Allergy Or Intolerance Lactose Free Or Non
Lactose free cheese or non-dairy cheese? How do we choose products that are lactose free or dairy free? On a par with tax evasion or tax avoidance, these phrases can be difficult to understand, at first. They are not one and the same, but there are similarities and subtle differences which can catch you out.
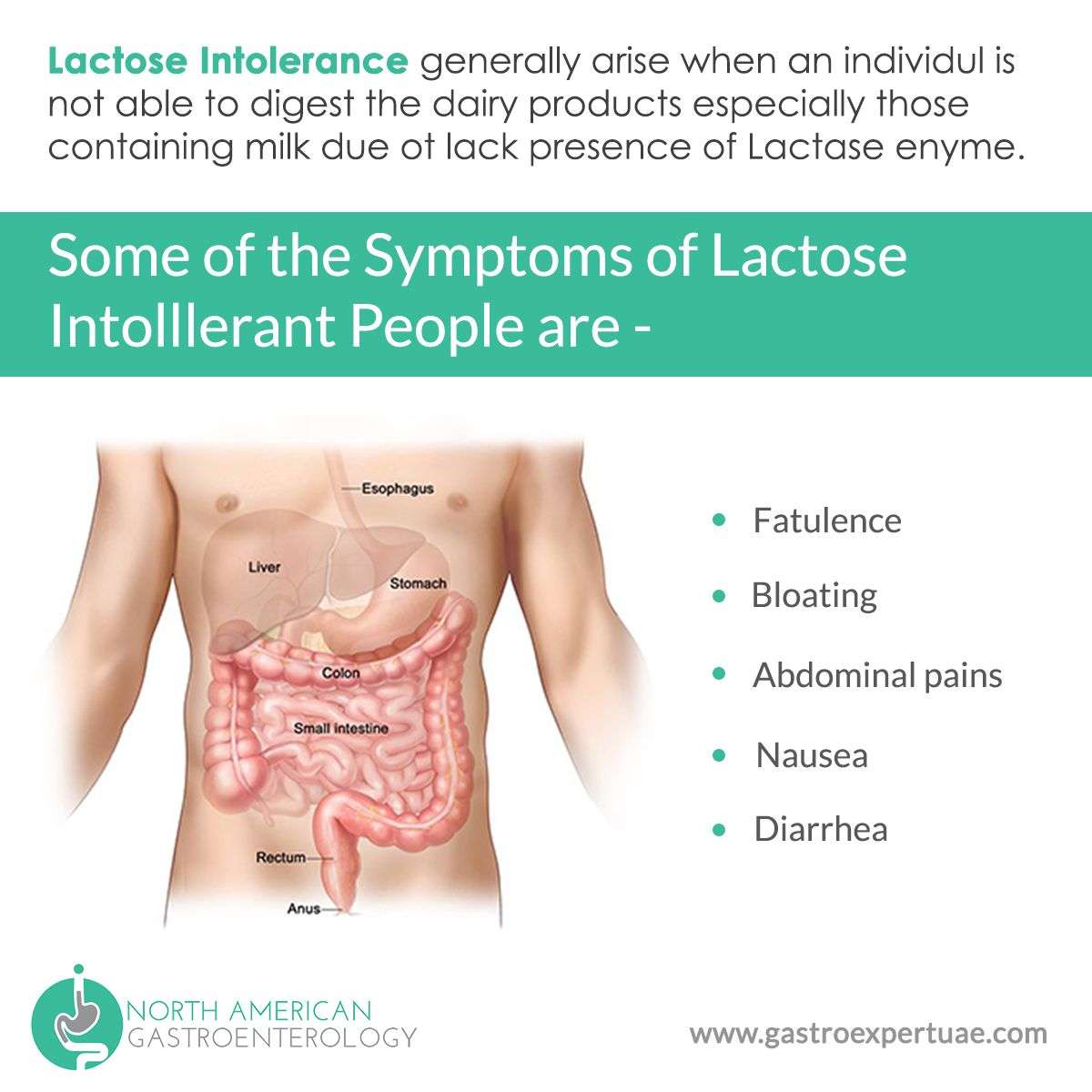
It generally follows that if one suffers from ulcerative colitis, then the inability to digest lactose can compound the problem. A hypersensitive reaction to certain types of food such as dairy is referred to as a food allergy, since it is our immune system which is reacting to the sugars and proteins found in milk products, in a way that doesnt help us to digest the food properly. Conversely, food intolerance refers to an inability to digest certain food types because our digestive system does not produce the requisite lactase enzyme to help breakdown lactose into its constituent glucose and galactose. Symptoms are similar in both conditions and include wind, bloating, stomach cramps and rumbles, diarrhoea, and very rarely even anaphylaxis. Quite often, people complain of feeling bloated or uncomfortable after eating, but put it down to having eaten too much. It is quite possible that they have a degree of lactose intolerance but are unaware of it. In any event, and in particular when associated with ulcerative colitis, consultation with a medical professional would be wise.
Prevalence Of Lactose Maldigestion In Ibd
Description of included studies for meta-analysis
The meta-analysis included a total of 1935 IBD patients and 761 controls. Table outlines demographics of 17 studies . The mean age of participants based on available data was 35.6 years for CD, 40.8 years for UC, and 37.7 years for controls. One study focused exclusively on a pediatric population . Based on reports that specified gender distribution, there were more females in the IBD groups than the control group.
Table 1 Studies of lactose maldigestion in IBD using breath test, lactose tolerance test, jejunal biopsies or urinary sugar ratio tests
Eleven studies originated from countries with low risk for LNP and 4 specified ethnic make-up . Five reports were from moderate risk countries and 1 was from a high risk country .
Twelve studies used a lactose challenge with measurement of BT . One of these also analyzed the C/T-13910 polymorphisms . Two studies used LTT alone . Two evaluated jejunal biopsies and one used urinary lactose/L-arabinose sugar ratio to define LM . Intestinal biopsies , BT and the LTT have been validated against genetic tests for the north European C/T- 13910 lactase polymorphisms .
Outcome of meta-analyses
Fig. 2
Subgroup analysis using BT alone showed similarly that LM was only significant in CD , but not in UC . Fig. shows the forest plots with log OR using breath test only. LTT did not show any statistically significant differences in CD ) or UC ) .
Fig. 3Fig. 4
Gut And Systemic Symptoms
Gastrointesinal symptoms , and systemic symptoms were recorded by the participants 0=no symptoms, 10=severe symptoms up to 48h in a symptom diary. Patients and healthy volunteers were advised on how to assess the severity of any symptoms. This was based on conventional clinical methods and our previous study. Our study shows that an objective, quantitative test for cognitive dysfunction is now required in the clinical management of both IBS and IBD.
Read Also: How To Cure Ulcerative Proctitis
What Are The Symptoms
IBS and lactose intolerance can both cause:
IBS can also cause constipation. You might have mucus in your stool or feel like you canât completely empty your colon. Symptoms can change over time and flare up, get better, or disappear.
Along with the other symptoms, lactose intolerance can cause nausea. You usually start to feel bad between 30 minutes and 2 hours after you eat milk or other dairy products.
What Is The Treatment
Only a doctor can tell if your symptoms come from IBS or lactose intolerance. They usually diagnose IBS based on the symptoms you describe. For lactose intolerance, youâll need to give a little more information, such as:
- Your family history
- A physical exam
- A hydrogen breath test. Undigested lactose in your body gives off high levels of hydrogen. During the test, you drink a beverage that has lactose, then blow air into a special bag. A lab tests your breath to look for the gas.
IBS symptoms can come and go, but itâs a condition youâll have for the rest of your life. There is no cure for it. But you can use a few different strategies to manage how you feel. Changes to your diet and tools to handle stress may help ease your symptoms. Medications like anti-diarrhea drugs or laxatives can make you feel better, too. Itâs important to work with a doctor to find the approach that works for you.
There is also no cure for lactose intolerance, but it usually helps to avoid milk, cheese, and other dairy foods. Some people with the condition can handle small amounts of them, and others have to cut them out completely. Your doctor or dietitian can help you figure out the right diet and suggest supplements that may help. There are lactase enzyme replacements available which can be taken with food, but they have varying degrees of benefit.
Show Sources
Recommended Reading: How To Cure Gastritis And Ulcers Naturally
Newly Diagnosed With Ulcerative Colitis
No matter what you may be feeling upon hearing you have ulcerative colitis, it is of great value to know that you are not alone. Many places have support groups, both in-person and online, for people all ages that can be very helpful.Talk to your health care provider about support groups at their office or the hospital or do your own research to get involved with the ulcerative colitis community.
If you are overwhelmed by your new diagnosis, dont wait toreach out to a mental health expertto talk through the changes. Relaxation techniques, such as yoga, meditation or mindfulness, may be very helpful.
Working together with your health care team, you can make a treatment plan just for you, to help control your symptoms andput you in charge of your ulcerative colitis.
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
ishonestNo.361 – Acne Scars
Doctors arent sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Its most likely if youre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress dont cause it, but they can trigger a flare of symptoms.
Recommended Reading: How Can You Tell If You Have An Ulcer
What To Expect After Your Surgery
Most people do very well after their surgery and are able to return to work and their normal daily activities after they recover.
-
You should expect an adjustment period of up to one year to get used to the changes in your body after your proctocolectomy.
-
You will likely be on liquid or soft food diet for the first few days after surgery. Your doctor will then have you slowly introduce bland solid foods. You should chew your food thoroughly and avoid any foods that may cause gas, diarrhea or anal irritation. Its also important to drink plenty of water. We recommend six to eight glasses a day.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantomrectum and it completely normal. It does not require any treatment and often subsides over time.
-
Your doctor may recommend a physical activity restriction for a minimum of six weeks, depending on what type of surgery you had.
-
Talk to your doctor about resuming normal sexual activity after your surgery. Some people find their sex life improves some time after surgery due to improvements in pain, inflammation, and other ulcerative colitis symptoms.
Symptoms Of Lactose Intolerance
Individuals with insufficient levels of lactase usually experience symptoms as the lactose that has been consumed moves into the digestive tract. The symptoms of lactose intolerance include:
- Diarrhea
- Abdominal pain
- Flatulence
These symptoms usually occur about 30 minutes to 2 hours after the consumption of the offending products. The severity of the symptoms depends on the patient’s age, intolerance level and rate of digestion.
You May Like: Wound Vac For Pressure Ulcers
Diagnosis Of Lactose Intolerance
Lactose intolerance can be difficult to diagnose because the symptoms mimic other conditions. The doctor may perform specific tests to confirm the diagnosis. Tests that may be conducted include the following:
- Lactose tolerance test
- Hydrogen breath test
- Stool acidity test
If these tests are negative, further investigation must be undertaken to find the cause of the patient’s symptoms.
Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
Recommended Reading: Ulcerative Colitis Surgery Pros And Cons
Data Extraction For Meta
Year of publication, country of origin, number of patients and controls, type of test for LM, test outcomes, distribution of CD or UC cases, site of involvement in CD, disease activity at time of testing, and surgical history were recorded from each study. A description of genetic likelihood of LM for patients versus controls was estimated. Each study included in the meta-analysis was graded by country for low , moderate , or high risk , based on classification as per Mishkin and Szilagyi .
What Is Lactose Intolerance

Lactose intolerance is the medical term that is used to describe a condition in which people are unable to digest milk or sugar properly. In fact, this health problem is prevalent and can afflict up to 65% of the worlds population. A recent study has found lactose intolerance is not dangerous but it can cause discomfort to most people, even spoiling their quality of life if there is no immediate and proper treatment being recommended.
Recommended Reading: What To Do When Ulcerative Colitis Flares
Food Labelling For Lactose Free Products
In short, if you know you have an aversion to dairy products, or you suspect that you might, any food that is based on cows milk is best avoided. Even though the lactose might have been removed , they are still dairy products. They should be safe for those of us who suffer a lactose intolerance, but as they contain other derivatives of milk, such as whey and casein, those with dairy allergies need to avoid them. Likewise, products labelled ‘non-dairy’ may still have milk products in them: casein, for example, typically makes up over half of the proteins found in milk produced from cows, and may be present in foods such as cheese which has been labelled ‘non-dairy’. Food labelling in the UK is comprehensive enough to be able to determine whether or not the product is suitable for lactose or dairy-free diets, and known foods and their derivatives are highlighted in bold if they are present and likely to affect some people by way of an allergic reaction or intolerance.
Lactose Challenge Test And Lactose Sensitivity
It is important to distinguish between hypolactasia, assessed either by the polymorpisn CC13910 or through small intestinal biopsy and lactose sensitivity. The key clinical criterion for diagnosing lactose sensitivity in this study was the effect of an oral lactose challenge on breath hydrogen and methane, and the appearance of gut and systemic symptoms. Thus, participants were given 50g lactose as previously described. They were asked not to smoke for 4h prior to the breath test. They had also not received any antibiotic treatment or had bowel preparation for GI investigation in the 4weeks before the study. Lactose sensitivity was defined on the basis of breath analysis for hydrogen and methane over 6h as previously described, together with a record of both gut and systemic symptoms for up to 48h after the lactose challenge. Transit times through the small intestine vary considerably between individuals. This is why, on the basis of our previous study, we measured breath hydrogen and methane up to 6h after the lactose challenge. The initial rise in breath gases can give an indication of the transit time. However, unlike one report in a Greek population, we did not find this to be of value in assessing whether a patient was lactose sensitive or not.
Recommended Reading: How To Check A Horse For Ulcers
Dairy Products And Ibd: Avoiding Them May Not Be Necessary
Many people with Inflammatory Bowel Disease report that their symptoms become worse after consuming dairy products. However, research about food and IBD is controversial. A new meta-analysis investigated the lactose maldigestion prevalence in IBD.
Many people with Crohns disease or Ulcerative Colitis avoid dairy out of fear that it will cause uncomfortable symptoms, such as excess gas, abdominal cramping, and diarrhea. However, not every person with CD or UC is actually lactose maldigester or lactose intolerant, so avoiding all dairy may not be a good option. It could even be counterproductive, because dairy is an excellent source of calcium. This is a particularly important nutrient for people with Crohns disease, as certain drug treatments and malabsorption may cause a calcium deficiency. This literature review was performed to extract data on lactose maldigestion prevalence in IBD.
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesn’t exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
Read Also: Snack Ideas For Ulcerative Colitis
Most Symptoms Of Ulcerative Colitis Relate To Bowel Movements
The symptoms of ulcerative colitis can vary from person to person, based on where the disease is in the body and how bad the inflammation is.
Most common symptoms:
- Diarrhea , which is often the first symptom.
- Blood in the stool.
- Urgency, or immediate need, to go to the bathroom.
- Increased number of bowel movements.
- Belly pain and cramping.
Ulcerative colitis can cause symptoms throughout your body.
You might have weight loss or other symptoms that affect the entire body. The inflammation of ulcerative colitis can also affect your joints or skin, leading to painful joints and skin rashes. During a flare-up, symptoms may go beyond those that affect the digestive system, including:
- Rashes or patches of red, swollen skin.
- Painful or swollen joints.
- Mouth ulcers.
- Red, irritated eyes.
Keep of track of any symptoms, how often you have them, and how bad they are to talk about with your health care provider.
Lactose Malabsorption And Lactose Intolerance In Children With Inflammatory Bowel Diseases
1Department of Pediatrics, Medical University of Silesia, Katowice, Poland
Abstract
Background. Insufficient vitamin D and calcium intake associated with the restricted intake of milk and dairy products can lead to poor health outcomes like malnutrition and abnormal bone mineralization. The aim of the study was to estimate the prevalence of primary and secondary lactose intolerance in children with IBD. Methods. The study included 107 patients which includes 43 patients with Crohns disease , 31 with ulcerative colitis , and 33 children with functional abdominal pain . We analysed the result of the hydrogen breath test with lactose loading, two single nucleotide polymorphisms of the LCT gene . The results were analysed with MedCalc Statistical Software. Results. Adult-type hypolactasia was found in 31% of patients with IBD and 42.4% of AP-FGID . Lactose malabsorption was found in 27.9% of patients with CD, in 22.6% with UC, and in 24.2% with AP-FGID . Lactose intolerance was diagnosed in a similar percentage of patients in each group . Secondary LI in IBD patients does not depend on the location, duration, and activity of the disease and the number of relapses . The median time of lactose-free diet in CD was 10 months and in CU 24 months. . The incidence of LI, LM, and ATH does not differ among children with IBD from the population.
1. Introduction
2. Aims
3. Materials and Methods
4. Results
4.1. Location and Activity of IBD
| Symbol |
4.2. Lactose Intolerance
5. Discussion
Recommended Reading: How To Treat A Diabetic Ulcer