Gut Bacteria And Ulcerative Colitis
Imbalances in the gut microbiome have been linked with the onset of IBD. This is likely due to an inappropriate immune response to the gut bacteria leading to inflammation.
Its also been noted that in those with IBD, there are imbalances in the gut bacteria. This bacterial imbalance is referred to as dysbiosis and is seen as a reduction in the diversity of the gut bacteria. This also results in a reduced number of specific beneficial bacteria that have anti-inflammatory properties.
Have Medications At The Ready
When was the last time you checked that your stash of anti-diarrheal drugs arent expired? Make sure you do this on the regular so you have what you need when you need it. Stocking up on Imodium is important, Dr. Nandi says. You might even want to ask if youd be better off with prescription strength, says Dr. Nandi. You can also ask your M.D. to prescribe you some extra meds or suppositories for a future flare, Dr. Nandi suggests. Fill them ahead of time , and tell your doc when you start taking them.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medication such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as the colon becoming stretched and enlarged or developing large ulcers. Both of these can increase the risk of developing a hole in the bowel.
If medications arent effective at controlling your symptoms, or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Read more about:
Read Also: Food For Ulcer Patient In Nigeria
Don’t Miss: What Do You Do If You Have A Bleeding Ulcer
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Keep Up With Regular Physicals

Getting an annual physical is always smart, but its especially important if you have UC.
During the checkup, your healthcare provider will ask whether your treatments are going well and ensure that screening is performed at the appropriate intervals to catch any cancer in the early stages. Even if your UC symptoms are in remission , seeing a healthcare provider regularly can help ensure that you stay on the healthy track.
Recommended Reading: Best Nsaid For Stomach Ulcers
Read Also: How To Diagnose Gastric Ulcer
Give Yourself Some Tlc
Stress doesn’t cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
10
Manage Symptoms Of A Flare
While you work with your doctor to get your flare under control, you can take steps to ease certain symptoms:
Pain. Experts say acetaminophen is the safest way to get pain relief. If it doesnt help you enough when you have pain in your stomach or another body part, ask your doctor what other meds theyd recommend.
Sometimes UC is linked to pain beyond your gut. If you get eye pain or if your eyes feel sensitive to light, see a doctor called an ophthalmologist as soon as possible. Some people living with UC develop eye problems that need fast treatment.
If you have leg pain or pain in another large joint, it might be due to arthritis linked to your UC. Your doctor may tell you to rest the joint that hurts. They may also recommend that you occasionally soothe it with moist heat, like from a warm bath or heated wash cloth. You could also ask the doctor if physical therapy might help.
Irritated bottom. Keep it clean with moist wipes and protect it with diaper cream. You could also soak in a saltwater bath.
Diarrhea. Ask your doctor if you can take an anti-diarrheal drug, like bismuth subsalicylate or loperamide .
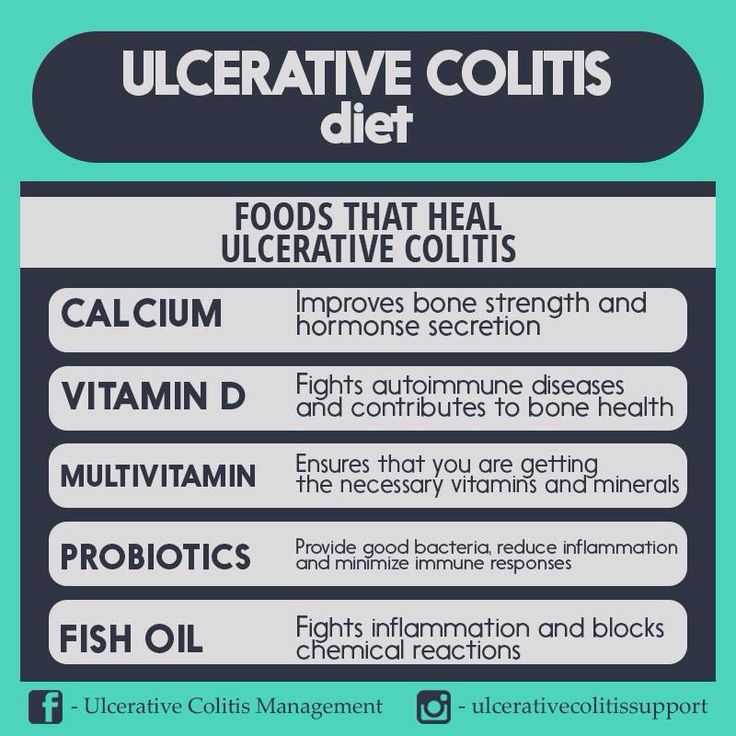
Canker sores. Medicated mouthwash may ease the irritation that these small mouth ulcers bring on. A balanced diet and a multivitamin or mineral supplement may help, too. Talk to your doctor before you try any new supplement.
You May Like: What Is A Duodenal Ulcer And How Is It Caused
Read Also: Vsl 3 For Ulcerative Colitis
Bottom Line On Uc Pain Relief
You may be battling UC pain today but that by no means predicts your future. Complete remission should be a shared goal between you and your doctor. It may take patience to find the best treatment but living your life without UC pain is an achievable goal.
Pain Prevalence:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Over the Counter Medications: Mayo Clinic. Ulcerative Colitis.
How Imodium Works: Imodium. How IMODIUM Products Work.
How Tylenol Works: Tylenol. What Is Acetaminophen?
NSAIDs: Therapeutic Advances in Gastroenterology. Pain Management in Patients With Inflammatory Bowel Disease: Insights for the Clinician.
Prescription Medications:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
How Do I Know If My Uc Has Gone Into Remission
UC doesn’t have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you don’t experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isn’t experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didn’t show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications aren’t working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
Read Also: Can Ulcerative Colitis Cause Fever
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
What To Eat With An Ulcerative Colitis Flare
While certain foods can be very well tolerated during good periods of the disease, these may then become an issue during an Ulcerative colitis flare-up.
Once the gut lining becomes inflamed and irritated this can lead to anything passing along it feeling very painful. This leads to the suggestions to reduce foods rich in fibre which can take a strain off the gut.
This involves key points such as:
- Removing stems and skins from fruits and vegetables
- Cooking and pureeing fruits as vegetables
- Slow cooking meats
- Avoiding nuts and seeds
Dairy has also been indicated to be an issue for many people with Ulcerative colitis and can potentially contribute to a flare. Removing dairy may calm the immune response and flare-up. A 2014 study concluded that the intake of dairy products may increase the severity of Ulcerative colitis.
Recommended Reading: What Does Ulcerative Colitis Affect
Meal Timing And Portion Sizes
For most people with IBD,eating small meals is easier on the digestive tract. For others, the simple act of eating can rev up the digestive system and make diarrhea worse. If your bowel movements subside when you take a break between meals, consider reworking your meal timing to include more substantial meals less often.
Since UC symptoms vary from person to person, theres no one-size-fits-all meal schedule. Pain can feel worse when youre not well-rested. Choose meals that are easy to tolerate when its close to bedtime, or finish eating for the day a few hours before going to sleep.
Keep Up With Your Medicine

Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Don’t Miss: Does Colectomy Cure Ulcerative Colitis
Can I Drink Alcohol With An Ulcerative Colitis Flare
Alcohol has a significant impact on the gut microbiome, leading to changes that can promote inflammation. While a small amount may be well tolerated, for some, alcohol even when consumed in small amounts, can lead to an increase in symptoms such as diarrhoea and pain.
The changes in the gut microbiome are noted in Ulcerative colitis patients who consume alcohol. Specifically, an increased number of bacteria that promote inflammation in the gut. This may then lead to increased permeability along the gut lining and the overactivation of the immune response which then leads to the tissue damage seen in this condition.
What Are Some Practical Steps To Take When A Flare
The first thing to do if a flare up occurs is to make sure you are eating a healthy diet which is low in fibre and contains plenty of water. Avoiding dairy products and cutting down carbohydrates may also help. The vast majority of people will requite adjustments to their medication, so you should seek medical advice from your GP or specialist.
Read Also: Does Turmeric Help Ulcerative Colitis
Recommended Reading: How To Apply Compression Bandages For Leg Ulcers
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
You May Like: Most Common Extraintestinal Manifestation Of Ulcerative Colitis
Have A Plan To Contact Your Doctor
If youre flaring, your gastroenterologist will want to knowso its important to keep in close contact. Have the conversation in advance, and ask your doctor, If I flare, who do I call and what do I do? says Neilanjan Nandi, M.D., an IBD gastroenterologist at Penn Medicine in Philadelphia. Be sure to write down any emergency contact numbersincluding for after-hours emergenciesand get familiar with your doctors online patient portal if they have one, he says. The sooner your doc is in the loop, the sooner you can get the treatment you need.
Recommended Reading: What To Avoid If You Have An Ulcer
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Prevent An Ulcerative Colitis Flare By Following A Diet That Works For You
To prevent flare-ups, I think that all the stress management techniques combined with DIET make a huge difference for me. My amazing GI has talked to me about a diet eliminating as much sugar and refined carbs as possible. I will definitely talk more in-depth about diet and a breakdown of my diet in the future, but here are some diet based tips to help you prevent an ulcerative colitis flare
You May Like: What Causes Ulcers To Flare Up
Read Also: Alginate Dressings For Treating Pressure Ulcers
Overview Of Ulcerative Colitis
UC is a chronic condition and one of the more common IBDs .
While UC can be managed, theres currently no cure. Its a complex condition broadly characterized by persistent inflammation of the lower intestine. Small ulcers develop due to the inflammation that cause significant pain and discomfort. Sometimes the pain is continuous, others its mild unless theres a flare-up.
Estimates are that between 600,00 and 900,000 in the US live with Ulcerative Colitis. Youre not born with UC. It normally develops between ages 15-30, but can appear at any point in life. Some peoples UC gradually develops, while others are hit with full force almost overnight.
UC can lead to complications pretty quick, some of which are fatal, so it cant be left untreated.
Recommendations For Cancer Surveillance
Patient with UC have an elevated risk of developing colon cancer. After 8-10 years of colitis, annual or biannual surveillance colonoscopy with multiple biopsies at regular intervals should be performed . Detection of high grade dysplasia in flat mucosa has to be confirmed by a second pathologist and is an indication for colectomy .
The sensitivity of random biopsies is a matter of debate and uncertainty as dysplasia in flat mucosa can be easily overlooked. Implementation of advanced endoscopic imaging techniques such as high-resolution white-light endoscopy, autofluorescence and narrow-band imaging may help to better identify pathological lesions and optimize cancer surveillance in inflammatory bowel disease in the future.
You May Like: Diabetic Leg Ulcers Home Treatment
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Work With Your Doctor
Youâll need to see your doctor regularly. It may be every 6 months while youâre in remission. Youâll have routine procedures like colonoscopies and bloodwork to check on your UC.
If youâre having a flare-up, make sure to check in with your doctor. UC isnât the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Canât keep liquids down
Recommended Reading: What Can Cause Ulcerative Colitis Flare Ups
Prediction Of Outcome And Surgical Therapy
In a recent population-based European study, the global risk of colectomy in UC was 8.7% over 10 years. Efforts have been made to identify patients who are at high risk of not responding adequately to pharmacological therapy. In Crohns disease, factors such as young age at first diagnosis, early steroid use, ileal disease, mucosal healing, and smoking were identified as important for developing disabling disease or for major abdominal surgery. Much less is known in UC. According to data from different population-based studies, including the recent 10-year data from the Norwegian IBSEN cohort, initial extensive colitis, elevated ESR and sclerosing cholangitis were associated with an increased risk of colectomy. In contrast, older age at disease onset and smoking reduced the risk of subsequent colectomy. In a prospective study evaluating 49 hospitalized patients with severe UC, patients treated with steroids and/or CsA, a stool frequency of > 8/d or 3-8 stools/d, and increased CRP on day 3 predicted the need for colectomy with 85% certainty. Further work to identify predictive parameters of refractory courses should help to prevent a delay in inevitable surgical therapy.
Emergency indications for surgery includes refractory toxic megacolon, perforation and continuous severe colorectal bleeding . In this situation the recommended operation is colectomy and ileostomy, leaving the rectum in situ, since reconstruction is not an option in the acute setting .