Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
When Is Blood In The Stool A Cause For Concern
Although bleeding with UC is common, losing too much blood can have severe negative effects on the body. Its essential to recognize the warning signs of significant blood loss and seek help if you start to exhibit these symptoms.
Everyone with UC experiences this symptom differently. When present, bright red blood is often seen on the surface of the stool. However, it may also appear in the toilet bowl, turning the water red.
The amount of bleeding a person with UC experiences also depends on the severity of their condition. Those with mild to moderate UC may only see occasional blood in their stool, while those with severe or active UC may see blood frequently in their bowel movements. In extreme cases, some people may have more than 10 bloody bowel movements a day.
Seek immediate medical care if you experience any of the following while having bloody stools with UC:
- Infrequent or low urination
- Pale, cold, or clammy skin
- Lightheadedness or dizziness upon standing
- Severe abdominal cramping
- Heavy and continuous rectal bleeding
Its important to carefully monitor how much blood is normal for you to expect during a flare-up in order to understand what is out of the ordinary. If you do not have these symptoms but notice bleeding from your rectum for more than one or two days, are bleeding more heavily than normal, or are experiencing unusual flare-ups, contact a health care professional.
How Ulcerative Colitis Causes Nausea
Depending on the circumstances, nausea can be a , confrms Loretta Randolph, R.N., a clinical research nurse in digestive diseases at the University of Cincinnati in Cincinnati, OH. Although nausea can strike at any time, patients are most likely to experience it during a , she adds.
On the other hand, itself may also be to blame, says Randolph, since nausea can be a side effect of some oral UC medications.
Disease severity and the location of your ulcerative colitis can also influence symptoms. According to the National Institute of Diabetes and Digestive and Kidney Diseases, nausea and vomiting are more likely to occur if your or affects more of your large intestine.
Don’t Miss: How To Treat And Ulcer
People Describe How They Were Diagnosed With Ulcerative Colitis
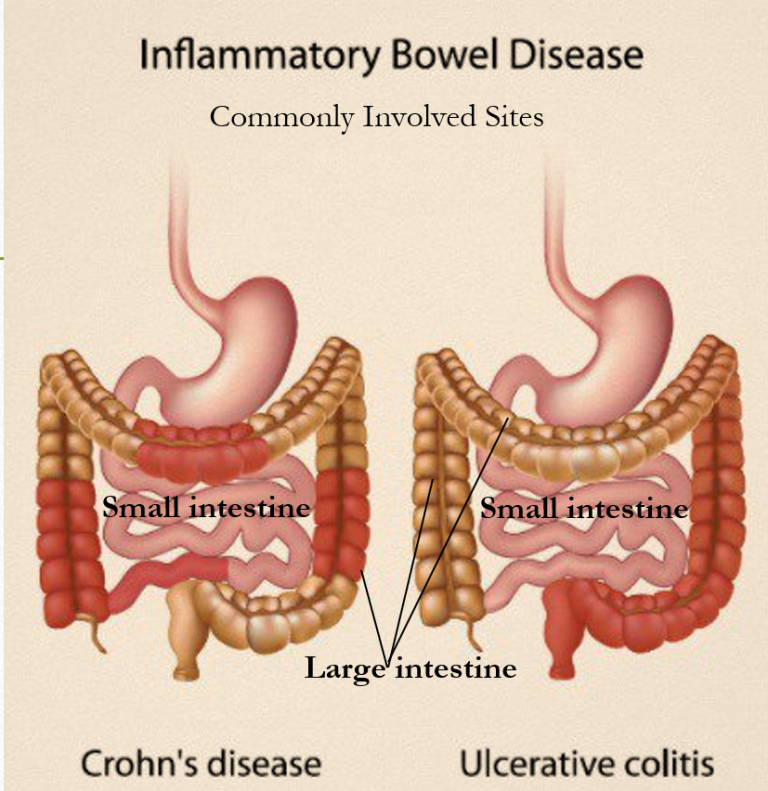
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohn’s disease .
UC is a chronic conditionthat can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while there’s no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesn’t cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Related:
When To Call A Professional
New or changing symptoms often mean that additional treatment is needed. People who have ulcerative colitis should be in frequent contact with their physicians.
Common symptoms that require a doctor’s immediate attention are:
- Fever, which could indicate infection or a ruptured intestine
- Heavy bleeding from the rectum
A serious, but uncommon, complication is called toxic megacolon. This results when the colon inflammation is so severe that it stops the colon’s motion. Megacolon causes the abdomen to swell. This can cause vomiting or severe abdominal pain and bloating. Megacolon requires emergency treatment, often surgery.
Also Check: How To Calm Ulcer Attack
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
What Are The Risk Factors Of Ulcerative Colitis
The cause of ulcerative colitis is unclear, but its thought that a combination of genetics and environmental factors are at play. Up to 20 percent of people with ulcerative colitis have a parent, sibling or child with the disease.
Ulcerative colitis is more common for people living in urban, industrialized areas compared to undeveloped countries, which indicates that highly refined diets may play a role. Although all ethnic groups are affected, the problem is most common among Caucasians and people of Eastern European Jewish descent.
Lastly, there appears to be a connection to nonsteroidal anti-inflammatory medications. Its not that these medications cause the disease but, because they inflame the bowel, they can worsen symptoms. This category of medication includes ibuprofen , naproxen sodium and diclofenac sodium .
Don’t Miss: Generic Drugs For Ulcerative Colitis
Taking Care Of Your Hair
For some people, simple dermatologist-recommended practices to increase scalp and follicle health may do the trick. These practices include:
- Limiting the use of heated styling tools, such as curling irons and hair straighteners
- Blow-drying infrequently or on low heat
- Avoiding chemical treatments, such as coloring and relaxing
- Using gentle or naturally derived hair products
- Avoiding hairstyles that tug on the hair follicles, such as tight ponytails
- Being gentle when combing or styling your hair
Recommended Reading: Holistic Treatment For Ulcerative Colitis
Managing Vomiting With Ibd
People living with IBD may experience vomiting for the same reasons they have nausea. For adults with IBD, vomiting greenish-yellow fluid called bile can be normal or a sign of an obstruction of the intestines.
While managing vomiting at home, avoid eating solid food and anything besides clear liquids until the vomiting episode is over. Be aware of the symptoms of dehydration like confusion, dark yellow urine, and excessive thirst.
People living with IBD should consider contacting their health care providers about vomiting sooner than those without the condition because of the risk of serious complications such as bowel obstruction with Crohns disease. Adults should seek medical attention after one to two days of vomiting or if they have any of the following symptoms with the vomiting:
- Blood in your stool or vomit
- Fever over 101 degrees Fahrenheit
- Severe cramping or belly pain
- Severe headache
If youre caring for a child with IBD who is vomiting, bring them to medical professionals quicker than if they were an adult, as they are at higher risk for complications like dehydration.
You May Like: How To Use Aloe Vera Gel For Ulcerative Colitis
Symptom No : Abdominal Cramps
Solution: Try to pinpoint your triggers. Stomach cramps are often caused by gas or spasms in the gut. Common culprits include foods high in fiber or fat, which can impact gas production, says , an assistant professor of medicine at the University of Minnesota Medical School in Minneapolis and director of their inflammatory bowel disease program. Foods that are high in insoluble fiber especially cruciferous vegetables, such as broccoli and cauliflower can be particularly hard to digest, according to the Crohns & Colitis Foundation.
Medications, such as a recent course of antibiotics or nonsteroidal anti-inflammatory medications ibuprofen, naproxen, aspirin can also trigger abdominal pain, he says.
What Causes Nausea In Ibd
Nausea, like all symptoms of IBD, is believed to result from a faulty immune response. In autoimmune disorders like IBD, the immune system mistakenly attacks the bodys healthy tissues in this case, the gastrointestinal tract. This attack results in inflammation that ultimately causes the symptoms of UC and Crohns disease.
Although nausea can be present at any time, it usually indicates that a person diagnosed with IBD is experiencing a flare-up. Other factors may also contribute to nausea in those with Crohns disease and UC, including bowel obstruction in Crohns disease and medications for IBD.
Recommended Reading: Best Over The Counter Medicine For Ulcer Pain
Strategies For Handling Nausea After Eating
Even though I have a J-pouch, my nausea is often extremely debilitating, making it hard for me to function at work or when Im out with friends. Ive consulted with a dietitian who specializes in ulcerative colitis, and shes helped me really understand what foods to avoid and why.
Ive also figured out a few other coping strategies:
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
You May Like: What Causes Stomach Ulcers In Horses
Symptom No : Sudden Diarrhea
Solution: In a pinch, use an over-the-counter antidiarrheal medication,such as those containing imodium. To reduce diarrhea over the long term, try eating more gut-soothing foods rice, bananas, toast and avoiding some of the tougher-to-digest fruit and vegetable skins, Vaughn says.
If youre in public, make sure you know the locations of nearby bathrooms. The Crohns & Colitis Foundation recommends drawing up a map ahead of time and packing a personal hygiene kit that includes toilet paper, wipes, ointment, and extra underwear or clothes.
Symptoms Beyond The Intestine
When ulcerative colitis is raging, it can take its toll on more than just the GI tract.
The inflammation from ulcerative colitis can make patients feel very fatigued lead to blood loss, causing anemia and cause weight loss due to difficulty absorbing nutrients, says Dr. Ather.
Symptoms beyond the intestine affect mental health and quality of sleep, too. A study published in 2018 in the International Journal of Behavioral Medicine found higher rates of mental health and sleep disorders in people with ulcerative colitis.
It is important for us to screen for these issues and refer our patients to get the help they need, Dr. Ather says.
You May Like: How Do You Get Ulcerative Colitis
Don’t Miss: Can Ulcers Cause Heart Palpitations
When To Contact A Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
There is no known prevention for this condition.
What Is Ulcerative Colitis
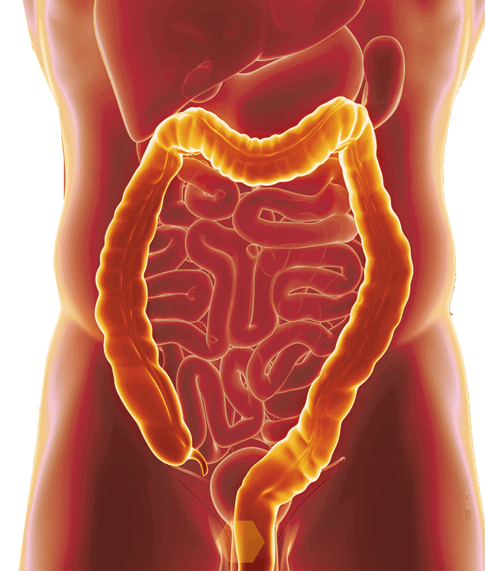
Ulcerative colitis is an inflammatory disease. It usually begins in the rectum, then worsens to involve some or all of the large intestine. Ulcerative colitis is a lifelong condition.
Ulcerative colitis may begin with a breakdown in the lining of the intestine. The inside of the intestine, with its digested food, contains trillions of bacteria. Normally, the lining of the intestines keeps these bacteria from causing an infection of the wall of the intestine.
As long as the bacteria are contained, they remain invisible to your immune cells. They do not provoke a reaction. But when the intestine’s lining fails, bacteria that usually are harmless can activate your immune system.
Ulcerative colitis is an autoimmune disease. This means that the immune system, which is supposed to attack foreign things that get inside our bodies, instead attacks a part of the body.
In ulcerative colitis, the bowel bacteria provoke the immune system to attack the wall of the intestine itself, injuring the bowel.
There also is evidence that unusually large or small numbers of certain types of bacteria that normally live in everyone’s gut can make the gut vulnerable to ulcerative colitis.
Once the bowel inflammation has started, it can continue. It continues even if the immune system stops being exposed to the bowel bacteria.
Ulcerative colitis affects the inner lining of the rectum and colon. This causes the lining to:
- Wear away in spots
- Ooze cloudy mucus or pus
Also Check: Living With Ulcerative Colitis Stories
What Tests Diagnose A Peptic Ulcer
To confirm a person has an ulcer a diagnostic imaging test will usually be ordered. The two most widely used tests are:
- Upper GI series : This is a type of X-ray. The patient is given a chalky liquid to drink that increases the contrast on the X-ray, making certain features easier to see. Because this liquid contains barium, this test is sometimes called a barium swallow.
- Endoscopy : An endoscope is a thin, flexible tube with a tiny camera at the end. The patient is given a mild sedative, and then the tube is passed through the mouth into the stomach. The doctor can see the lining of the stomach to diagnose a peptic ulcer. Tiny samples of the tissue will be taken , which are examined under a microscope.
If a diagnostic imaging test reveals an ulcer, the patient will most likely have a test to see if H pylori bacteria are present.
- It is important to be certain about this, because treatment of the H pylori is likely to heal the ulcer.
- Ulcers caused by H pylori are treated differently than ulcers caused by medications.
Three types of tests are available to detect H pylori.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Recommended Reading: Ulcerative Colitis And Night Sweats
Managing Daily Life After Surgery
Flatulence is a common problem following surgery. People may need to avoid insoluble fiber foods, such as popcorn, olives, and vegetable skins, which can obstruct the stoma. Some pouching systems have filters that can help limit flatulence.
It is important to increase fluid intake, and include not only water but also broth, sports drinks, and vegetable juice to maintain appropriate levels of sodium and potassium.
Ileostomy and ileoanal anastomosis do not interfere with bathing or showering or most physical activity except for contact sports. As a rule, the surgeries do not impair sexual function.