Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
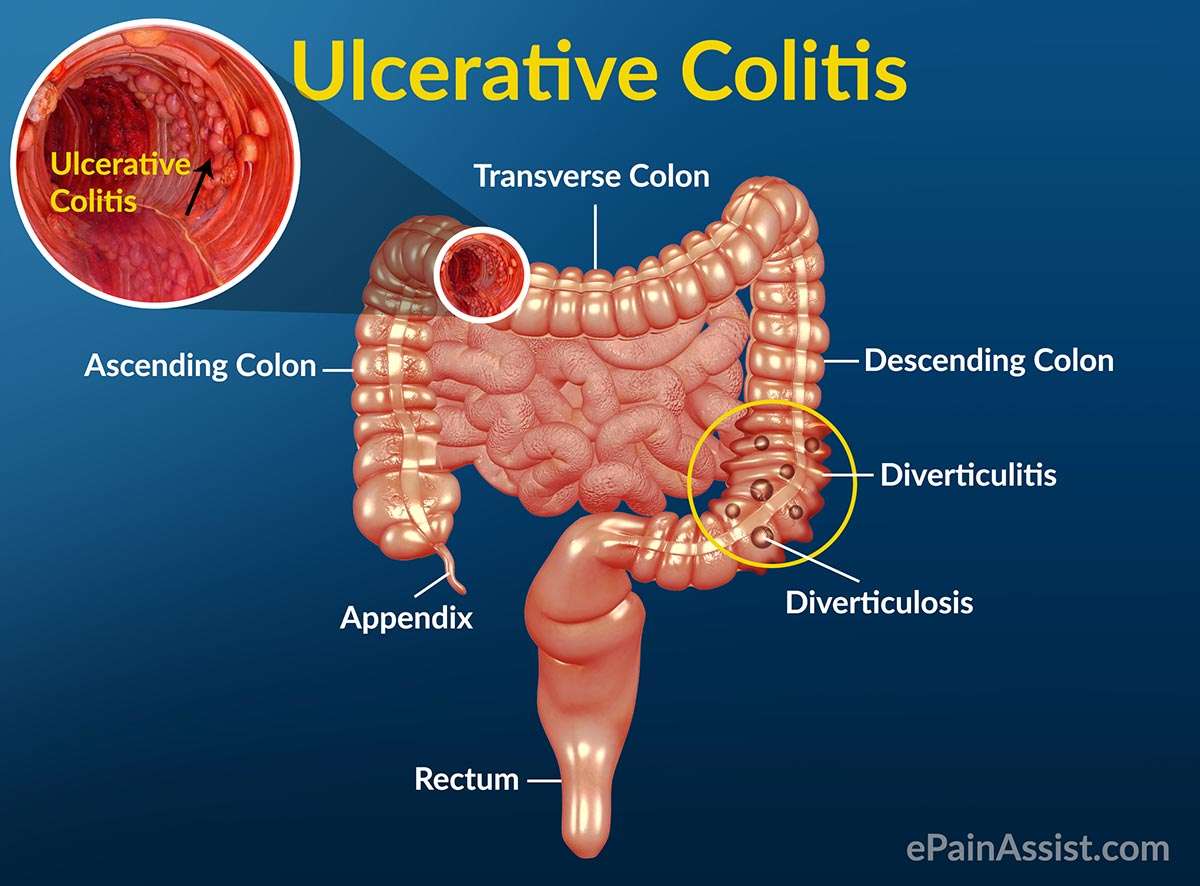
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
How Do Doctors Treat Symptoms And Complications Of Ulcerative Colitis
Doctors may recommend or prescribe other treatments for symptoms or complications of ulcerative colitis. Talk with your doctor before taking any over-the-counter medicines.
To treat mild pain, doctors may recommend acetaminophen instead of nonsteroidal anti-inflammatory drugs . People with ulcerative colitis should avoid taking NSAIDs for pain because these medicines can make symptoms worse.
To prevent or slow loss of bone mass and osteoporosis, doctors may recommend calcium and vitamin D supplements or medicines, if needed. For safety reasons, talk with your doctor before using dietary supplements or any other complementary or alternative medicines or practices.
Doctors most often treat severe complications in a hospital. Doctors may give
- antibiotics, if severe ulcerative colitis or complications lead to infection
Also Check: Ulcerative Colitis And Stomach Pain
More Drugs That Work On Your Immune System
Other types of medicines for ulcerative colitis target your immune system, too. Your doctor may call these immunomodulators. They may be good options if 5-ASAs and corticosteroids havenât worked well for you.
The most common ones are azathioprine , mercaptopurine , and cyclosporine . Due to the risk of side effects, doctors usually save cyclosporine for people who donât have success with other meds. They may also try methotrexate paired with folic acid.
Ozanimod is an oral medication and is the first sphingosine 1-phosphate receptor modulator approved for patients with moderately to severely active UC.
The goal is to lower inflammation in your colon.
These drugs can have side effects. They can damage your liver and make you more likely to get skin cancers, lymphoma, and infections. If you take them, your doctor will test your blood and check you for skin cancer regularly.
Cyclosporine is especially strong, but it works fast. Your doctor might prescribe it to get a severe flare under control, and then give you 6-MP or azathioprine afterward. The drug may cause kidney problems, gout, infections, and high blood pressure.
It can take several months for some of these drugs to work. So your doctor may give you a faster-acting medicine, like a low dose of a corticosteroid, to help in the meantime.
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
You May Like: Ulcerative Colitis And Colon Cancer Statistics
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Uc Treatment Options At A Glance
The most commonly used treatments for UC:
These drugs, given orally or rectally, are anti-inflammatory compounds that contain 5-aminosalicylic acid . They decrease inflammation at the wall of the intestine. Examples of 5-ASAs include sulfasalazine, balsalazide, mesalamine, and olsalazine.
Metronidazole, ciprofloxacin, and other antibiotics may be used when infections occur, or to treat complications of ulcerative colitis.
Biologics for UC are designed to suppress the immune system to reduce inflammation. Certain biologics work by targeting specific inflammatory proteins called cytokines that play a role in inflammation. Others work by preventing certain white blood cells from getting into inflamed tissues.
Prednisone, prednisolone, and budesonide are included in this type of medication. They affect the bodys ability to initiate and maintain an inflammatory processkeeping the immune system in check. While effective for short-term flare-ups, theyre not recommended for long-term use.
These modify the bodys immune system activity to stop it from causing ongoing inflammation These drugs are usually used for people who have responded only to steroids.
Don’t Miss: How To Use Aloe Vera Gel For Ulcerative Colitis
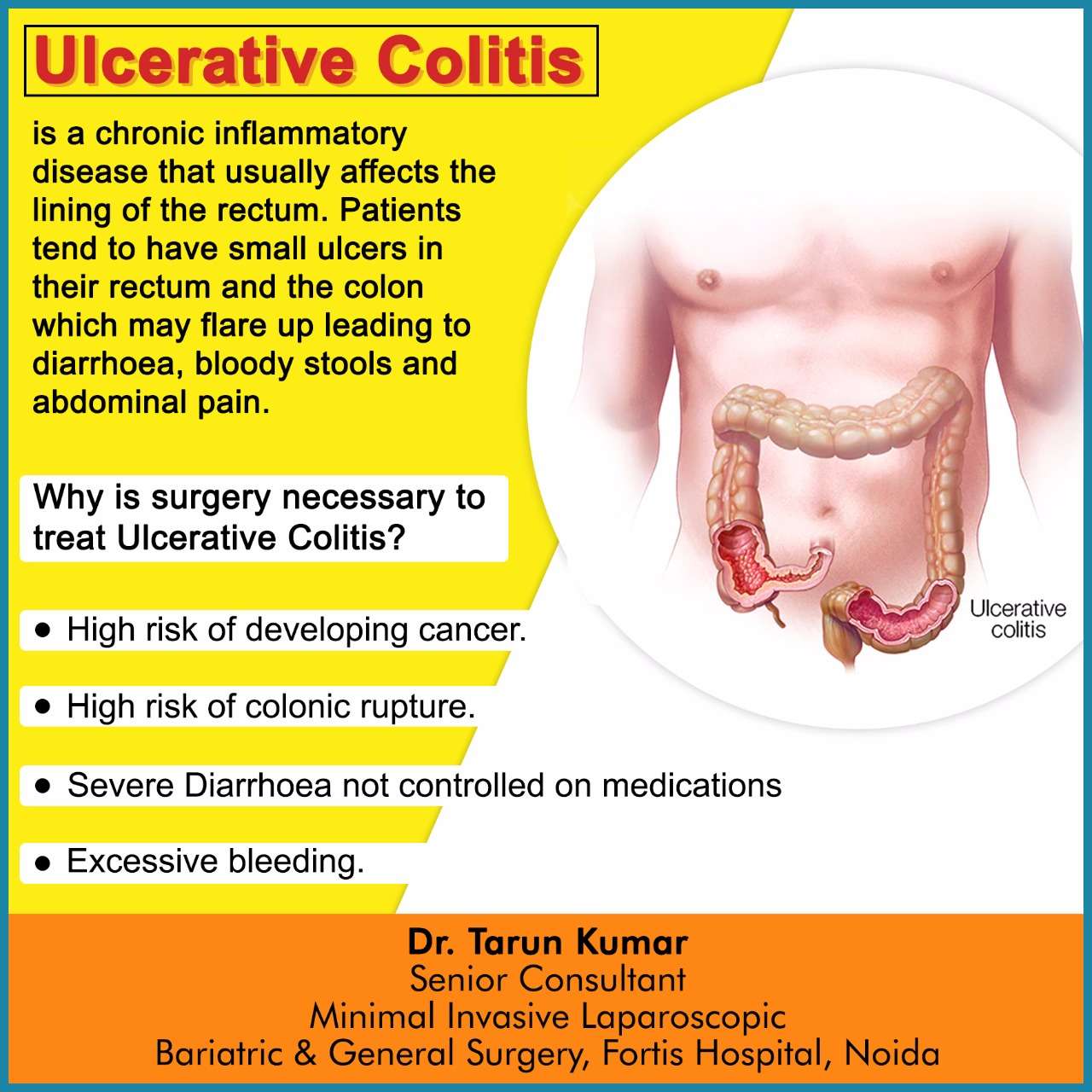
How Does Ulcerative Colitis Progress
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
What Will You Need
Your needs will depend on your symptoms, and each person is different. Your ulcerative colitis could start out as mild, then stop for a while, only to come back worse than it was before. Or you may have only mild ulcerative colitis your entire life.
Plus, your body may not respond the same way to a drug as someone else’s. And over time, you may find that you need a different type of medicine. For example, something thatâs worked well for years may not work anymore. You may need a whole new treatment plan.
Let your doctor know how youâre really doing, and always tell them about any side effects that you have.
Show Sources
Don’t Miss: What Should You Eat With Ulcerative Colitis
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
“Try to engage in a moderate-intensity exercise like swimming or biking, three or four days per week,” he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Recommended Reading: What Causes Stomach Ulcers In Horses
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
What Are Ulcerative Colitis Medications
Since ulcerative colitis cannot be cured by medication, the goals of treatment with medication are to 1) induce remissions, 2) maintain remissions, 3) minimize side effects of treatment, 4) improve the quality of life, and 5) minimize risk of cancer. Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohn’s disease.
Medications for treating ulcerative colitis include 1) anti-inflammatory agents such as 5-ASA compounds, systemic corticosteroids, topical corticosteroids, and 2) immunomodulators.
Anti-inflammatory medications that decrease intestinal inflammation are analogous to arthritis medications that decrease joint inflammation . The anti-inflammatory medications that are used in the treatment of ulcerative colitis are:
- Topical 5-ASA compounds such as sulfasalazine , olsalazine , and mesalamine that need direct contact with the inflamed tissue in order to be effective.
- Systemic anti-inflammatory medications such as corticosteroids that decrease inflammation throughout the body without direct contact with the inflamed tissue. Systemic corticosteroids have predictable side effects with long term use.
It has long been observed that the risk of ulcerative colitis appears to be higher in nonsmokers and in ex-smokers. In certain circumstances, patients improve when treated with nicotine.
Don’t Miss: What Foods Irritate An Ulcer
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Expert Treatments For Ulcerative Colitis
Our inflammatory bowel disease experts deliver advanced care for ulcerative colitis. At the Stanford Inflammatory Bowel Disease Program, you have access to the most advanced care:
- Clinical trials: We offer the latest clinical trials including a trial for the Specific Carbohydrate Diet as Maintenance Therapy in Crohn’s Disease.
- Innovative medical treatment: Our experts have unique expertise in creating medical treatment plans for individual patients.
Read Also: Nasal Cannula Pressure Ulcer Prevention
Medication Options For Ulcerative Colitis
Medication is the first line of treatment for ulcerative colitis. Your doctors recommendation for which medication will work best for you is based on the severity of your disease, your overall health, and other individual factors.
There are six major classes of medication used to treat ulcerative colitis.
Side Effects Of Ulcerative Colitis
Side effects are based on the biologic medication that youre receiving. While some are minor, others may be life-threatening. You should talk to your doctor before receiving infusion therapy to ensure that you are getting the best option for your UC. The most common side effects include:
- Serious allergic reactions
- Lymphoma and other cancers including skin and cervical cancer
- Heart problems including failure
- Psoriasis
Also Check: Foot Ulcer Treatment At Home
Avoid Foods That May Exacerbate Uc Symptoms
Because a healthy diet is a cornerstone for overall health, its no surprise that it tops Sniders list of natural remedies for ulcerative colitis. Diet is a foundational treatment for patients with ulcerative colitis, he says, adding that there’s often a dietary component to the disease.
According to a review published in October 2014 in Clinical Gastroenterology and Hepatology, people who reported a diet high in fats were more likely to have a relapse of UC. Other studies highlighted in the paper suggested avoiding greasy foods, dairy products, caffeine, and raw fruits and vegetables if you have ulcerative colitis. But the review notes that theres no one-size-fits-all diet for UC, so youll have to figure out what works best for you through trial and error.
It helps to keep a food diary to discover which foods are best for you. Snider says it can’t hurt to limit certain foods, and then if your symptoms improve according to your symptom diary, to continue doing so. He also notes that it’s worthwhile to avoid sugar because its effect on the pancreas hinders the output of anti-inflammatory enzymes.
The 3 Key Goals Of Uc Treatment
There are treatments available that can help control excess inflammation in order to help you:
Controlling inflammation can help relieve UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain.
Controlling inflammation can also help you achieve and maintain remission. This means you have achieved ongoing symptom relief and are able to prevent flares.
Controlling inflammation over time allows the lining of the colon to heal and can help you maintain remission.
Also Check: How Do They Treat Ulcerative Colitis
Signs And Symptoms Of Ulcerative Colitis
While the clinical signs of ulcerative colitis can vary from child to child, some symptoms may be more common than others, including bloody diarrhea. Other symptoms related to inflammation in the colon may include: abdominal pain, urgent or uncontrollable bowel movements, poor appetite, weight loss, and fatigue. Some children may experience less common symptoms, including skin rashes, joint pain, fatigue or fevers.Ulcerative colitis is a chronic condition, meaning children may have periods of no symptoms alternating with periods of active symptoms . Mild symptoms may present at first, while in other children, the onset of symptoms is more severe.