Will Ulcerative Colitis Affect Me Over Time
The effects of ulcerative colitis vary considerably from person to person, based on the nature and severity of their disease. In many cases, the condition does not have much impact on daily life, the ability to work or to enjoy an active social life but does take some getting used to. When it is at an active stage, symptoms such as diarrhoea and abdominal pain often require time away from work, college etc. and can make it difficult to cope going out or even being at home. However, treatment usually makes the symptoms better within days or weeks so normal quality of life can be restored quite quickly. Some severe cases of ulcerative colitis, however, can have a significant impact on peoples lives. This can be due to a weak response to treatment which makes symptom-free remission difficult to achieve and can involve frequent flare ups.
Available Topical Therapies For Distal Colitis
Common therapies for the treatment of UP and UPS include 5-aminosalicylic acid and steroids. Mesalamine and other 5-ASA substances are the first-line choice in treating mild-to-moderate UC, regardless of the physical extent of disease. Mesalamine has multiple reported anti-inflammatory effects that include inhibiting leukotriene and IL-1 production, impairing TNF and NF-B transcription signaling and having antioxidant properties by acting as a free-radical scavenger. Additionally, mesalamine reduces mucosal inflammation by acting on mucosal colonic epithelial cells and infiltrating leukocytes, with its clinical efficacy therefore correlating with its local concentration in the gut.
Practice guidelines recommend using topical mesalamine agents as first line compared to topical steroids or oral aminosalicylates for the treatment of distal mild-to-moderate UC, and the combination of oral and topical aminosalicylates is more effective than either alone. In addition, practice guidelines recommend mesalamine suppositories or enemas as the preferred agents to maintain remission in distal mild-to-moderate UC. Mesalamine suppositories maintain remission in 90% of patients with mild-to-moderate UP at 1 year, while mesalamine enemas maintain remission in 72% of patients with mild-to-moderate UPS when administered every other day at 1 year.,
How To Define Ulcerative Colitis Pain
To help your doctor figure out whats causing your abdominal pain and other symptoms, you need to be able to accurately describe the sensation. Before seeing your doctor, take stock of what youre feeling. It may be useful to keep a colitis symptom journal to write down what you are experiencing. Be ready to describe:
- How long youve had your pain
- Where you feel your pain
- How it feels, both in sensation and intensity
- The frequency and duration of your pain
- What seems to trigger your abdominal pain
- What seems to help ease the pain
- What time each pain occurred, including how long after eating, and how long it lasted
The more specific you can be about your pain, the better, Dr. Kane says.
Read Also: Does Ulcer Pain Come And Go
Ways To Ease Ulcerative Colitis Pain
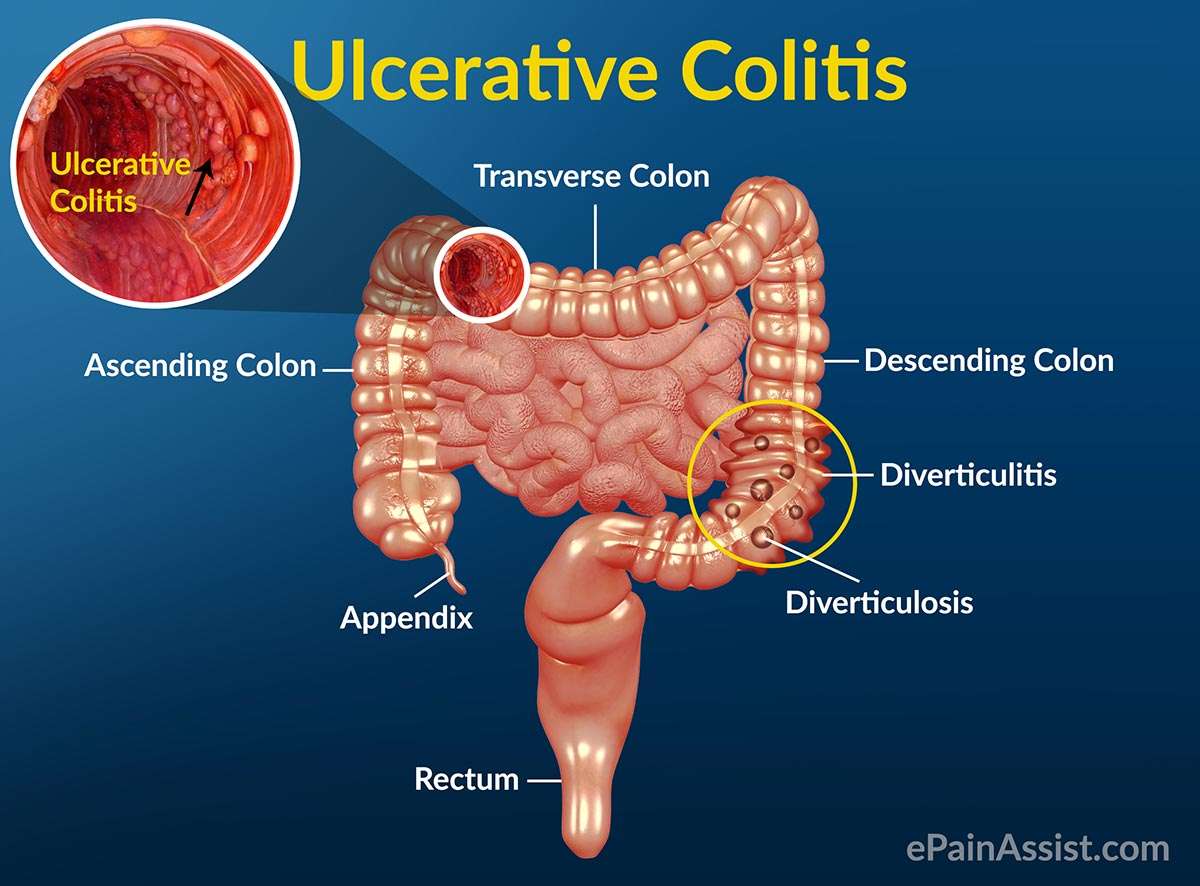
Ulcerative colitis is one of the chronic pain conditions that make up the category of inflammatory bowel diseases . It affects the digestive tract, but specifically is defined as causing inflammation and ulcers in the lining of the large intestines and the rectum. According to the CDC, over one million people suffer from some kind of IDB. This condition can be painful, debilitating, and wreak havoc on your everyday life. However, there are ways to help control ulcerative colitis pain and minimize the risk of flare-ups.
Can Lifestyle Changes Help Relieve Ulcerative Proctitis Symptoms
Remember, ulcerative proctitis is an autoimmune disease, meaning you didnt do anything to cause it. Even in remission, theres a risk of disturbing the very fine balance within the colon that can tip a flare-up, Dr. Lerrigo says. Its not the patients fault.
However, he says there are a few things you can do to try and support a healthier GI tract.
The perfect diet doesnt exist because each person has unique nutrition needs, explains Dr. Lerrigo. Thats why most of his patients work with a registered dietitian. However, experts do know that a diet that closely mimics the Mediterranean diet, one that is focused on fiber-rich whole grains, leafy vegetables, nuts, legumes, lean proteins like chicken and fish, and some dairy if you tolerate it, promotes a healthy gut ecosystem2 and reduces the risk of ulcerative proctitis flares, Dr. Lerrigo says.
He also recommends getting plenty of exercise and doing your best to manage stress, both of which can impact the immune system.
Don’t Miss: Ulcerative Colitis Flare Up Treatment Guidelines
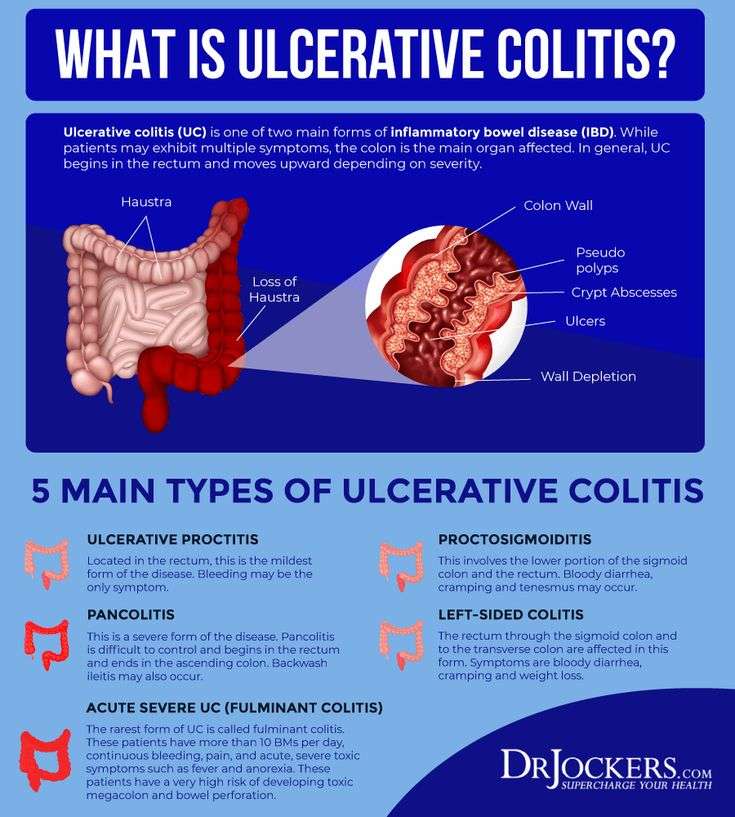
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Be Diligent And Careful With Medication
A physician will usually prescribe an anti-inflammatory and medication to help with an overactive immune system with a diagnosis of ulcerative colitis. This medication is vital to fight off flare-ups and missing a dose can be a trigger all by itself.
When taking medication for this condition, it is always wise to consult a doctor. Certain over-the-counter medications, like NSAIDs, can exacerbate ulcerative colitis as well as cause other issues.
Read Also: How Do You Treat A Peptic Ulcer
When To See A Doctor
Bleeding from the rectum or blood in or on the stool is never normal. It should always be brought up to a doctor. However, its not always an urgent situation.
If the cause of the bleeding is from a chronic condition , it should be discussed with your gastroenterologist.
In the case of new bleeding, see a doctor as soon as possible. Rectal bleeding that wont stop is a reason to go to the emergency department. Additionally, if you feel faint from blood loss, get to the emergency department right away or call an ambulance.
Abdominal pain can come and go with ongoing conditions, like Crohns disease or ulcerative colitis. Its important to discuss pain at doctors visits. However, if abdominal pain comes on suddenly and is severe, you should go to the emergency room or see a doctor right away.
In infants, caregivers will want to take the baby to see a pediatrician as soon as possible after seeing blood in the stool or around the rectum. Allergic colitis may be a common reason for bleeding, but its important to have a doctor check it out to make sure theres not a more serious reason.
Diet And Nutrition Modifications
Although food specifically doesnt cause ulcerative colitis, your diet can play a role in triggering or easing your symptoms. You may find that adopting a diet low in certain sugars or fiber particularly insoluble fiber, which passes through the GI tract undigested or free of lactose or gluten helps you manage your inflammatory bowel disease . Caffeine and carbonated beverages might also worsen your symptoms, as could spicy dishes.
Finally, if ulcerative colitis interferes with your bodys ability to absorb nutrients, ask your doctor whether you should take a vitamin supplement.
You May Like: How Do They Check For Ulcers
If Your Doctor Has Recommended Infusion Therapy Let Infusion Associates Help You
At Infusion Associates, we provide medically-prescribed infusion therapy for patients with chronic conditions in a welcoming and friendly environment. Our team of healthcare professionals is fully committed to making the experience as comfortable as possible for you or your patients. We always inform patients of any potential side effects and answer all their questions before starting treatment. In addition, we have a Registered Pharmacist on-site to make the process as seamless as possible.
If you would like to refer a patient to us or want to inquire about the treatments we offer, you can contact us by calling us at or filling out this form.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
You May Like: Can You Eat Pizza With Ulcerative Colitis
How Is Ulcerative Proctitis Treated
Ulcerative proctitis is usually very responsive to treatment, says Dr. Yoon. Your doctor will likely start by prescribing topical therapy, which means youll either use a suppository or an enema with an anti-inflammatory medication called mesalamine.
Dr. Yoon explains that the recommendation is to either use it every single night or at least two or three times a week just to keep the inflammation from coming back. If it works, you should ideally continue using it every night moving forward.
But in a practical sense, most people dont want to do that. People with ulcerative proctitis are usually young, in their 20s, so getting them to use a suppository for the rest of their life is wishful thinking, Dr. Yoon says. I have patients do it for four weeks and if theyre feeling fine and symptoms are mild, they can go ahead and stop. In the future, if they start bleeding again, they can do it for another four weeks.
Treatment for ulcerative proctitis can also include corticosteroids, such as prednisone or budesonide, which help reduce inflammation. Treating ulcerative colitis in general can involve immune system suppressors, like the pill azathioprine, and biologics, which are antibodies given via IV infusion or an injection that stop certain proteins from causing inflammation, according to the Crohns & Colitis Foundation.
Signs And Symptoms Of Proctosigmoiditis
Beyond the symptoms listed above, proctosigmoiditis also makes it difficult for you to have bowel movements even if you feel like you have to. Your symptoms will vary depending on how severe your inflammation is in your colon and rectum.
Ulcerative colitis is the overall term for this condition. It’s a type of IBD that causes many gastrointestinal problems. You might experience these symptoms, or you could have more localized symptoms with proctosigmoiditis. Common signs and symptoms of ulcerative colitis, in general, include:
- Weight loss
- Rectal bleeding â passing a small amount of blood with stool
- Urgent need to have a bowel movement
- Inability to have a bowel movement despite needing to â
Proctosigmoiditis is a milder type of ulcerative colitis. Depending on how much of your colon and rectum is affected, the symptoms can be less severe. However, the flare-ups can cause a lot of pain and can affect your health-related quality of life.
Don’t Miss: Diabetic Foot Ulcer Treatment Guidelines
Health Factors That Affect Proctosigmoiditis
If you have been diagnosed with ulcerative proctosigmoiditis, you may wonder what caused it. Some people believe food or stress causes it, which is a common misconception. While certain foods can upset your gastrointestinal tract, like stress, they are not the cause. Thereâs not a specific cause of ulcerative colitis, but there are factors that put you at risk. â
Heredity. Youâre more likely to get ulcerative colitis if your family has it too. Though in some cases, you might be the first in your family, you’re at higher risk if your parents or siblings have it. â
Age. Youâll typically be diagnosed with ulcerative colitis before 30. But you can get it later in life. This condition can affect anyone, regardless of age. â
Race or ethnicity. People who are white have a higher risk of getting ulcerative colitis. However, you have an even higher risk if youâre of Ashkenazi Jewish descent. â
Immune system malfunction. Another potential cause of proctosigmoiditis is when your immune system attempts to fight off a virus or bacteria but attacks your digestive cells too. Instead of fighting off the disease, your immune system goes after your digestive tract.
Infusion Therapy Treatment For Ulcerative Colitis
Your colon plays a vital role in everyday life. So, when a condition like inflammatory bowel disease causes ulcers to occur in your digestive tract, you tend to notice. Such is the case for people with Ulcerative Colitis . It impacts the innermost lining of the large intestine and rectum causing major discomfort. What can you do to treat UC? And, is infusion therapy a viable treatment?
Also Check: What To Do When You Have A Stomach Ulcer
Efficacy Of Budesonide Rectal Foam
Budesonide, a high-potency, nonhalogenated, second-generation corticosteroid, can be used either topically or orally in patients with UC. The pharmacokinetic profile of budesonide rectal foam, specifically the extent of spread and length of persistence in the colon, make it an efficacious topical treatment. Using -labeled budesonide foam in patients with moderate proctosigmoiditis or left-sided colitis, Brunner et al determined that budesonide spread 25.4±10.3 cm, reached the sigmoid colon in all patients, and had a mean colonic residence time of 5.3 hours. Sandborn et al compared rectal budesonide foam to placebo in two randomized, double-blind, side-by-side trials utilizing 546 patients with mild-to-moderate UP or UPS. All patients had disease extending at least 5 cm, but no > 40 cm from the anal verge. The budesonide treatment arm received 2 mg/mL two times daily dosing of the foam for 2 weeks and then was switched to once daily dosing for 4 weeks. The primary end point was remission, defined by Mayo Score 1, no rectal bleeding, and either no change or an improvement in stool frequency. A combined 41.2% of patients demonstrated remission as compared to 24% of the placebo patients . Interestingly, in subgroup analysis, budesonide rectal foam was still superior to placebo regardless of concurrent use of < 4.8 g/d of oral mesalamine, suggesting that budesonide foam can have additive treatment effects in patients already receiving oral mesalamine treatment.
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
You May Like: What Are Infusions For Ulcerative Colitis
Does Ulcerative Proctitis Always Progress To Ulcerative Colitis
Getting treated for ulcerative proctitis can ease symptoms and even lead to remission, meaning you may not experience symptoms for a certain period of time, but thats not quite the same thing as a cure.
Progression of the disease can happen, but its not super common, although being younger at the time of your diagnosis tends to be a risk factor for more severe disease throughout life, adds Dr. Lerrigo.
Less than 15% of people with ulcerative proctitis go on to develop full-blown ulcerative colitis, according to the National Organization for Rare Disorders . A majority of the time, people with ulcerative proctitis just have ulcerative proctitis. It doesnt necessarily progress to other areas of the colon, Dr. Yoon says. In most people with IBD, wherever the disease is located, it usually stays in that area.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Read Also: How Do I Know If I Have A Peptic Ulcer
Getting The Most From Your Treatment
- Try to keep your regular appointments with your doctor. This is so your doctor can check on your progress.
- Prednisolone can suppress your immune system, so it is important if you become ill that you make an appointment to see your doctor straightaway. If you come into contact with anyone who has measles, shingles or chickenpox , you should contact your doctor for advice as soon as possible.
- If you are having an operation or dental treatment, tell the person carrying out the treatment that you are using a rectal steroid preparation. It is also important that, if you are due to have any vaccinations, you make sure that the person treating you knows that you are using prednisolone. Some vaccines are not suitable for you while you are being treated with prednisolone.
- If you buy any medicines, check with your pharmacist that they are suitable for you to take with prednisolone.