How Is Treatment Of Crohns Disease Different From Ulcerative Colitis
Although the medications may seem similar, there are differences in how Crohns disease and ulcerative colitis are treated. Many medication classes treat both conditions, so there is a lot of overlap. However, there are enough differences that getting the right diagnosis is important. For example, people with ulcerative colitis usually take aminosalicylates, while only a limited number of people with Crohns disease will benefit from these medications. When it comes to more advanced therapies like biologic agents, some can only be used for ulcerative colitis and some can only be used for Crohns disease.
Getting the correct diagnosis can be tricky. Sometimes it might look like you have ulcerative colitis at first, but later your providers will find out that its actually Crohns disease. Work closely with them to be sure you get the right treatment.
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
You May Like: Signs I Have An Ulcer
What Questions Should I Ask My Healthcare Provider
You may want to ask your healthcare provider:
- What type of IBD do I have?
- Whats the best treatment for me?
- What foods or drinks should I avoid?
- What lifestyle changes should I make?
- Am I at risk for other problems?
- Should I look out for signs of complications?
A note from Cleveland Clinic
Most people with inflammatory bowel disease enjoy active lives. Still, symptoms of Crohns disease and ulcerative colitis can be life-disrupting. Some people go into remission after taking medications. Some people need surgery to deal with severe symptom flare-ups. Your healthcare provider can suggest dietary and lifestyle changes to manage IBD.
Last reviewed by a Cleveland Clinic medical professional on 05/03/2021.
References
Are Inflammatory Bowel Diseases Different From Irritable Bowel Syndrome
Yes! IBD and IBS are very different, even though the symptoms can be similar. Most importantly, the treatments are not the same. Working with your provider to figure out what condition you have is important so that you can find the best treatment.
IBS is much more common than IBD. About 11% of people have IBS. That makes it about 10 times more common than IBD.
Fortunately, its also less serious. IBD is caused by inflammation and damage to the GI tract. With IBS, this isnt the case. IBS is a collection of gut symptoms caused by unusual functioning of the bowel.
Also Check: Oats For Horses With Ulcers
Growth And Development Problems For Children
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
Which Signs And Symptoms Of Ibd Vs Ibs Are Different
Signs and symptoms unique to inflammatory bowel disease include:
- Diarrhea that may be bloody
Stress can affect both conditions. In inflammatory bowel disease, stress can cause flare-ups of Crohns disease and ulcerative colitis. Stress may cause gastrointestinal symptoms of IBS to worsen, so you may be more aware of them. Stress also can trigger symptoms because of how they can affect your daily life.
Don’t Miss: Besivance Dosage For Corneal Ulcer
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Symptoms Of Ulcerative Colitis
The symptoms of ulcerative colitis occur in flare-ups. Sometimes, a flare-up is sudden and severe, causing violent diarrhea that typically contains mucus and blood, high fever, abdominal pain, and occasionally peritonitis Peritonitis Abdominal pain is common and often minor. Severe abdominal pain that comes on quickly, however, almost always indicates a significant problem. The pain may be the only sign of the need for surgery… read more . During such flare-ups, the person is profoundly ill. More often, a flare-up begins gradually, and the person has an urgency to have a bowel movement , mild cramps in the lower abdomen, and visible blood and mucus in the stool. A flare-up can last days or weeks and can recur at any time.
When the disease is limited to the rectum and the sigmoid colon, the stool may be normal or hard and dry. However, mucus containing large numbers of red and white blood cells is discharged from the rectum during or between bowel movements. People may or may not have mild general symptoms of illness, such as fever.
Don’t Miss: What To Eat To Cure Ulcer
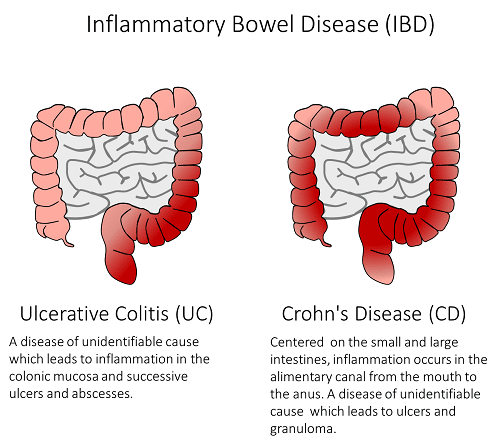
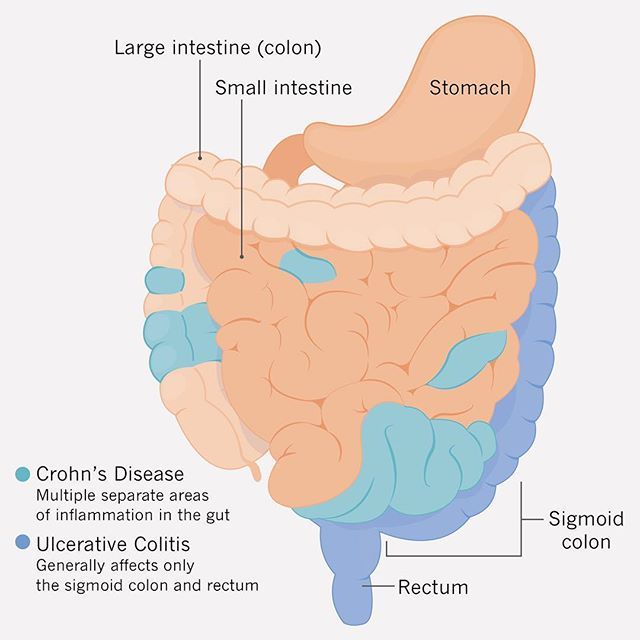
What Is Ulcerative Colitis
Ulcerative colitis belongs to a group of chronic conditions known as inflammatory bowel diseases , and affects the colon, also known as the large intestine. The severity of symptoms may vary and can include abdominal pain, bowel urgency, diarrhea, and blood in the stool. The inflammation begins in the rectum and extends up the colon in a continuous manner. It is important to know that ulcerative colitis is not the same as Crohns disease, another type of IBD. In ulcerative colitis, only the innermost lining of the colon is inflamed and often involves the rectum, but depends on the location of the disease.
No one knows exactly what causes ulcerative colitis and no one can predict how this disease- once it is diagnosed- will affect a person. Some people go for years without having any symptoms, while others have more frequent flare ups .
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Recommended Reading: What Foods To Eat When You Have Ulcerative Colitis
Treatment Options For Ulcerative Colitis
Ulcerative colitis involves more than just medications and symptoms. It is a life changing condition that you are learning to manage, and it represents only part of your story. As you continue your journey with ulcerative colitis while in college, there may be many questions that you will have to navigate in order to help make your experience rewarding. This Campus Connection website will cover some helpful tips and information that you should know before, and during college, and offers a way for you to potentially connect with others like you.
Read our Living with Ulcerative Colitis brochure to learn more about the disease, treatment and daily living.
- Campus Connection
What Causes Ibs And Who Gets It
Someone you know fo sho has IBS, even if you dont know it. Thats because IBS is among the most common disorders diagnosed by doctors. About 11 percent of the population worldwide and about 12 percent of people in the U.S. have it, though some estimates are as high as 20 percent.
The cause of IBS remains unknown, and theres currently no known cure .
Those more likely to get IBS may include:
Women with IBS often report increased symptoms during their period.
Also Check: Is Olive Oil Good For Ulcerative Colitis
Irritable Bowel Syndrome Myths
Irritable bowel syndrome is so common that it is likely you know at least one person with this functional disorder. In 2003, the Canadian Society of Intestinal Research advocated to mayors across Canada and succeeded in having April declared as IBS Awareness Month, yet the myths and misinformation surrounding IBS are pervasive. Read on as we dispel some of these common myths.
Can Ibs Cause Depression
Absolutely. Does IBS make you happy or sad? IBS can be very debilitating and therefore can cause people to be depressed. It used to be common to treat IBS with antidepressants . Unfortunately, this will rarely cure IBS and is not addressing the cause of the IBS. Many studies have documented a link between IBS and depression as well as anxiety, as described in the European Archives of Psychiatry and Clinical Neuroscience.
You May Like: Stomach Ulcer Blood In Stool
Also Check: Can An Ulcer Make You Nauseous
Treatment Of Ulcerative Colitis
Vedolizumab is a drug for people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect it causes is increased susceptibility to infection. Vedolizumab has a theoretical risk of a serious brain infection called progressive multifocal leukoencephalopathy Progressive Multifocal Leukoencephalopathy Progressive multifocal leukoencephalopathy is a rare infection of the brain that is caused by the JC virus. People with a weakened immune system are most likely to get the… read more because this infection has been reported with the use of a related drug called natalizumab.
Ustekinumab is another kind of biologic agent given to people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The first dose is given by vein and then by injections under the skin every 8 weeks. Side effects include injection site reactions , cold-like symptoms, chills, and headache.
How Is Ibd Treated
The aim of treatment is to heal the intestines and confirm this on repeat endoscopy. Even though a medical cure is not yet possible, control of symptoms and disease can be very effective in majority of patients. The number of medications available continues to increase and new treatments can be expected in the future. The most common medications used to treat IBD are:
- Antibiotics such as metronidazole and ciprofloxacin
- ASA anti-inflammatory drugs such as Asacol®, Azulfidine®, Colazol®, Pentasa®, Rowasa® and Lialda®
- Steroids, such as prednisone, prednisolone or budesonide
- Immunomodulators such as Imuran®, Purinethol®(6MP, and methotrexate
- Biologics, such as Remicade®, Inflectra Humira®, Cimzia®, Entyvio®, Stelara® and Xeljanz®
- Nutritional therapy can be used to induce and maintain remission in Crohns disease
Don’t Miss: Chicken Recipes For Ulcerative Colitis
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Ibd And Changing Your Diet
Some dietary changes that may help a person with IBD include:
- Low-fibre diet when IBD is active, most people find a bland , low-fibre diet helps to ease diarrhoea and abdominal cramping. People with Crohns disease who have a narrowed small intestine may need to eat a low-fibre diet most of the time.
- Low-fat diet people with Crohns disease who experience steatorrhoea may benefit from a low-fat diet.
- Low-lactose diet the milk sugar lactose is broken down by the enzyme lactase, commonly found in the lining of the small intestine. Some people with Crohns disease lack this enzyme, so should avoid milk and other dairy products. Lactose intolerance can be diagnosed with a simple test ask your doctor.
- Liquid diet a person with severe Crohns disease may need a nutritionally balanced liquid diet.
- Plenty of water people with IBD need to drink plenty of fluids to prevent dehydration.
Read Also: Ulcerating Breast Cancer Life Expectancy
Diagnosing Inflammatory Bowel Disease
To diagnose Crohns disease or colitis, we start with a comprehensive examination and collecting a thorough history. A number of tests are needed to confirm diagnosis. They may include:
- Colonoscopy and flexible sigmoidoscopy: Used for initial diagnosis, both use a thin, flexible tube with camera to examine different areas, including the colon, small intestine and large intestine to see any ulcers, bleeding and inflammation.
- Upper endoscopy: Uses a thin, flexible tube with camera inserted through the mouth, following the tract to the stomach and upper small intestine to look for bleeding, ulcers and inflammation.
- Capsule endoscopy: A capsule containing a camera is swallowed by the patient to take pictures along the digestive tract not easily reachable by other procedures .
- Laboratory tests: Blood work plus stool samples to check for bacteria and intestinal bleeding.
- CT interography and MR interography: Specialized radiology tests that evaluate the small intestine, an area of the gastrointestinal tract that is beyond the reach of colonoscopy and upper endoscopy, but is often where Crohns disease is present.
- Imaging tests: Collaborating with experts in Radiology for imaging and interpreting gastrointestinal abnormalities, including abdominal x-rays, barium enema, computed tomography , fistulogram and MRI.
How Are Ibs Crohns And Ulcerative Colitis Different
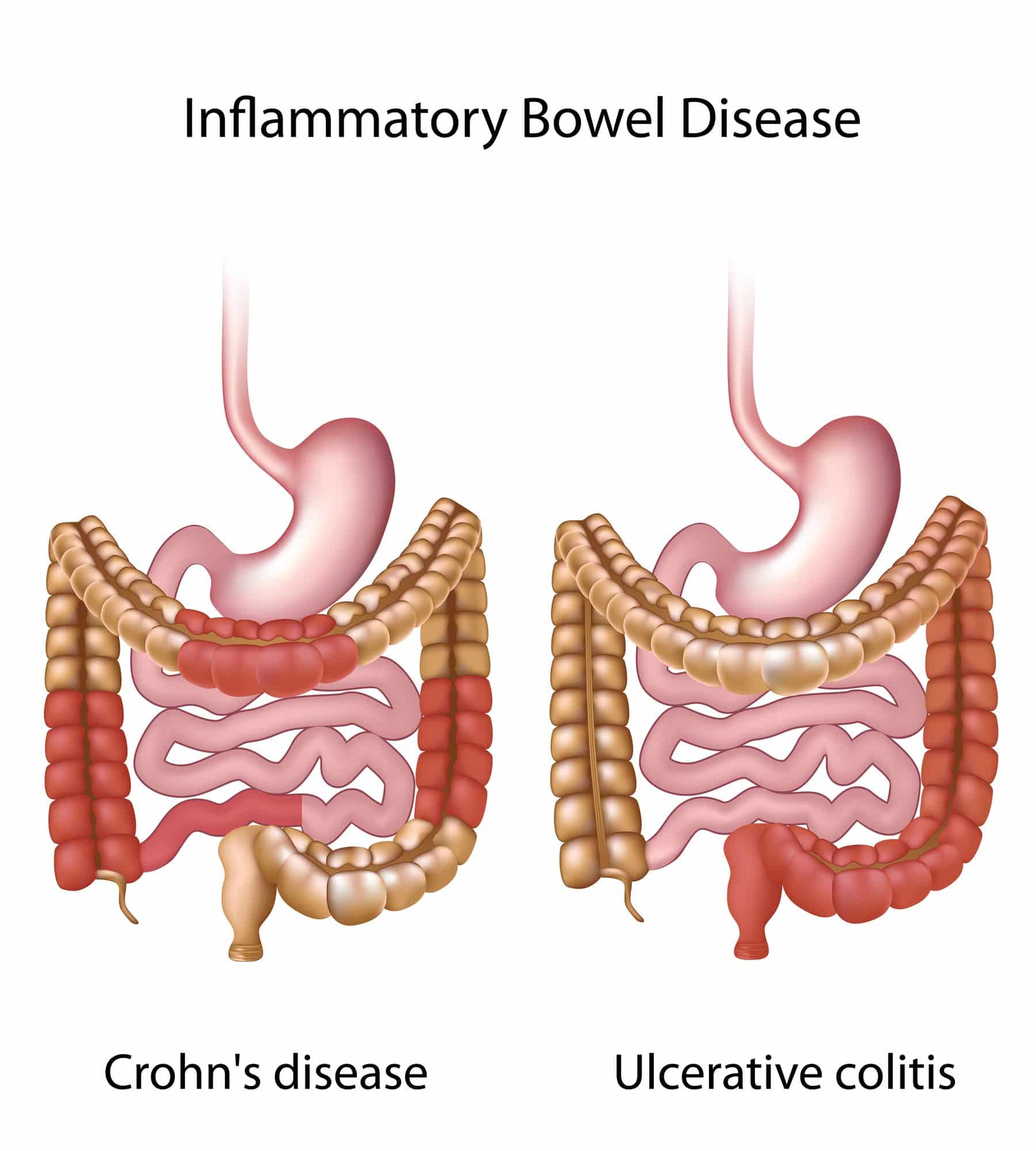
The short answer is Crohns disease and ulcerative colitis are both types of inflammatory bowel disease , which causes chronic inflammation of the intestines.
Irritable bowel syndrome , is a different noninflammatory condition that also affects the intestines .
If your heads spinning over gut disorders, dont worry, we gotchu. Heres the lowdown on Crohns and ulcerative colitis , and IBS.
Also Check: What Can You Eat With A Peptic Ulcer
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
What Are The Causes Of Ibd And Ibs
The exact causes of both IBD and IBS are not clear. With IBD, your genes play a strong role, and it runs in families. There are also many other things that can contribute, such as certain foods, smoking , and missing medication doses. With IBS, many factors are thought to be involved, but stress and diet play a big role. Sometimes people develop IBS after infections as well.
Recommended Reading: Low Sulfur Diet Ulcerative Colitis