Ulcerative Colitis And Cancer Of The Colon
The chance of developing cancer of the large intestine is higher than average in people who have had ulcerative colitis for several years or more. It is more of a risk if you have frequent flare-ups affecting the whole of the large intestine. For example, about 1 in 10 people who have ulcerative colitis for 20 years which affects much of their large intestine will develop cancer.
Because of this risk, people with ulcerative colitis are usually advised to have their large intestine routinely checked after having had the condition for about 10 years. This involves a look into the large intestine by a flexible telescope every now and then and taking small samples of bowel for examination. It is usually combined with chromoscopy – this is the use of dye spray which shows up suspicious changes more easily. Depending on the findings of this test and on other factors, you will be put into a low, intermediate or high risk category. ‘Other factors’ include:
- The amount of intestine affected.
- Whether you have had complications such as polyps. These are small, non-cancerous growths on the inside lining of the colon or rectum.
- Whether you have a family history of cancer.
The National Institute for Health and Care Excellence recommends the next colonoscopy/chromoscopy should depend on the degree of risk of developing colon or rectal cancer. After the next test, your risk will be calculated again.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
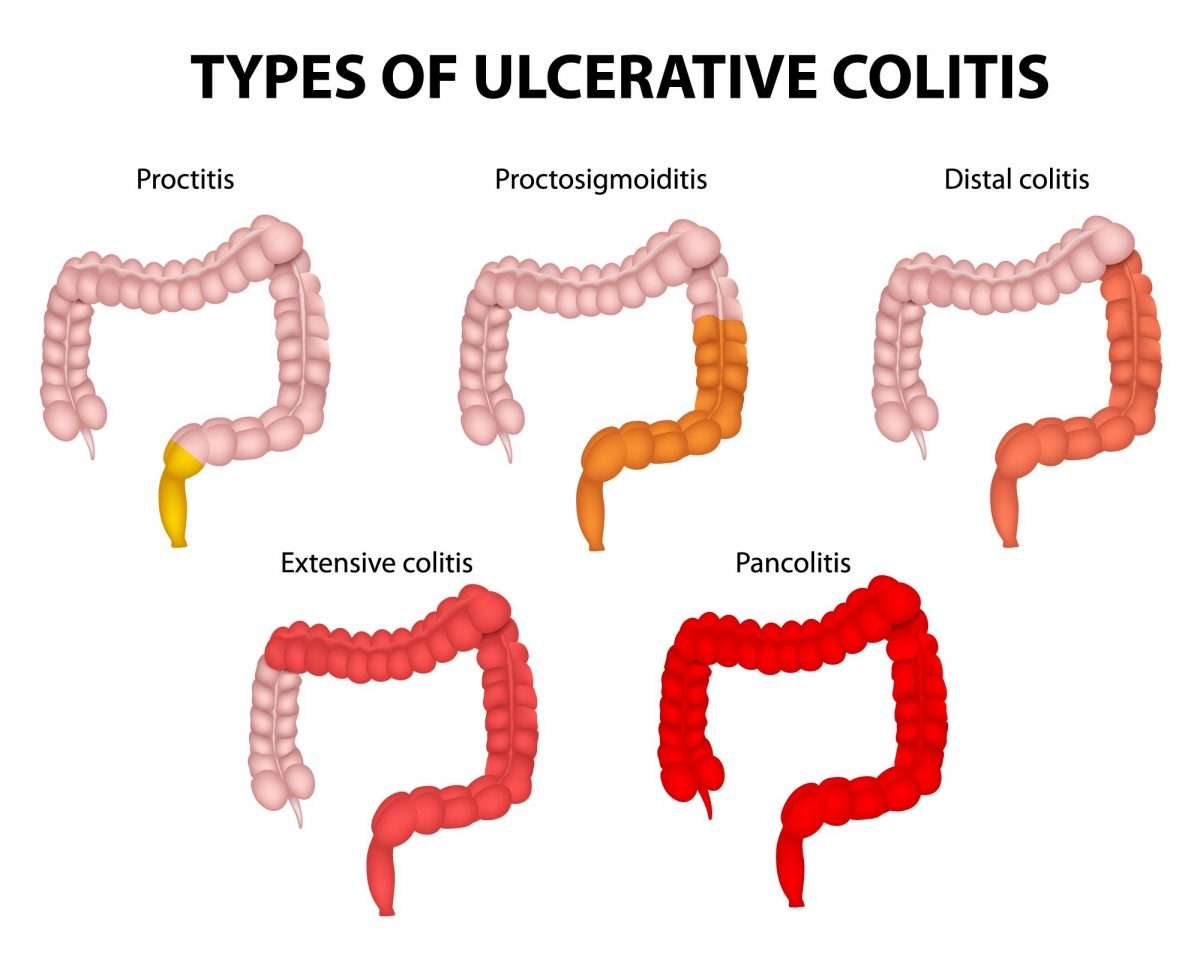
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Recurring Or Severe Symptoms Of Ulcerative Colitis
Doctors examine people when their typical symptoms return, but they do not always do tests. If symptoms have been more frequent or longer-lasting than usual, doctors may do sigmoidoscopy or colonoscopy and a blood count. Doctors may do other tests to look for infection or parasites.
When symptoms are severe, people are hospitalized. Doctors take x-rays to look for a dilated or perforated intestine.
Also Check: What Are The First Signs Of A Stomach Ulcer
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Eating Diet And Nutrition
Researchers have not found that eating, diet, and nutrition play a role in causing ulcerative colitis symptoms. Good nutrition is important in the management of ulcerative colitis, however. Dietary changes can help reduce symptoms. A health care provider may recommend dietary changes such as the following:
- avoiding carbonated drinks
People should speak with a health care provider about specific dietary recommendations and changes.
Don’t Miss: How Can You Get Rid Of Ulcers
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
Recovering From Colectomy Surgery
After your surgery you may need to stay in hospital for around a week until you regain normal bowel function. The length of your stay will also depend on whether you had open or laparoscopic surgery.
You may receive nutrition through an intravenous drip until your bowel has healed a little and you are able to drink more normally. You will probably be encouraged to eat and drink as soon as you feel able and will be encouraged to move around.
If your surgery involved the formation of a stoma then you will see an ostomy nurse who will teach you how to care for it.
It will probably take several weeks after leaving hospital for you to begin to feel better. You will probably be advised against any heavy lifting or strenuous physical activity and you may not be able to drive for a couple of weeks.
You may be recommended to follow a certain diet, or avoid certain foods, in the weeks immediately after surgery to aid healing.
Donât Miss: Can Diverticulitis Cause Ulcerative Colitis
Also Check: How Severe Is Ulcerative Colitis
Ulcerative Colitis And Colon Cancer
People with ulcerative colitis may be more likely to develop colon cancer when:
- ulcerative colitis affects the entire colon
- a person has ulcerative colitis for at least 8 years
- inflammation is ongoing
- people also have primary sclerosing cholangitis, a condition that affects the liver
- or a person is male.
People who receive ongoing treatment and remain in remission may reduce their chances of developing colon cancer.
People with ulcerative colitis should talk with their health care provider about how often they should get screened for colon cancer. Screening can include colonoscopy with biopsies or a special dye spray called chromoendoscopy.
Health care providers may recommend colonoscopy every 1 to 3 years for people with ulcerative colitis who have:
- the disease in one-third or more or of their colon, or
- had ulcerative colitis for 8 years.
Such screening does not reduce a person’s chances of developing colon cancer. Instead, screening can help diagnose cancer early and improve chances for recovery.
Surgery to remove the entire colon eliminates the risk of colon cancer.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Recommended Reading: List Of Foods Good For Ulcers
How Does Ulcerative Colitis Progress
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
How Does It Affect You
The condition also leads to several health issues. For example, people with this disorder often experience unhealthy weight loss as they have difficulty absorbing enough nutrients and fluids from their diet.
In addition, affected children usually grow more slowly than usual. Although it is not so common, Ulcerative Colitis causes skin, eyes, joints, kidneys, or liver issues. However, these complications occur most likely due to abnormal inflammation. Furthermore, Ulcerative Colitis also increases the risk of colon cancer, especially in people having the disease for years.
Ulcerative colitis is one of the two major types of inflammatory bowel disease . Crohns disease is another type of IBD that causes chronic inflammation of the intestines. However, unlike ulcerative colitis, which affects only the inner surface of the large intestine, Crohns disease may cause inflammation in any part of the digestive system. In addition, the inflammation extends deeper into the intestinal tissue.
Don’t Miss: What To Eat And Drink If You Have An Ulcer
When Youre In The Hospital
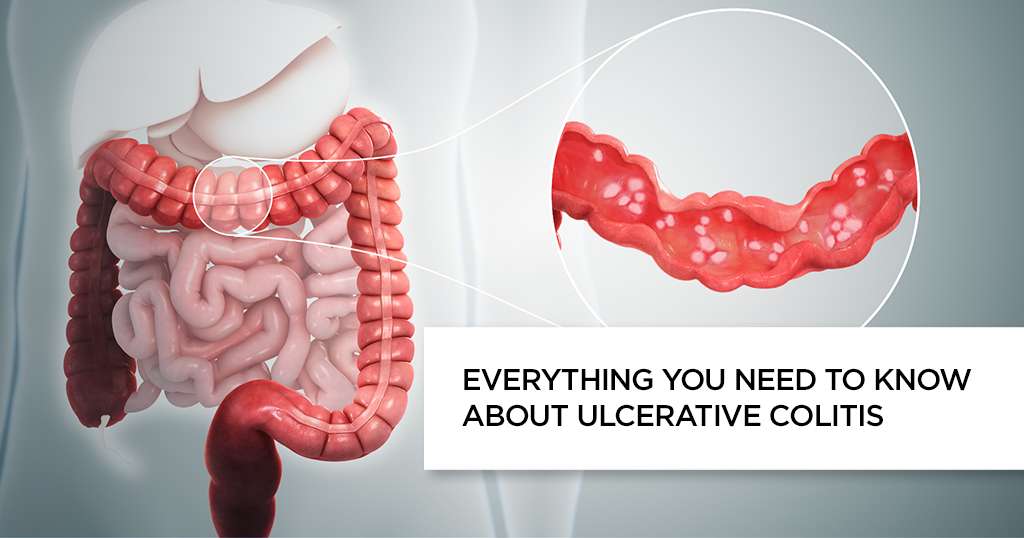
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
Read Also: How Long Do Stomach Ulcers Last
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Ulcerative Colitis: Diet And Management
After you have been diagnosed with ulcerative colitis, you might be asking what you should and shouldnt eat to best take care of your body. Eating well is especially important with ulcerative colitis, since symptoms can lead to weight loss and malnutrition. Unfortunately, there are no hard-and-fast rules when it comes to UC and diet.
Your healthcare team may recommend that you go on an elimination diet. This is a temporary diet that involves avoiding, and then slowly reintroducing, certain foods to see what foods trigger your symptoms. Only follow this diet under our doctors supervision to make sure you are getting adequate nutrition.
Other tips you can try include:
Recommended Reading: Hindgut Ulcers In Horses Treatment
Don’t Miss: What To Eat When You Have Gastric Ulcer
Stress And Ulcerative Colitis
Experts havenât found an exact link. But they have some theories about the connection between the two.
Inflammation. Your body goes into fight-or-flight mode when stressed. That triggers the release of lots of chemicals, including cytokines. Those are molecules that turn on your immune system and lead to inflammation. People with UC might be more sensitive to this process.
Brain-gut axis. Stress changes the signals that travel between your brain and gut. This can cause all kinds of digestion problems, even in people who donât have UC. These changes are also linked to irritable bowel syndrome , food allergies, and heartburn.
Other reasons. Research shows stress might:
- Damage the lining of your gut
- Disturb gut bacteria
- Change how fast or slow your digestive muscles work
- Make your gut more sensitive to pain
Recommended Reading: Can Ulcer Cause High Blood Pressure
Could My Symptoms Be Ibs
Irritable Bowel Syndrome is a different condition from IBD, although some of the symptoms are similar. Like Crohns and Colitis, IBS can cause abdominal pain, bloating and bouts of diarrhoea or constipation. However, it does not cause the type of inflammation typical of Colitis, and there is no blood loss with IBS.
Some people with Colitis may develop IBS-like symptoms, for example experiencing diarrhoea even when their Colitis is inactive. These symptoms may need slightly different treatment from their usual IBD symptoms. IBS is more common in people with IBD than in the general population.
If you develop diarrhoea with bleeding and abdominal pain, your doctor may suspect you have Colitis, particularly if you are a young adult or have a family history of Crohns or Colitis. You will need tests and physical examinations to confirm a diagnosis. See Tests and Investigations for IBD.
You may need to have tests repeated from time to time to check on your condition and how your treatment is working.
Some drug treatments may also require a series of blood tests and, occasionally, x-rays or scans to check for any potential side effects. Your specialist will avoid giving you any unnecessary tests or investigations.
You may need more regular colonoscopies when you have had Ulcerative Colitis for a long time to check for any signs of cancer.
You May Like: Best Pain Relief For Leg Ulcers
Causes And Risk Factors
The exact causes of ulcerative colitis are unknown. Researchers observe that:
- Genetics plays some role. Many people with ulcerative colitis have family members with inflammatory bowel disease.
- Ulcerative colitis is diagnosed most often in people ages 15 to 35. However, it can occur at any age, including in older people.
- Ulcerative colitis is more common among whites than people of other races. Jewish people of Eastern European descent have a higher than average risk of developing this disease.
What Is The Large Intestine
The large intestine is part of the GI tract, a series of hollow organs joined in a long, twisting tube from the mouth to the anusan opening through which stool leaves the body. The last part of the GI tract, called the lower GI tract, consists of the large intestinewhich includes the appendix, cecum, colon, and rectumand anus. The intestines are sometimes called the bowel.
The large intestine is about 5 feet long in adults and absorbs water and any remaining nutrients from partially digested food passed from the small intestine. The large intestine changes waste from liquid to a solid matter called stool. Stool passes from the colon to the rectum. The rectum is located between the lower, or sigmoid, colon and the anus. The rectum stores stool prior to a bowel movement, when stool moves from the rectum to the anus and out of a person’s body.
Read Also: 8 Foods To Eat During An Ulcerative Colitis Flare