Referral To A Specialist
In some cases, your GP or nurse may decide to refer you to a specialist in conditions affecting the blood vessels .
For example, you may be referred to a vascular specialist if your GP or nurse is unsure about your diagnosis, or if they suspect your ulcer may be caused by artery diseases, diabetes or rheumatoid arthritis.
After taking your medical history and examining you, the vascular specialist may need to arrange further investigations to plan your treatment.
Treating An Infected Ulcer
An ulcer sometimes produces a large amount of discharge and becomes more painful. There may also be redness around the ulcer. These symptoms and feeling unwell are signs of infection.
If your ulcer becomes infected, it should be cleaned and dressed as usual. You should also elevate your leg most of the time. Youll be prescribed a 7-day course of antibiotics. The aim of antibiotic treatment is to clear the infection. But antibiotics do not heal ulcers and should only be used in short courses to treat infected ulcers.
When Should I See My Healthcare Provider
You should see a primary care provider at least once a year for a physical. This is key to the early detection of health problems, including those that can cause vascular ulcers.
You should also talk to your provider if you have any of the following:
- A wound on one of your legs or feet that is taking longer to heal.
- Symptoms that might mean you are having circulation problems in your legs, especially swelling, pain, color changes or pain that changes or goes away depending on how you hold your leg or foot.
- Pain in your legs that gets better when you rest.
Also Check: Good Foods To Eat With An Ulcer
What Are The Symptoms Of Chronic Venous Insufficiency
Symptoms of chronic venous insufficiency may include:
-
Swelling in your legs or ankles
-
Tight feeling in your calves or itchy, painful legs
-
Pain when walking that stops when you rest
-
Brown-colored skin, often near the ankles
-
Varicose veins
-
Leg ulcers that are sometimes hard to treat
-
Having an uncomfortable feeling in your legs and an urge to move your legs
-
Painful leg cramps or muscle spasms
The symptoms of chronic venous insufficiency may seem like other health conditions. Talk with your healthcare provider for a diagnosis.
Making Healthy Lifestyle Choices

Maintaining a healthy lifestyle has a direct impact on vein health. A nutritious diet, regular exercise, maintaining a healthy weight, and following the recommendations of your health care provider can slow the progression of vein disease, ensure the successful outcome of vein treatment, and promote healing.
Also Check: Where Does It Hurt When You Have An Ulcer
Understanding Venous Stasis Ulcers
Venous stasis ulcers are wounds caused by the accumulation of fluid that commonly accompanies vein disorders. As fluid leaking from dysfunctional veins accumulates into surrounding tissues, the flesh surrounding the area becomes irritated, inflamed, and begins to break down. Over time, the breakdown of tissues combined with the lack of oxygen and nutrients causes ulcers on the lower leg. The lack of circulation impairs healing. Left untreated, venous stasis ulcers can cause a significant number of health complications, including severe infections and necrosis.
Venous Insufficiency Stage 2
As the symptoms of venous insufficiency progress, the discomfort can be more pronounced. As a result of the breakdown of iron in the blood, skin can turn various shades of red and brown. The skin on the lower leg eventually starts to show outward signs of the internal dysfunction. Skin may appear thickened, hardened, scaly, or bumpy, a skin condition known as stasis dermatitis. As inadequate blood supply impairs the skins ability to regenerate, even mild trauma or scratching can injure traumatized skin. Those living with chronic venous insufficiency may also find their skin can appear thin, shiny, weepy, or crusty. Since venous insufficiency impairs the healing process, skin damage can easily become infected.
Also Check: How Do They Treat Stomach Ulcers
Caring For Venous Ulcers
Venous ulcers need proper care and treatment to prevent infection and to heal. It’s important to have any venous ulcers checked right away by your healthcare provider.
Treatment may require focusing on the circulatory or vein problems that are causing the ulcers. Or it may mean removing some tissue around the wound. You may be asked to:
-
Clean the wound regularly
-
Apply a dressing to the ulcer
-
Avoid products that cause skin sensitivity
-
Wear compression stockings to prevent blood from pooling in the legs and to speed healing
-
Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
-
Take oral antibiotic medicines to prevent or treat an infection
-
Have allergy testing done
Wearing a compression wrap to keep blood flowing back up to your heart can also help ulcers heal more quickly. In some cases, surgery or a skin graft is needed to close up the opening in the skin.
Tabular List Of Diseases And Injuries
The Tabular List of Diseases and Injuries is a list of ICD-10 codes, organized head to toe into chapters and sections with coding notes and guidance for inclusions, exclusions, descriptions and more. The following references are applicable to the code I87.2:
Inclusion Terms
Your vascular system is your bodys network of blood vessels. It includes your
- Arteries, which carry oxygen-rich blood from your heart to your tissues and organs
- Veins, which carry the blood and waste products back to your heart
- Capillaries, which are tiny blood vessels that connect your small arteries to your small veins. The walls of the capillaries are thin and leaky, to allow for an exchange of materials between your tissues and blood.
Vascular diseases are conditions which affect your vascular system. They are common and can be serious. Some types include
Italian sausage and a heap of Parmesan cheese lend signature flair to the easy Thanksgiving dressing
A classic dry martini cocktail made with gin and vermouth and stirred with ice.
Its all about the layers and ruffles in this dramatic seasonal pie.
As with hot chocolate, use any milky liquid you prefer, whether its from a cow, nuts ,
This is the dramatic seafood paella that looks stunning, with crustaceans and shellfish. You can vary
Alton Browns turkey brine recipe from Good Eats will give you a flavorful Thanksgiving turkey with juicy
Bone-in turkey breasts are easy to find, and as impressive as a whole bird when you roast them in butter
Don’t Miss: Foods To Avoid If You Have A Stomach Ulcer
What Is Venous Ulcer
A venous leg ulcer is a long-lasting sore that takes more than 4 to 6 weeks to heal. Venous leg ulcers usually develop on the inside of the leg, just above the ankle. A venous leg ulcer is the most common type of leg ulcer, accounting for more than 90% of all cases. Venous leg ulcers can develop after a minor injury, where persistently high pressure in the veins of the legs has damaged the skin. The symptoms of a venous leg ulcer include pain, itching and swelling in the affected leg. There may also be discolored or hardened skin around the ulcer, and the sore may produce a foul-smelling discharge.
Its estimated around 1 in 50 people over the age of 80 has one venous ulcer.
Venous ulcers are usually accompanied by other clinical signs of venous disease such as swelling, pigmentation, varicose dermatitis, atrophie blanche and lipodermatosclerosis. High blood pressure in the leg veins causes leakage of fluid from the abnormal veins into the surrounding tissues. This leads to swelling, especially around the ankles. Leakage of red blood cells leads to iron staining and skin pigmentation in the lower legs. The subsequent inflammation will result in varicose eczema and may lead to scarring and hardening of the skin and fat in affected areas. This will eventually lead to skin breakdown and ulceration.
Youre more at risk of developing venous ulcer if you previously had deep vein thrombosis or find it difficult to walk because of a problem such as:
- osteoarthritis
- obesity
- paralysis
Definition Rationale And Scope
Venous leg ulcers are defined as open lesions between the knee and ankle joint that occur in the presence of venous disease. They are the most common cause of leg ulcers, accounting for 60-80% of them. The prevalence of VLUs is between 0.18% and 1%. Over the age of 65, the prevalence increases to 4%. On an average 33-60% of these ulcers persist for more than 6 weeks and are therefore referred to as chronic VLUs. These ulcers represent the most advanced form of chronic venous disorders like varicose veins and lipodermatosclerosis.
Risk factors for development of VLUs include older age, female sex, obesity, trauma, immobility, congenital absence of veins, deep vein thrombosis , phlebitis, and factor V Leiden mutation.
Also Check: What’s Good For An Ulcer In Stomach
Risk Factors And Symptoms
The incidence of venous insufficiency rises with age, and is also linked to a family history of varicose veins, a sedentary lifestyle, or to jobs that require people to spend many hours on their feet. Venous insufficiency can also be caused by a partial blockage of the veins, for example by a blood clot .
The most common early symptom of venous insufficiency is chronically swollen ankles the feet and calves may also swell. The swelling can be accompanied by a dull aching, cramping, or feeling of heaviness in the legs and feet that becomes worse after prolonged standing.
As the condition progresses, people with venous insufficiency develop brown patches and deteriorating skin around the ankles. If venous insufficiency is not treated, venous ulcers may develop on the lower legs.
Doctors use an imaging test called a duplex ultrasound to determine if there is structural damage in the veins.
What Is Venous Stasis
Venous stasis is the swirling, slowing down or pooling of blood inside leg veins. This condition is also called venostasis. This pooling is a direct result of malfunctioning vein valves, sitting for too long or varicose veins. When malfunctioning vein valves are left untreated, and as it progresses, venous stasis can cause increasing pain and swelling in affected areas while also increasing the risk of blood clots and contributing to the formation of varicose veins, venous stasis ulcers, and stasis dermatitis.
Most often observed in the legs, this condition is more common in people with chronic venous insufficiency and people who travel often.
Read Also: Best Over The Counter Ulcer Medication
Venous Ulcer Diagnosis And Treatment
Doctors at Vascular surgeons at UPMC’s Heart and Vascular Institute use duplex ultrasound, a noninvasive test, to diagnose abnormal veins that cause venous ulcers. Part of the UPMC difference is that we actively look for the causes of the ulceration to treat venous pathology and keep the ulcer healed.
After an evaluation of your veins, we recommend a treatment plan based on your needs:
- Compression
- Compression of the leg is vital to healing venous wounds.
- Compression stockings are most commonly used for this treatment.
- The pressure from the compression dressing counteracts the pressure from the veins of the leg and allows skin to heal.
What Causes Chronic Venous Insufficiency
You are more likely to have this condition if you:
-
Are overweight
-
Have a family history of the problem
-
Had damage to your leg due to injury, surgery, or previous blood clots
Other causes of chronic venous insufficiency include:
-
High blood pressure in the leg veins over time, due to sitting or standing for long periods
-
Lack of exercise
-
Smoking
-
A blood clot in a deep vein, often in the calf or thigh
-
Swelling and inflammation of a vein close to the skin, often in the legs
Also Check: Home Remedies For Oral Ulcers
Recognizing The Signs Symptoms And Stages Of The Disease
As a complication of venous insufficiency, venous stasis ulcers affect an estimated 25 percent of our population. The signs and symptoms of venous insufficiency are commonly classified into three distinct phases. The phases of the disorder progress over time, particularly if this chronic health condition is left untreated or poorly managed. The three stages of venous insufficiency are identified by the following symptoms:
Venous Stasis Ulcer Diagnosis
Venous stasis ulcer diagnosis is largely based on your symptoms and examination of your affected leg, although additional tests may be required.
Venous stasis dermatitis can also be related to heart problems or other conditions that cause leg swelling. Your provider may need to check your general health and order more tests.
Medical history and examination
Your doctor or practice nurse will ask whether you have any other symptoms associated with venous leg ulcers, such as:
- swelling in your ankles
- discolored or hard skin
Your doctor will try to determine the cause of the ulcer by asking about underlying conditions or previous injuries, such as:
- diabetes
- injury or surgery in the affected leg
- a previous leg ulcer
Your doctor will also examine your leg, both when youre standing up and lying down.
Varicose veins will be more obvious when youre standing up, and itll be easier to look at the ulcer when youre lying down.
Your doctor will also feel your pulse at your ankles to make sure the arteries in your leg are working properly.
Recommended Reading: What Makes Stomach Ulcers Feel Better
How Are Stasis Ulcers Diagnosed
Stasis ulceration is usually a clinical diagnosis, made on the basis of the patient’s history and examination findings, and includes the presence of risk factors for venous stasis, that is, congestion and slowing of venous circulation, and the characteristic features of the wound and surrounding tissues.
- Duplex ultrasonography is used to confirm venous obstruction or valvular incompetence prior to saphenous vein ablation surgery
- Concomitant arterial disease is identified using the ankle-brachial index
Other investigations to evaluate venous insufficiency and provide haemodynamic information may include:
- Intravenous ultrasonography
- Ascending or descending venography/phlebography
- Venous air plethysmography
- Haematological studies of the coagulation system.
How Can I Reduce My Risk Of Developing A Vascular Ulcer
There are some things you can do to reduce your risk of developing a vascular ulcer. They can also help improve ulcers you already have.
- Maintain a healthy weight. Obesity is strongly tied to the formation of vascular ulcers and health problems that may also cause ulcers.
- Manage your health issues. This includes high cholesterol, high blood pressure, diabetes and more.
- Get a regular checkup. Many of the issues that can cause a vascular ulcer can be caught during a routine physical, even if they aren’t causing symptoms yet. Knowing about a health concern early can help you avoid developing an ulcer.
- Quit tobacco. The use of tobacco and nicotine products is closely tied to an increased risk of several conditions including high blood pressure and heart disease that can cause a vascular ulcer.
- Don’t delay care. If you develop a wound that is taking longer to heal than expected, see your doctor as soon as possible. They can examine the wound and help you resolve it before it gets even worse.
Also Check: What Does And Ulcer Feel Like
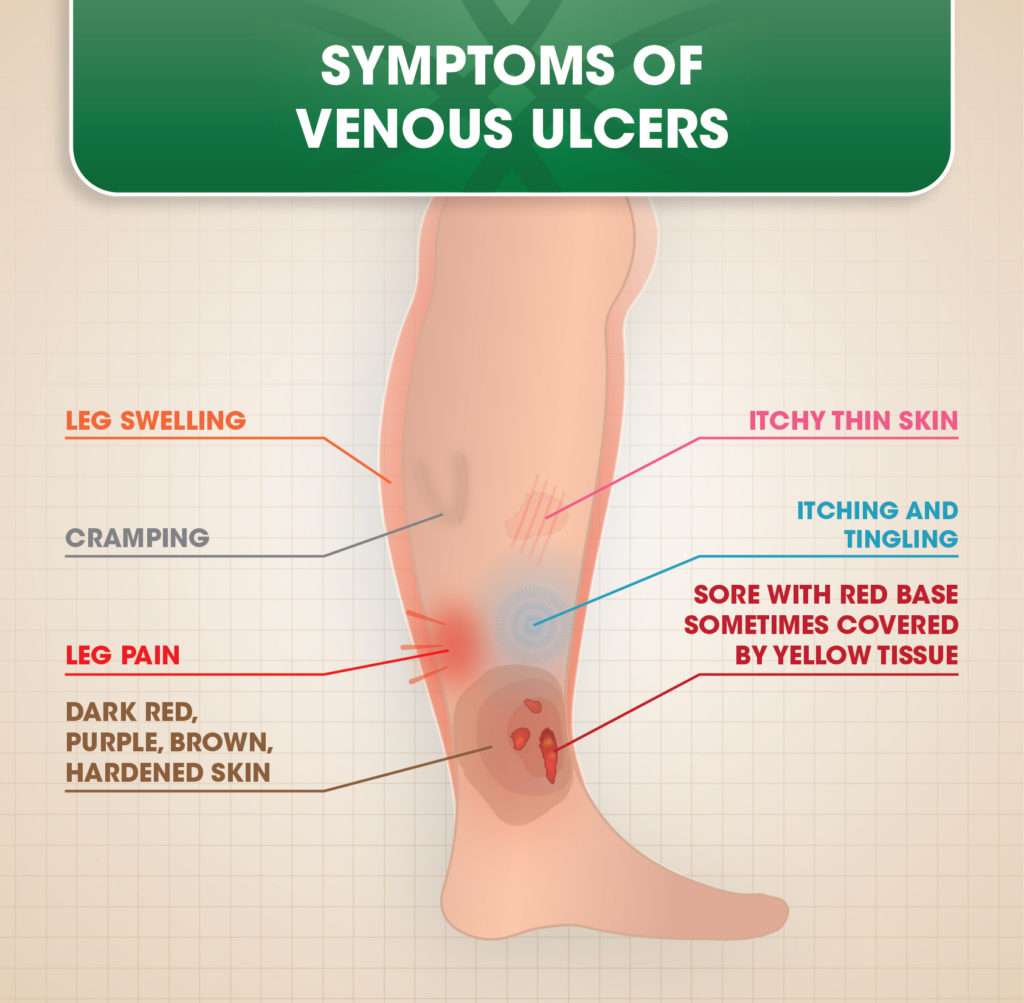
Venous Stasis Ulcer Signs And Symptoms
Venous stasis ulcer signs and symptoms include:
- Shallow sore with a red base, sometimes covered by yellow tissue
- Unevenly shaped borders
- Surrounding skin may be shiny, tight, warm or hot, and discolored
- Leg pain
- If the sore becomes infected, it may have a bad odor and pus may drain from the wound
You may have symptoms of venous insufficiency including:
- Dull aching or heaviness in the leg
- Pain that gets worse when you stand
- Swelling in the leg
At first, the skin of the ankles and lower legs may look thin or tissue-like. You may slowly get brown stains on the skin.
The skin may become irritated or crack if you scratch it. It may also become red or swollen, crusted, or weepy.
Over time, some skin changes become permanent:
- Thickening and hardening of the skin on the legs and ankles
- A bumpy or cobblestone appearance of the skin
- Skin turns dark brown
Skin sores may develop . These most often form on the inside of the ankle.
Medical History And Examination

Your GP or practice nurse will ask whether you have any other symptoms associated with venous leg ulcers, such as:
- swelling in your ankles
- discoloured or hard skin
They’ll try to determine the cause of the ulcer by asking about underlying conditions or previous injuries, such as:
Read more about how venous leg ulcers are treated.
Also Check: Natural Supplements For Ulcerative Colitis
What Causes A Venous Ulcer
Vein disease is the root cause of a venous ulcer. Vein disease develops when the one-way valves inside of a vein stop functioning correctly. The one-way valves are designed to push blood toward the heart however, sometimes the valves weaken and are unable to adequately return the blood to the heart. As a result, excess blood remains in the vein, which creates increased pressure on the vein wall. Further, the excess blood has nowhere to go, so it pools in the lower extremities. The pooled blood may seep out of the vein and into surrounding tissue, causing the skin to become discolored and tender. If left untreated, the excess blood and pressure can break down the skin from the inside out and create open, painful sores on the surface of the skin. Once a venous ulcer has developed, it can be challenging to treat and can take weeks, months or even years to heal.