing care homes.
What we found
The evidence of this review is up-to-date as of 12 June 2017.
To assess the effects of educational interventions for healthcare professionals on pressure ulcer prevention.
Recommended Reading: Side Effects Of Ulcerative Colitis