What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
What You Eat In The Morning
While eating certain foods does not usually trigger IBD flares, it could worsen existing flares and symptoms. The Crohns & Colitis Foundation recommends avoiding the following food categories that can worsen a persons symptoms during a flare:
- Greasy, fried foods Fast food, fried potato chips, donuts, etc.
- High-fiber foods Raw vegetables and fruit
- Gas-inducing foods Beans, cabbage, broccoli
- Gas-inducing drinks Caffeinated or carbonated beverages
- Problem foods Foods you recognize as personal flare triggers
Things No One Tells You About Life With Ulcerative Colitis
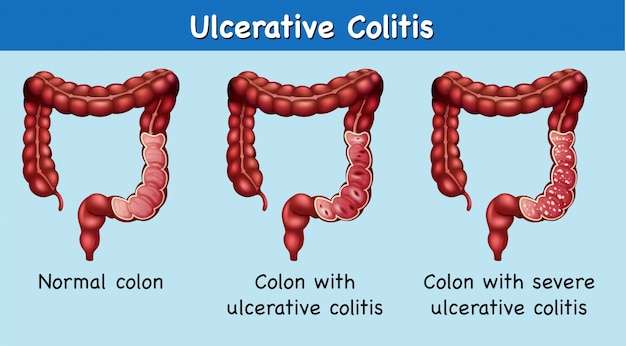
People who have never experienced ulcerative colitis may think it means getting the occasional bad stomachache or having a fussy gastrointestinal system. But as anyone with ulcerative colitis knows, the effects of this inflammatory bowel diseasein which sections of the large intestine develop inflammation and ulcerscan be severe and disrupt many aspects of your life. After a diagnosis of ulcerative colitis, it can be incredibly hard to navigate the reality of your new normal. Knowing the following seven facts about life with ulcerative colitis might help make the whole experience a little bit easier.
Don’t Miss: What Should You Eat With Ulcerative Colitis
Symptoms Can Range Widely In Severity And Frequency Between People
Ulcerative colitis causes inflammation and ulcers along the lining of your intestines. This condition can be uncomfortable, but with effective treatments you can manage your symptoms with ease and focus o. Ulcerative colitis is a health condition that affects your digestive tract, and thats one of the main reasons why its important to watch your diet. Ulcerative colitis from the inside out written by elizabeth pratt a person living with ulcerative colitis is three times more likely to develop sacroiliitis written by jenna fletcher written by charlotte lillis 3 studies cited written by j. Wondering how much your medical care wil. Medication is one of many options to help treat ulcerative colit. The best treatment for ulcerative colitis depends on the severity of the condition. Ulcerative colitis is a form of inflammatory bowel disease. Many of its early symptoms resemble those of other conditions, which is why its important to learn more about what dist. Ulcerative colitis is a chronic condition that develops in your intestines over time and has symptoms that come and go. The colon carries waste to be expelled from the body. Can physical or cognitive activity prevent dementia? Overview of ulcerative colitis, an inflammatory bowel disease does your child need to bathe every day?
You Need An Adjustment Of Your Meds
Antibiotics for an infection outside of your gut could aggravate UC symptoms. Let your doctor know if you start to experience diarrhea after starting antibiotics, since a switch in the type of drug might be needed.
Your doctor may also suggest taking an antidiarrheal medication or a probiotic, which may help reduce diarrhea.
Don’t Miss: Can I Take Tylenol With An Ulcer
If Ibd Symptoms Like Diarrhea And Abdominal Pain Get In The Way Of Restful Sleep Here Are Some Tips That Will Help You Get The Restful Sleep You Need
When you have inflammatory bowel disease , which can include ulcerative colitis and Crohn’s disease, symptoms like diarrhea and abdominal pain can get in the way of restful sleep. And when you don’t get restful sleep, you may notice that those troubling symptoms of IBD appear to worsen.
A recent report found that poor sleep has been independently linked to depression and poorer IBD-related quality of life, which is understandable since adequate sleep is necessary for normal brain function, proper emotional stability and overall physical health.
To help break this bad-sleep cycle, here are some tips that will help you get the rest you need.
Fend off night sweats Night sweats can interrupt your sleep. Maintain a comfortable bedroom temperature. Use air conditioning or a fan or open a window if you don’t already do so. Wear loose-fitting, lightweight, cotton pajamas . Use layered bedding that can be removed if necessary.
Monitor caffeineCaffeine intake can irritate IBD symptoms and prevent sleep. Know your limits some people are more sensitive to caffeine than others. Up to 400 milligrams of caffeine a day appears to be safe for most adults, according to the Mayo Clinic. How much is that? It’s about the amount of caffeine in four cups of brewed coffee, 10 cans of cola or two “energy shot” drinks.
This post was created with support from Bausch Health.
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
You May Like: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
Ways To Have Healthy Sleep With Ulcerative Colitis
1. Change your sleeping position
Sleeping position makes a great deal in terms of relieving pain and having better sleep. Choose a sleep position in which you feel more comfortable, mostly sleep straight against your back. This sleeping position suits most of the people who suffer from this disease. Certain sleeping positions may increase the flares and inflammation in intestines. So to reduce the symptoms and inflammation it is better to change your sleeping position till ulcerative colitis gets treated.
2. Revise your Medications
This is required because sometimes the medications which are going are not that effective on your body and needs to be changed. If the medication is not helping you with the disease, then it might increase pain rather than giving relief from it. Also certain UC medicines can also cause difficulty in sleeping like corticosteroids. This medication is used for controlling ulcerative colitis flares but it gets hard to sleep after taking this medicine. You need to consult you doctor for change in medication or alternative medicine. The doctor may advice you the following-
- To change medication
- Adding some medicine or pills to help you sleep
- Changing the time of medication to day time
3. Eat Dinner Early
Triggers of UC related to diet include the following-
- Lactose
Also Read- Digestive Issues During COVID Recovery. Heres What You Need To Know
4. Improve your Mental Health
5. Practise Good Sleeping Habits
6. Heating Pads and Sleep Aids
- Diarrhoea
To Treat Or Not To Treat
Because Crohns is usually painful and is associated with complications including bowel perforation, anemia and malnutrition, patients are usually treated with medications to calm down the immune system and reduce the inflammation. These are powerful drugs that suppress the immune system. They are very effective at controlling the pain and destruction but can leave a patient open to infection. Because of that, its less clear how to treat patients with asymptomatic disease. For those with no pain and no signs of inflammation, watchful waiting is a common strategy.
The same type of medications are used to treat the arthritis associated with inflammatory bowel disease. The physician wasnt sure if it made sense for him to use an immune-suppressing medicine while seeing sick patients. His rheumatologist, seeing him put the pad on his seat before gently lowering himself onto the chair, was much less uncertain. She had put many people on these medications, she told him some of them doctors. Most did fine. He agreed to start taking it. The effect was immediate and amazing. His pain a regular visitor for nearly a decade is gone. Even at the end of the day, his walk to and from his car is painless. He still uses the pad at times those bones are still a little tender. But the rest of him feels great.
Recommended Reading: Medical Card For Ulcerative Colitis
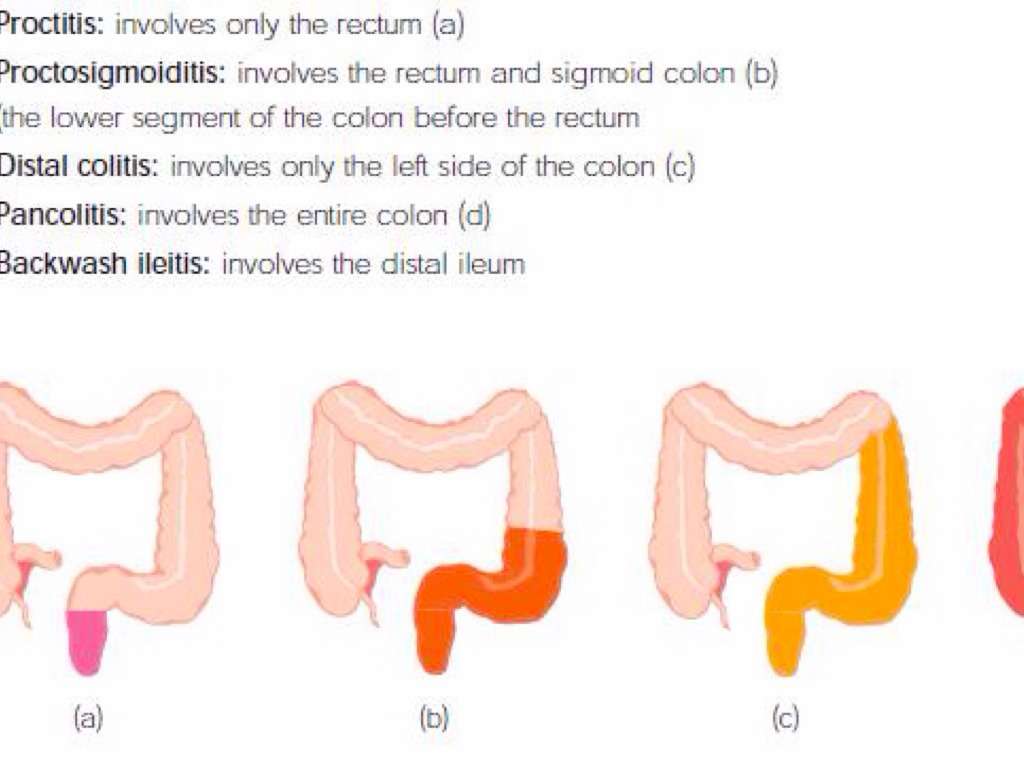
Symptoms By Type Of Ulcerative Colitis
Ulcerative colitis can be broken into subtypes depending on where the inflammation is in your colon.
- Ulcerative proctitis. Ulcerative proctitis affects your rectum, the part of your colon closest to your anus. Its the most common type and affects 30 to 60 percent of people with ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis causes inflammation of your rectum and the lower part of your colon, called the sigmoid colon.
- Left-sided colitis. Left-sided colitis affects your rectum, your sigmoid colon, and the descending part of your colon on the left side of your body.
- Pancolitis.Pancolitis affects your entire colon.
Symptoms typically become worse as inflammation spreads farther along your colon.
| Ulcerative proctitis |
show ulcerative colitis is slightly more prevalent in men, but most studies show no difference.
Symptoms of ulcerative colitis are similar regardless of sex, but unique issues may occur for some people.
Rectovaginal fistulas may develop, which are holes that allow stool to leak from the bowel to the vagina.
Ulcerative colitis may also lead to irregular periods or increased menstrual pain. Women may also be at a higher risk of anemia and osteoporosis, and ulcerative colitis can further increase this risk.
Complications Of Ulcerative Colitis
Problems from ulcerative colitis can include:
- Narrowed areas of the intestine . They can make it hard to pass stools.
- Increased risk of cancer of the colon and rectum. This risk is higher than average if you have had ulcerative colitis for 8 years or longer.
- Complications outside the digestive tract. These include joint pain, skin problems, and eye problems.
- The colon swelling to many times its normal size. This is called toxic megacolon. Its rare, but it needs treatment right away.
- Other rare complications, such as scarring of the bile ducts and the pancreas.
- Inflammatory bowel disease, which also increases the risk of melanoma, a serious type of skin cancer. Your doctor may recommend regular screening by a dermatologist.footnote 2
Also Check: How To Use Aloe Vera Gel For Ulcerative Colitis
You May Like: Can You Cure Ulcerative Colitis Naturally
Youre Drinking Caffeine Or Alcohol
Coffee, tea, and sodas can make UC flare-ups worse, says Yun, because caffeine is a stimulant that can get your intestines going not what you need when you have diarrhea. The same goes for beer, wine, and liquor. People with active UC symptoms should consider skipping caffeinated and alcoholic drinks.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Don’t Miss: Nutritionist Specializing In Ulcerative Colitis
Poor Sleep Patterns Could Increase Your Chance Of Developing Ulcerative Colitis
While it remains mostly a mystery why we need sleep, what we do know is that it is a crucial part of maintaining good health. Not getting the right amount of sleep can leave you feeling tired and groggy, it can affect your mood and appetite, make your concentration dwindle, and even exacerbate certain illnesses. On top of all this, new research shows that not getting enough sleep, or sleeping too much, can increase your chance of developing ulcerative colitis , a chronic inflammatory bowel disease , consisting of fine ulcerations in the inner mucosal lining of the large intestine. UC can be a devastating disease, with sufferers experiencing diarrhea, rectal bleeding, and abdominal cramping.
A well-known study, following more than 150,000 female nurses for more than 30 years, found that the women who slept on average 6 hours a night or fewer were slightly more likely to develop UC than those who slept for 7-8 hours each night.1 Even more alarmingly, was that those who slept for more than 9 hours each night were more than twice as likely to develop UC as those who slept the ideal amount.
If you are concerned about the effects that a lack of sleep could be having on you, then consult your physician.
First published in the Inside Tract® newsletter issue 192 2014
1. Ananthakrishnan AN. et al. Sleep Duration Affects Risk for Ulcerative Colitis: A Prospective Cohort Study. Clinical Gastroenterology and Hepatology. 2014 12:1879-86.
Image: Free-Photos from Pixabay.com
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Also Check: How To Tell If You Have A Stomach Ulcer
What Is The Sleep
Animal studies have shown that sleep deprivation can lead to worse colitis. This is true of both tissue markers and symptoms. Many studies show a 2-way street between sleep and immune diseases, including those with Crohns and UC.4
Even when IBD is not in the picture, researchers have made many links between sleep and our immune systems. For instance, good sleep helps the body fight infection.1
Sleep deprivation negatively affects T-cells into the following day. T-cells are part of the immune system that help protect the body from infection. Sleep deprivation is also linked to increases in pro-inflammatory markers such as cytokines. These are cells involved in the immune system.1,5
Crohns Disease And Ulcerative Colitis
A serious but rare complication of these forms of inflammatory bowel disease is fulminant or toxic colitis, formerly called toxic megacolon.
The signs and symptoms of this condition can include bloody diarrhea along with fever, racing heartbeat , low blood pressure , metabolic acidosis , low urine output , and acute kidney failure.
Toxic colitis is more common with ulcerative colitis than it is with Crohns disease.
Read Also: Best Supplement For Gastric Ulcers In Horses
Read Also: Foods To Avoid With Peptic Ulcer
Ulcerative Colitis Is A Chronic Condition That Develops In Your Intestines Over Time And Has Symptoms That Come And Go
Symptoms can range widely in severity and frequency between people. Ulcerative colitis is a type of inflammatory bowel disease that causes inflamed sores on the colon or large intestine. Ulcerative colitis from the inside out written by elizabeth pratt a person living with ulcerative colitis is three times more likely to develop sacroiliitis written by jenna fletcher written by charlotte lillis 3 studies cited written by j. Overview of ulcerative colitis, an inflammatory bowel disease does your child need to bathe every day? The colon, also called the large intestin. Ulcerative colitis is a chronic condition that develops in your intestines over time and has symptoms that come and go. Ulcerative colitis is an autoimmune disease that causes the immune system to attack the colon, leading to a range of painful signs and symptoms, both in the gastrointestinal tract and in other parts of the body. Ulcerative colitis is a form of inflammatory bowel disease. Many of its early symptoms resemble those of other conditions, which is why its important to learn more about what dist. Ulcerative colitis is a health condition that affects your digestive tract, and thats one of the main reasons why its important to watch your diet. Home digestive disorders centertopic guide ulcerative colitis is an acute or chronic inflammation of the colon . Here’s what you need to know about available options. Wondering how much your medical care wil.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Recommended Reading: Best Foods To Eat If You Have An Ulcer