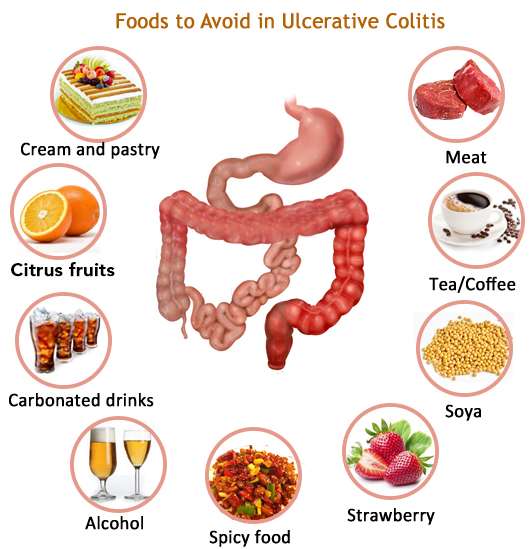
Certain Foods Can Trigger Uc Symptoms In Some People
Has ulcerative colitis made you hesitant to eat for fear of causing painful symptoms? If you know for sure what foods make you feel worse, it’ll be easier to live with the disease. A review published in April 2019 in the journal Current Treatment Options in Gastroenterology noted that people with inflammatory bowel disease who had a diet full of fiber from fruits and vegetables, and low in animal fats, dairy, and processed food, had the fewest flares and best health outcomes. Doctors and nutritionists recommend that people who are diagnosed with ulcerative colitis change their dietary intake to ensure that they are consuming much-needed nutrients without exacerbating symptoms.
Whats the best way to identify what not to eat if you have UC? According to the research review mentioned above, starting an elimination diet for patients with Crohns disease or UC allowed 73 percent of patients to achieve remission in a six-week period. . Elimination diets, where patients remove certain foods from their diet to see if their symptoms abate, are a good way to identify common food triggers.
To get started on one, record all the food you eat during the day in a diary or journal along with any symptoms you experience. You can do this with pen and paper or with phone apps.
Ulcerative Colitis Diet: Advice From A Dietitian
If you have ulcerative colitis, knowing what to eat can be tricky. Its important to customize your food choices based on your current tolerance and health goals. This post will help you understand the current scientific thinking on ulcerative colitis and diet and how to move forward with the approach that is right for you.
We have been working with clients with Crohns disease and ulcerative colitis in our practice for over seven years its an area I am passionate about because of the massive toll these diseases take on peoples quality of life. I also believe that nutrition can play a much larger role in the management of the diseases than is often discussed in the doctors office.
As a dietitian, I believe that the goal of nutrition is more than just ensuring you get all the vitamin D you need. I believe and have seen firsthand in my practice that creating a strong individualized approach to nutrition can help people find healing and learn how to thrive, no matter their diagnosis. Which is why it is frustrating that much of the scientific literature on ulcerative colitis is focused on either associating the risk of disease with certain foods, or acute strategies for securing remission in a flare.
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Recommended Reading: Ulcerative Colitis Flare Up Relief
Directions For Ice Pops
What Should I Eat If I Have Ulcerative Colitis
If you have ulcerative colitis, you should eat a healthy, well-balanced diet. Talk with your doctor about a healthy eating plan.
Ulcerative colitis symptoms may cause some people to lose their appetite and eat less, and they may not get enough nutrients. In children, a lack of nutrients may play a role in problems with growth and development.
Researchers have not found that specific foods cause ulcerative colitis symptoms, although healthier diets appear to be associated with less risk of developing IBD. Researchers have not found that specific foods worsen ulcerative colitis. Talk with your doctor about any foods that seem to be related to your symptoms. Your doctor may suggest keeping a food diary to help identify foods that seem to make your symptoms worse.
Depending on your symptoms and the medicines you take, your doctor may recommend changes to your diet. Your doctor may also recommend dietary supplements.
You May Like: Ulcerative Colitis Worse At Night
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Quick Tips For Nausea
If youre really having trouble keeping things down, here are a few of my tips:
- Be cautious about how much volume youre putting in and what ingredients you may be substituting. If youâre youâre questioning if youâll be able to keep it down at the rate that its dissolving, or wondering if it may just come right back up and leave you back to where you started ⦠consider this.
- Iâve heard of others using cupcake wrappers to poke through and hold the contents that melt if not consumed quickly enough. Cool, huh? But, eating faster doesnât mean better if youâre vomiting. If you find this to be true, consider putting less in each cube.
- Major nausea hack: In the past, Iâve taken a couple of tablespoons of the purée and placed pureed contents into one corner of a few small Ziploc bags. Freeze that, then cut off a very small tip of the corner of the bag, so when youâre ready to eat one, you can consume it at a slower rate.
Dont Miss: Early Symptoms Of Stomach Ulcer
Don’t Miss: Wound Care For Diabetic Foot Ulcers
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Ulcerative Colitis Diet: What To Eat To Manage Symptoms
A tailored diet for ulcerative colitis may provide you with some relief
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system is thought to attack the gut lining, failing to recognise it as part of the body. A focused ulcerative colitis diet may therefore help with the management of symptoms. With the guidance of an IBD team or a dietician, those suffering from ulcerative colitis can be put on an elimination diet in order to identify potential trigger foods, or may be encouraged to keep a food diary in order to track links between certain foods and symptoms.
Those who have undergone surgery or are struggling with an ulcerative colitis flare up may be put on a low residue diet or a low fiber diet in order to manage symptoms and lessen the burden of their disease.
However, ulcerative colitis diets are often unique to the individual, so some experimentation under medical supervision may be necessary to find the right eating pattern for you. An ulcerative colitis diet may not work at all either, so it is important to collaborate with your medical team in order to properly manage your condition.
Don’t Miss: How Can You Get Ulcers In Your Stomach
Dairy Is A Common Trigger Food For People With Ulcerative Colitis
Lactose intolerance is a common issue affecting the general population, as well as people with ulcerative colitis, says Themistocles Dassopoulos, MD, the director of the Baylor Center for Inflammatory Bowel Disease in Dallas. Lactose intolerance prevents you from properly digesting lactose, the sugar found in milk and dairy products, because the small intestine lacks the digestive enzyme called lactase. While dairy doesnt seem to cause UC flares, lactose intolerance can cause symptoms such as abdominal pain and diarrhea that can be mistaken for UC. Avoid dairy products or add lactase supplements to reduce these symptoms.
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Don’t Miss: What Is The Treatment For Ulcerative Colitis
Foods To Eat With Ulcerative Colitis
Understanding inflammatory bowel diseases like ulcerative colitis can be difficult, especially knowing what foods to eat. An ulcerative colitis flare can be exacerbated when eating inflammatory foods. Likewise, one can easily become nutrient deficient if there is a lack of variety in the diet. Here we look into some recommended foods to eat when you have an ulcerative colitis flare.
Your nutrition affects your overall health and well-being. When you do not get the proper nutrients, you can experience ulcerative colitis complications like weight loss, malnutrition, and nutritional deficiencies. Before we dive into the foods that you should eat, here are a few tips that can help improve your health and reduce the frequency of flare ups.
Which Nutrients Are Important In Crohn’s And Colitis
Vitamins and minerals
Your body needs vitamins and minerals to work and stay healthy. Your Crohns or Colitis may stop you absorbing enough vitamins and minerals from your food. Vitamins and minerals that you may not absorb properly include iron, vitamin B12, vitamin D and calcium.Eating a healthy, balanced diet may help improve the level of vitamins and minerals in your body. If blood tests show you have low levels of vitamins and minerals, your doctor or specialist nurse may recommend you take supplements to restore your vitamin and mineral levels.Speak to your doctor, specialist nurse or dietitian if you think you may have low levels of any of these nutrients.
Iron
Having low levels of iron is common in people with Crohns or Colitis. Possible causes include a lack of iron in the diet, blood loss and problems absorbing iron from food. Lack of iron can lead to anaemia, where there are fewer red blood cells to carry oxygen around the body.Common symptoms of anaemia include:
Vitamin B12
Vitamin D
Calcium
Fibre
Its important to speak to a dietitian before cutting down on fibre so you dont miss out on the health benefits. For example, they may suggest that some people cut down on fibre for a short time during a flare-up, before slowly adding it back in to the diet.Fibre-rich foods include:
You May Like: When To Go To The Hospital For Ulcerative Colitis
Ulcerative Colitis Diet: What To Eat In A Flare Up
A low residue diet is often recommended to manage symptoms of ulcerative colitis. The Canadian Society of Intestinal Research outlines residue as the solid contents that stay in the bowel after digestion, with the goal of reducing the number of bowel movements that happen in a day. Residue includes fiber, which is limited to 10-15g per day, but the low residue diet differs from the low fiber diet by including foods that may stimulate frequent bowel movement, such as dairy, caffeine, alcohol and gristly or fatty meat.
Dr Deborah Lee, of Dr Fox Online Pharmacy, recommends the following foods for a low residue diet:
- Low fiber fruit and veg such as melon and bananas, as well as stewed fruit
- Lean protein such as white meat, eggs and tofu
- Refined grains such as white bread, white pasta and oatmeal
- Cooked seedless and skinless vegetables such as cucumber, potato and squash.
Cooking your food may also break down some of the dietary fiber to make it more digestible, as seen in a study in the journal of Plant Foods for Human Nutrition , which indicates that the process of cooking decreases the amount of insoluble dietary fiber in some vegetables.
Can Ulcerative Colitis Cause Me Constipation
Some individuals with Ulcerative Colitis experience constipation. No matter which symptoms you experience, learn how to prevent and treat your Ulcerative Colitis constipation before it affects your quality of life.
In general, Ulcerative Colitis causes inflammation in the large intestine and the rectum. When the inflammation associated with UC is concentrated in the rectum, you are likely to feel constipated. This happens because the inflammation in the rectum makes it difficult to pass stool out of your body. This form of Ulcerative Colitis is called proctitis. For individuals with proctitis, constipation may be accompanied by bleeding and a sense of urgency that are usually experienced with diarrhea. However, because the inflammation associated with proctitis is concentrated to the rectum the large intestine can successfully absorb water, which prevents diarrhea.
- Association / Trigger with other Gastrointestinal Symptoms: including gas and stomach pain, which may further complicate Ulcerative Colitis.
Read our full discussion of Ulcerative Colitis and constipation here.
Recommended Reading: How To Cure Colon Ulcers
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
What About A Low Fodmap Or Other Diets
FODMAP stands for fermentable oligosaccharides, di-saccharides, mono-saccharides, and polyols. They are the carbohydrates found in foods and they draw water into the colon, which can make you feel bloated and uncomfortable. FODMAPs also dont pass through your gut quickly but can ferment and hang around for a time, which can cause colitis symptoms.
FODMAPs include:
- Any foods with lactose, or dairy ingredients
- Foods with fructose, including natural fruits, honey, or processed high-fructose corn syrup
- Fructans like garlic, onions, or wheat
- Galactans, which are beans, lentils, or soybeans
- Polyols such as fruits with seeds like apples, avocados, cherries, figs, and peaches
There are other types of diets such as a specific carbohydrate diet that cuts starchy potatoes and grains. Some people have found relief on a Mediterranean diet that includes vegetables, whole grains, fruits, fish, and poultry. A gluten-free diet could also lessen your symptoms.
Also Check: Dakins Solution For Pressure Ulcers
Read Also: Ulcerative Colitis Mouth Sores Pictures
Probiotics For Ulcerative Colitis
The balance of “good and bad bacteria within the gut likely plays a role in the development of Ulcerative Colitis. The beneficial bacteria within your gut help with digestion and maintaining colon health. The detrimental bacteria trigger the bodys immune system to send immune cells to the intestine. The constant presence of these immune cells in the intestine leads to chronic inflammation, which is associated with Ulcerative Colitis symptoms. This is where probiotics come in.
Probiotics may help relieve Ulcerative Colitis symptoms by restoring a healthy balance of bacteria within your intestine. When beneficial bacteria are added to the gut and balance is achieved, the immune system no longer needs to send cells to the area and the inflammation resolves along with your Ulcerative Colitis symptoms.
If you do begin taking a probiotic supplement, it may not have an immediate effect on your Ulcerative Colitis symptoms. You will need to take a probiotic supplement for at least seven to ten days to begin to build up the good bacteria in your gut. Additionally, to continue to see their benefits, you will need to continue to take the probiotics. Stopping the supplement may even shift the balance of bacteria in a negative way and trigger a flare.