What Are The Complications Of Ulcerative Colitis
Ulcerative colitis may lead to complications that develop over time, such as
- anemia, a condition in which you have fewer red blood cells than normal. Ulcerative colitis may lead to more than one type of anemia, including iron-deficiency anemia and anemia of inflammation or chronic disease.
- bone problems, because ulcerative colitis and corticosteroids used to treat the disease can affect the bones. Bone problems include low bone mass, such as osteopenia or osteoporosis.
- problems with growth and development in children, such as gaining less weight than normal, slowed growth, short stature, or delayed puberty.
- colorectal cancer, because patients with long-standing ulcerative colitis that involves a third or more of the colon are at increased risk and require closer screening.
In some cases, ulcerative colitis may lead to serious complications that develop quickly and can be life-threatening. These complications require treatment at a hospital or emergency surgery. Serious complications include
Severe ulcerative colitis or serious complications may lead to additional problems, such as severe anemia and dehydration. These problems may require treatment at a hospital with blood transfusions or intravenous fluids and electrolytes.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
You May Like: Over The Counter Medication For Ulcerative Colitis
Remember Tell Your Doctor Right Away If You Have An Infection Or Symptoms Of An Infection Including:
- Fever, sweats, or chills
- Warm, red, or painful skin or sores on your body
- Diarrhea or stomach pain
- Urinating more often than normal
- Feeling very tired
HUMIRA is given by injection under the skin.
This is the most important information to know about HUMIRA. For more information, talk to your health care provider.
Uses
HUMIRA is a prescription medicine used:
- To reduce the signs and symptoms of:
- Moderate to severe rheumatoid arthritis in adults. HUMIRA can be used alone, with methotrexate, or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Moderate to severe polyarticular juvenile idiopathic arthritis in children 2 years of age and older. HUMIRA can be used alone or with methotrexate.
- Psoriatic arthritis in adults. HUMIRA can be used alone or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Ankylosing spondylitis in adults.
- Moderate to severe hidradenitis suppurativa in people 12 years and older.
US-HUM-210186
Reference: 1. HUMIRA Injection . North Chicago, IL: AbbVie Inc.
What Is A Flare

When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Read Also: Foods You Should Not Eat With Ulcerative Colitis
Treatment Options For Crohns Disease
Recommended treatments may vary based on your symptoms and specific health history.
If you have mild to moderate Crohns disease your doctor may recommend:
- Aminosalicylates, like sulfasalazine
If you have moderate to severe Crohns disease, your doctor may recommend:
- Corticosteroids, such as prednisone and prednisolone
- Immunomodulators, like azathioprine and 6-mercaptopurine
- Biologics, like vedolizumab , adalimumab , infliximab , and ustekinumab
If you have severe Crohns disease or an acute flare-up, your doctor may recommend:
- Intravenous corticosteroids, such as methylprednisolone
Regardless of your level of severity, your doctor may prescribe broad-spectrum antibiotics if you have any abscesses or fistulas.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Don’t Miss: How To Calm An Ulcer
Ibd And Changing Your Diet
Some dietary changes that may help a person with IBD include:
- Low-fibre diet when IBD is active, most people find a bland , low-fibre diet helps to ease diarrhoea and abdominal cramping. People with Crohns disease who have a narrowed small intestine may need to eat a low-fibre diet most of the time.
- Low-fat diet people with Crohns disease who experience steatorrhoea may benefit from a low-fat diet.
- Low-lactose diet the milk sugar lactose is broken down by the enzyme lactase, commonly found in the lining of the small intestine. Some people with Crohns disease lack this enzyme, so should avoid milk and other dairy products. Lactose intolerance can be diagnosed with a simple test ask your doctor.
- Liquid diet a person with severe Crohns disease may need a nutritionally balanced liquid diet.
- Plenty of water people with IBD need to drink plenty of fluids to prevent dehydration.
Also Check: How Does Alcohol Affect Ulcerative Colitis
Causes Of Ulcerative Colitis
Ulcerative colitis is the result of several factors that are not yet well understood. Abnormal immune response, genetics, microbiome, and environmental factors all contribute to ulcerative colitis.
Research suggests that ulcerative colitis could be triggered by an interaction between a virus or bacterial infection in the colon and the bodys immune response.
-
Typically, the cells and proteins that make up your immune system protect you from infection.
-
A normal immune response would cause temporary inflammation to combat an illness or infection. The inflammation would then go away once you are healthy and free of the illness.
-
In ulcerative colitis patients, the inflammation persists long after the immune system should have finished its job. The body continues to send white blood cells into the lining of the intestines, where they produce chronic inflammation and ulcers.
Recommended Reading: Can You Drink Coffee With Ulcerative Colitis
Goals Of Ulcerative Colitis Treatment
At the IBD Center, our goals for treating your childs ulcerative colitis are to:
- Restore balance and health to your childs body
- Relieve any pain or other symptoms caused by ulcerative colitis
- Make sure your child is getting good nutrition
- Restore your childs growth and development
- Ensure your child builds the best bone density
- Help your child and family with the mental, emotional and social effects of IBD
Is Ulcerative Colitis Curable
Ulcerative colitis can differ from person to person, but its usually a lifelong condition. Symptoms come and go over time.
Youll have flare-ups of symptoms, followed by symptom-free periods called remissions. Some people go years without any symptoms. Others experience flare-ups more often.
Overall, about half of people with ulcerative colitis will have relapses, even if theyre being treated.
Youll have the best outlook if the inflammation is only in a small area of your colon. Ulcerative colitis that spreads can be more severe and harder to treat.
The one way to cure ulcerative colitis is with surgery to remove your colon and rectum. This is called proctocolectomy. Once your colon and rectum are removed, youll also be at lower risk for complications like colon cancer.
You can improve your own outlook by taking good care of your ulcerative colitis and getting regular checkups to look for complications. Once youve had ulcerative colitis for about eight years, youll also need to start having regular colonoscopies for colon cancer surveillance.
It can be helpful to talk to others who understand what youre going through. IBD Healthline is a free app that connects you with others living with ulcerative colitis through one-on-one messaging and live group chats, while also providing access to expert-approved information on managing the condition. Download the app for iPhone or Android.
Also Check: Ulcer On Eye From Contact Lens
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
What To Eat During A Flare
All of the diets above are intended to be temporary and followed during a flare-up. Working with a dietitian can help prevent deficiencies in certain micronutrients, which is common with IBD.
During a flare its helpful to eat four to six small meals per day rather than fewer larger meals. Its also very important to drink fluids because diarrhea can occur with a flare and cause dehydration.
Recommended Reading: What Causes Ulcers On The Feet
Don’t Miss: How To Sleep With Stomach Ulcer
Ulcerative Colitis Vs Crohns Disease Vs Irritable Bowel
Other gut diseases can have some of the same symptoms.
- Ulcerative colitis affects only your large intestine and its lining.
- Crohnâs disease causes inflammation, but it affects other places in your digestive tract.
- Irritable bowel syndrome has some of the same symptoms as UC, but it doesnât cause inflammation or ulcers. Instead, itâs a problem with the muscles in your intestines.
How You May Feel
Ulcerative colitis attacks the lining of your digestive tract. It causes swelling and sores in the lining.
If youâve just been diagnosed with it, hereâs what might happen during a flare-up:
You might have some of those symptoms, but not all. And they may change over time. They can range from very mild to very bad.
Also Check: Foods To Treat Ulcerative Colitis
What Should I Tell My Doctor Before Starting Humira
Tell your doctor about all of your health conditions, including if you:
- Have an infection, are being treated for infection, or have symptoms of an infection
- Get a lot of infections or infections that keep coming back
- Have TB or have been in close contact with someone with TB, or were born in, lived in, or traveled where there is more risk for getting TB
- Live or have lived in an area where there is an increased risk for getting certain kinds of fungal infections, such as histoplasmosis, coccidioidomycosis, or blastomycosis. These infections may happen or become more severe if you use HUMIRA. Ask your doctor if you are unsure if you have lived in these areas
- Have or have had hepatitis B
- Are scheduled for major surgery
- Have or have had cancer
- Have numbness or tingling or a nervous system disease such as multiple sclerosis or Guillain-Barré syndrome
- Have or had heart failure
- Have recently received or are scheduled to receive a vaccine. HUMIRA patients may receive vaccines, except for live vaccines. Children should be brought up to date on all vaccines before starting HUMIRA
- Are allergic to rubber, latex, or any HUMIRA ingredients
- Are pregnant, planning to become pregnant, breastfeeding, or planning to breastfeed
- Have a baby and you were using HUMIRA during your pregnancy. Tell your babys doctor before your baby receives any vaccines
Symptom Development And Flares
The symptoms of UC usually start out fairly mild, such as slightly looser or more frequent bowel movements. The symptoms may become more severe as inflammation worsens and open sores develop in the bowel. Eventually, a person with UC might experience fatigue, fever, nausea, and weight loss.
Some people experience ulcerative colitis constantly. However, it is more common to have flare-ups, during which symptoms begin or worsen, followed by periods of remission, when symptoms go away or improve for a while.
Also Check: Can Alcohol Cause Stomach Ulcers
Can The Immune Response To Covid
byKate Kneisel, Contributing Writer, MedPage Today March 1, 2022
A 50-year-old male patient presented to an outpatient clinic in the spring of 2020 with fever and dyspnea he told clinicians that the symptoms had persisted for the past 3 days.
Physical examination findings included a fever of 37.8°C , respiratory rate of 24 breaths/min, and heart rate of 105 beats/min. There was no organomegaly, and the patient was a non-smoker.
Initial laboratory test findings included:
- White blood cell count: 6.4 × 109/L
- C-reactive protein : 4.6 mg/L
- Ferritin: 162 ng/mL
- D-dimer: 842 ng/mL
Findings of a polymerase chain reaction test for SARS-CoV-2 were negative. However, the patients wife and two children had positive PCR test results and the patients CT chest scan revealed diffuse ground-glass opacities consistent with viral pneumonia. Clinicians diagnosed him with COVID-19, and he was started on a now-debunked 7-day regimen of hydroxychloroquine and azithromycin. Once he was clinically stable, he was released with instructions to return for a follow-up assessment.
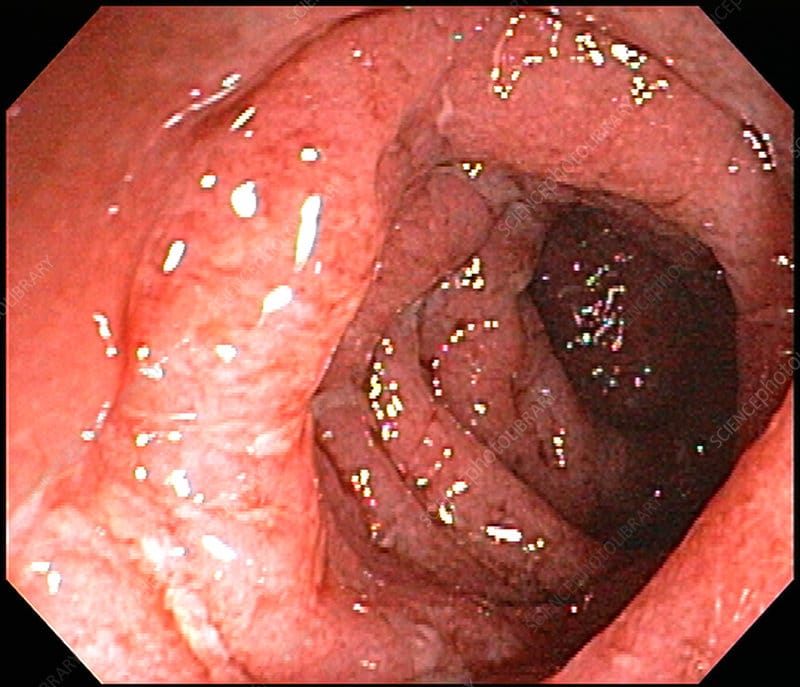
On follow-up assessment 1 week later, the patient reported no improvement in symptoms. His stool calprotectin level was 1800 g/g . Endoscopy revealed a diffuse, micro-ulcerated, granulated appearance that clinicians noted continued uninterrupted from the dentate line to the sigmoid colon, as well as distortion of the submucosal vascularization.
Discussion
You May Like: How To Treat Ulcerative Colitis Pain
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your . Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
You May Like: Is Ulcerative Colitis Considered An Autoimmune Disease
Comparative Effectiveness Of Csa And Ifx
The decision on whether to use CsA or IFX as a rescue agent in steroid-refractory ASUC is a combination of efficacy, safety and patient or provider preference and experience of use.36 Advantages of CsA include the rapid onset of action, shorter half-life and ability to transition to other concomitant immunosuppressive agents on discharge that can be used with other novel biologic therapies including anti-TNF agents. The advantages of IFX include the ability to monitor drug concentrations with a clear understanding of thresholds to achieve efficacy outcomes and the lack of other side effects seen with CsA that can be difficult to manage .
Taken together, these studies therefore suggest that CsA and IFX are comparable in terms of efficacy and safety profile, and the decision on which agent to use is a combination of preference, provider comfort and experience, and patient-specific factors.45