Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
You should not use Imodium A-D if you are allergic to loperamide, or if you have:
-
stomach pain without diarrhea
Ask your doctor before using Imodium A-D to treat diarrhea caused by Clostridium difficile.
Ask a doctor before using this medicine if you are pregnant or breastfeeding.
You should not breast-feed while you are using loperamide.
Ulcerative Colitis: Treatment And Therapy
The cause of the inflammatory bowel disease ulcerative colitis is not yet known. Therefore, the goal of treatment is to alleviate the symptoms as well as to prolong the symptom-free phases.
Various drugs are used for this purpose: 5-aminosalicylic acid is an anti-inflammatory agent that is prescribed in the form of the precursor mesalazine as tablets, suppositories, foams or enemas. Corticosteroids also have an anti-inflammatory effect and are used either as suppositories, enemas or tablets. Both medications containing the active ingredient mesalazine and cortisone can cause severe side effects. Cortisone in particular can cause long-term side effects.
In severe cases or when cortisone is not effective, some patients receive immunosuppressants . This can have a positive effect on the course of the disease. However, TNF antibodies , which inhibit the inflammatory messenger TNF, can also be considered. When taking immunosuppressants and TNF antibodies, severe side effects such as susceptibility to infections can also occur, and poisoning is also possible.
Which drugs are used in treatment always depends on various factors, such as the extent of the symptoms and how far the inflammation has spread in the intestine, among other factors.
In addition to drug therapy, it is important for those affected to ensure a varied and balanced diet and to avoid hard-to-digest food components and hot spices during an acute episode.
Also Check: Natural Way To Cure Ulcer
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Can People Inherit Crohns Disease
Crohns disease can run in families, and people can be more likely to develop the condition if a close relative has it.
Between 5 and 20% of people with Crohns disease have a biological relative with some form of IBD. This is usually a brother or sister, and sometimes, it is a parent.
According to the National Human Genome Research Institute, children with one parent with Crohns disease have a lifetime risk of developing the condition and a 10% likelihood of developing some form of IBD.
If both parents have IBD, the risk of their children developing Crohns disease increases to 35%.
However, review authors do not associate the NOD2 gene with disease risk in individuals of Chinese, Malay, or Indian descent that have Crohns disease in the last part of the small intestine, or the ileum.
Moreover, authors of the review suggest that there are 200 genetic regions associated with disease risk, and scientists need to understand further the complexities of inheriting the condition.
- rarely, liver damage
Additionally, people with IBD have a slightly higher risk of developing colon cancer, a liver disease called primary sclerosing cholangitis, and blood clots.
Don’t Miss: Foam Dressings For Leg Ulcers
Diagnosis Of Ulcerative Colitis
X-rays of the abdomen taken after barium is given by enema do not require any special preparation . These x-rays usually can show a blockage or paralysis read more ) may indicate the severity and extent of the disease but are not done when the disease is active, such as during a flare-up, because of the risk of causing a perforation. Other x-rays of the abdomen may also be taken.
What Is An Anti
Chronic diarrhea is a common symptom reported by patients with IBD.3 This can be extremely uncomfortable and negatively impact a patients health and quality of life. Anti-diarrheal medications can be helpful in long-term management of the disease. However, it is important to note that anti-diarrheals will not treat the underlying cause of the diarrhea, which is inflammation in the digestive tract due to IBD. This inflammation can only be treated with medications that specifically target the disease itself, such as aminosalicylates,immunomodulators, corticosteroids, antibiotics, and/or biologic therapies. Over-the-counter symptom management medications such as anti-diarrheals should never be used to replace those IBD medications, only to supplement them. Although anti-diarrheals will not treat the underlying cause of the diarrhea, they may help to mask the symptom and improve a persons quality of life on a day-to-day basis.
An anti-diarrheal is a medication that provides symptomatic relief of diarrhea. The most common anti-diarrheal is loperamide, also known as Imodium. Loperamide is an over-the-counter medication that can be useful in decreasing bowel movement frequency by effectively slowing down the digestive process. This allows for the better absorption of nutrients through the digestive tract. Loperamide also increases the anal sphincter tone at rest. Some other forms of anti-diarrheals, such as diphenoxylate/atropine , are only available with a prescription.1,3
You May Like: How To Heal Mouth Ulcers Fast
Plan B: Mesalazine To Treat Presumed Ulcerative Colitis
I expected to be told I needed another colonoscopy for more biopsies to be taken and sent for histopathological examination. But my gastroenterologist took a more direct approach, which I thought was far more practical: a trial of mesalazine, also known as mesalamine or 5-aminosalicylic acid , in the form of Salofalk 500 mg tablets, one tablet three times daily. This was actually a reduced dosage, in lieu of the intended dosage of Salofalk 1000 mg three times daily. My gastroenterologist being a little cautious due to my expressed concern over the drug being similar, in name and structure, to Aspirin , to which I am highly allergic. He reassured me, and continues to reassure me, that mesalazine is safe for me and for long-term use. My dosage of mesalazine was increased to a more standard one 1000 mg three times daily, i.e. 3 grams per day a few days later.
In addition, I was prescribed Salofalk suppository 500 mg, one to be taken at bedtime. I took the suppositories for about two weeks.
All my other symptoms I believed were linked to UC, listed above, also improved over the ensuing days and weeks. For me, mesalazine was a game changer. Just as tegaserod was for my gastroparesis 12 years earlier.
Ive been taking mesalazine since March 2018 and my UC symptoms have not recurred. So it appears that at least two goals of drug treatment have been achieved: induction of remission, and maintenance of remission.
Response To Initial Treatment
Though the clinical history and colonoscopic findings, on the whole, were most suggestive of UC, my initial treatment was based on the histopathology report. I was prescribed a two-week course of ciprofloxacin and metronidazole, and a 3-day course of albendazole.
To be sure, I never believed my gastrointestinal symptoms were due to an active infection, but I took the antibiotics and antihelmintic regardless. If the antibiotics and/or antihelmintic could eliminate my symptoms, that would have been a fantastic result.
How did I go? In a word: terrible.
Over the next 14 days, my symptoms steadily worsened, despite me taking those meds religiously. Even after a few days, as my diarrhoea, pus and mucus in the stools, and abdominal pain worsened, I knew the thing in my rear-end was definitely not due to a bacterial or tapeworm infection. Nevertheless, I soldiered on with the entire 14-day course of antibiotic treatment, if not for anything else, to prove a point . I called the doctors clinic on the 13th day to make an appointment to see him on the last day of the course of antibiotics. By then, my symptoms were quite severe, almost intolerable.
You May Like: Best Cure For Mouth Ulcers
Disease Course Therapeutic Strategies And Complications
The use of mesalamine as a therapy for induction of remission was similar in the two groups , as well as steroid therapy and surgery . .
Table 2 UC therapeutic strategies, disease course and complications
Globally, surgery was performed more frequently in the elderly , with a mean time between diagnosis and surgery of 18.4months in the elderly and 24.87months in younger patients .
The type of surgery most frequently performed was partial colic resection , followed by perianal disease , colectomy and resection for cancer in the elderly colectomy and perianal disease in adults.
As maintenance therapy, there was no difference between the two groups in the use of mesalamine and immunosuppressant while biologic agents were much less used in the elderly .
During follow up, 57% of patients had at least one disease exacerbation, with a similar median time to first relapse . p 0.5615.
Extraintestinal manifestations were less common in the elderly , . Intestinal complications were more frequent in the elderly . In particular, stenosis was the most frequent complication in both groups. The other ones were toxic megacolon, intestinal perforation and haemoperitoneum.
Moreover, major infections were more common in the elderly . The most frequent infection was pneumonia in both groups . The other ones were sepsis , C. difficile infection for the elderly and CMV infection for the adults . Herpes Zoster infection and systemic candidiasis were also reported.
Disease Extent And Phenotype At The Time Of Diagnosis And At Follow Up
Disease extent was compared in the two groups and within each group, both at the beginning and at maximum follow up. .
Fig. 2
At diagnosis, left colitis was more common in the elderly , while proctitis and extensive colitis , p 0.011) were less common.
During follow up, a variation in the disease extent was found in both groups .
Recommended Reading: Ulcerative Colitis Increased Risk Of Colon Cancer
Study Variables And Statistics
We studied and compared patients with CD and UC, regarding the following variables: follow-up demographic characteristics and clinical data .
Descriptive analysis included absolute and relative frequencies for categorical variables. Quantitative continuous variables with normal distribution were described as means and standard deviations. For those whose normality could not be determined, we described as medians with the first and third quartiles . To compare quantitative variables of normal unpaired distribution, Students t-test for independent samples for two groups was utilized. For unpaired samples that did not assume a normal distribution, the MannWhitney test was used for two groups and one-way ANOVA for comparisons between three groups. To compare categorical variables, the chi-square test for independent samples and the equality of proportions test were performed when appropriate. Descriptive levels of p< 0.05 were considered significant.
Who Is The Risk Of Inheriting Ibd

- There seems to be a stronger risk of inheriting Crohn’s disease than ulcerative colitis, especially in families of Jewish descent.
- Children who have one parent with Crohn’s disease have a 7 to 9% lifetime risk of developing the condition and a 10% risk of developing some form of IBD.
- Children of two parents who have IBD have a 35% risk of developing some form of IBD.
- Approximately 20% of people with IBD have a family member with IBD.
- The risk of IBD for persons who have a family member who has IBD is 10 times higher than for persons in the general population.
- The risk of IBD for persons who have a sibling with IBD is 30 times higher than for persons in the general population.
Other factors, such as diet, use of oral contraceptives, and infections are being studied, but their role is still unclear.
Read Also: Is Ulcerative Colitis The Same As Diverticulitis
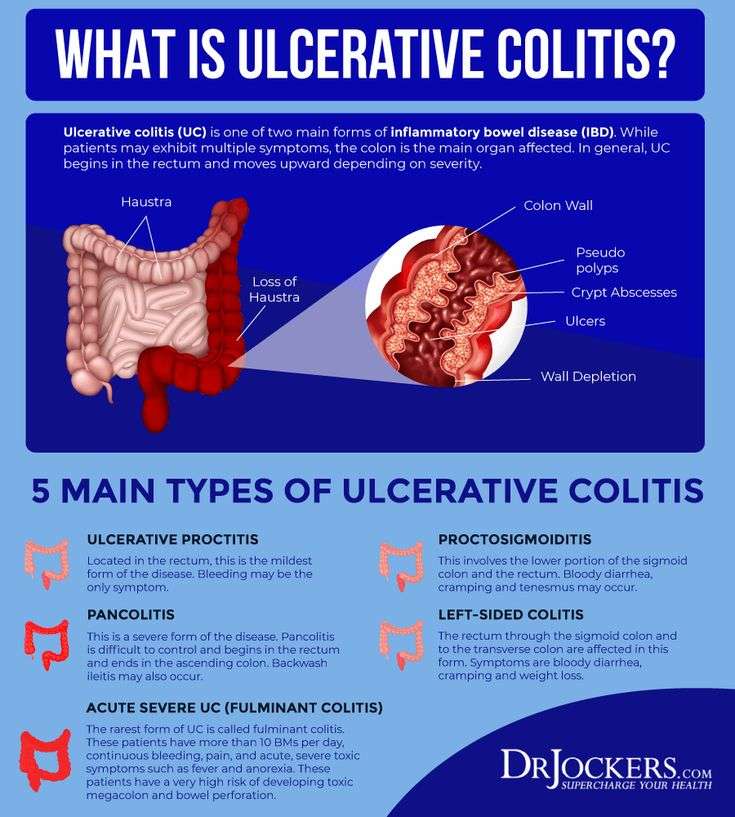
What Is Ulcerative Colitis
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
Also Check: Foods That Cause Stomach Ulcers
How Does Ulcerative Colitis Increase The Risk Of Colorectal Cancer
If you have ulcerative colitis, your risk of developing colon cancer is higher if you have the following conditions:
- An ulcerative colitis diagnosis at a young age
- Had ulcerative colitis for more than eight years
- Ulcerative colitis that affects most of your colon
- Uncontrolled inflammation
- Damage to your liver’s bile duct from inflammation or scarring
- Family history of ulcerative colitis
Cannabinoids Affect Endocannabinoid System In Ulcerative Colitis
An Israeli study published in 2021 investigated the impact of cannabinoid therapy on the endocannabinoid system and clinical symptoms in patients with IBD. The 2-month study examined the effects of THC-dominant cannabis flowers and placebo in Chrons disease and ulcerative colitis. Twenty-two subjects received cannabis and another 27 participants received placebo for smoking. During the course of the study, blood samples and intestinal tissue samples were taken to examine the function of the ECS .
Endocannabinoids and endocannabinoid-like substances examined in the blood :
- anandamide
- arachidonic acid
Enzymes studied on colon tissue :
- N-acylphosphatidylethanolamine-selective phospholipase D : this enzyme is required for the formation of endocannabinoids. NAPE-PLD is used for the biosynthesis of N-acylethanolamines such as anandamide .
- fatty acid amide hydrolase : this enzyme serves to degrade endocannabinoids. FAAH deactivates various fatty acid amides such as anandamide and oleic acid amide .
The studies showed a different function of the ECS in patients depending on the diagnosis : in all 30 affected patients with Crohns disease, endocannabinoids remained unchanged, regardless of whether cannabis or placebo was used.
The study shows that cannabis therapy can positively influence the endocannabinoid system in ulcerative colitis, thereby alleviating symptoms .
You May Like: Signs And Symptoms Of Stomach Ulcers In Adults
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
You May Like: What Should You Eat When You Have Ulcerative Colitis
Demographic Information And Risk Factors
94 patients who have been diagnosed with UC after the age of 65years were compared with 94 patients who have been diagnosed with UC between 40 and 64years. The demographic characteristics of both group are shown in Table . Median age at diagnosis was 71.5±5years and 50.1±6.7years in E-O and A-O, respectively . Male patients were more frequent in both groups . Family history for UC was similar in the two groups . Difference in smoking habits, althoughs not statistically significant was reported. Time between onset symptoms and UC diagnosis was similar in the two groups, 5.8±4.6months in the elderly and 6.2±4.7months in adults respectively. 34% of the elderly and 19% of the adults received a different diagnosis before UC diagnosis. The most frequent one was diverticular disease in the first group , while infectious colitis was the most common in the second group .
Table 1 Demographic characteristics of UC by age
Median follow among elderly patients up was 8.1years and 5.7years in the control group. Mortality was 20.5% in the elderly and 3.9% in adults. p< 0.0005. Main causes of death were cardiovascular disease , sepsis , extraintestinal neoplasia and respiratory failure in the elderly cardiovascular disease , sepsis and extraintestinal neoplasia in adults.