What Should I Eat During A Flare
During a flare-up, parts of the large intestine become inflamed, causing diarrhea and discomfort. Many experts recommend going on a low-residue diet — one that cuts out foods that are hard to digest or that contain indigestible fiber. That means avoiding fruits and vegetables, nuts and seeds, and whole grains.
Some doctors recommend a liquid diet during severe flare-ups. With no food passing through the large intestines, the bowels have time to heal.
Again, keep in mind that different people may respond differently.
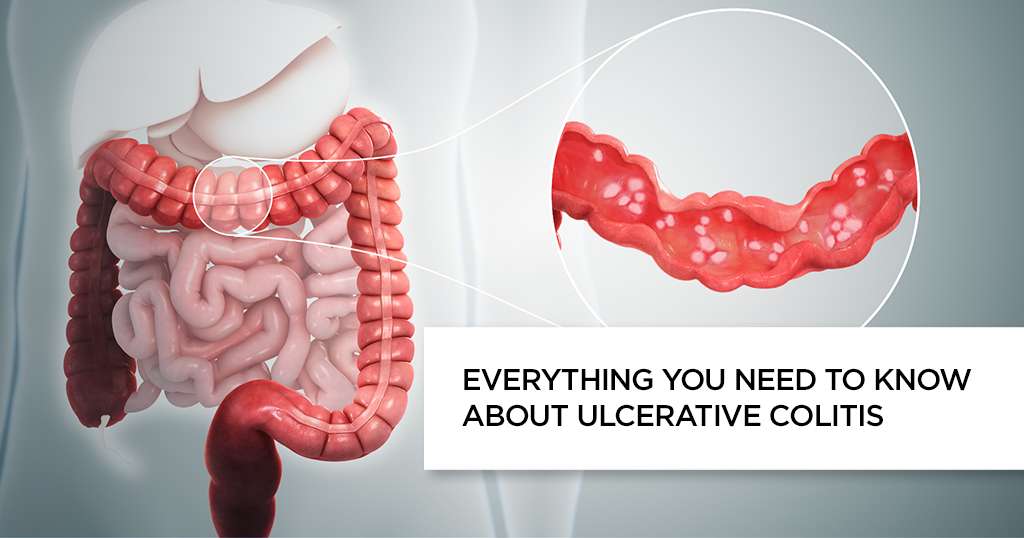
Types Of Ulcerative Colitis
Depending on the area of the colon affected, ulcerative colitis can be classified into several types, including:
- Ulcerative proctitis is typically the mildest type limited to the rectum and characterized by a total blurring of the normal vascular pattern and rectal bleeding.
- Left-sided colitis is found in patients in whom the inflammatory process extends up to the splenic flexure and usually leads to defecation urgency, bloody diarrhea, and associated weight loss.
- Pancolitis occurs when the entire colon is affected and results in abdominal pain, cramps, fever, blood in stool, and significant weight loss.
- Proctosigmoiditis involves the rectum and the part of the colon closest to it . Key symptoms include moderate pain on the lower left side of the abdomen, bloody diarrhea, and the inability to control bowel movements.
Manhattan Gastroenterology physicians are expertly trained and experienced in diagnosing and treating ulcerative colitis no matter the severity of disease and part of the colon affected. Get in touch with us today and start your journey to a pain-free and healthy life.
Cannabinoids Affect Endocannabinoid System In Ulcerative Colitis
An Israeli study published in 2021 investigated the impact of cannabinoid therapy on the endocannabinoid system and clinical symptoms in patients with IBD. The 2-month study examined the effects of THC-dominant cannabis flowers and placebo in Chrons disease and ulcerative colitis. Twenty-two subjects received cannabis and another 27 participants received placebo for smoking. During the course of the study, blood samples and intestinal tissue samples were taken to examine the function of the ECS .
Endocannabinoids and endocannabinoid-like substances examined in the blood :
- anandamide
- arachidonic acid
Enzymes studied on colon tissue :
- N-acylphosphatidylethanolamine-selective phospholipase D : this enzyme is required for the formation of endocannabinoids. NAPE-PLD is used for the biosynthesis of N-acylethanolamines such as anandamide .
- fatty acid amide hydrolase : this enzyme serves to degrade endocannabinoids. FAAH deactivates various fatty acid amides such as anandamide and oleic acid amide .
The studies showed a different function of the ECS in patients depending on the diagnosis : in all 30 affected patients with Crohns disease, endocannabinoids remained unchanged, regardless of whether cannabis or placebo was used.
The study shows that cannabis therapy can positively influence the endocannabinoid system in ulcerative colitis, thereby alleviating symptoms .
You May Like: What Is A Good Diet For Ulcerative Colitis
What Tests Are Used To Monitor Ulcerative Colitis
Doctors have a wide variety of tests that help diagnose and track inflammatory bowel diseases. Imaging tests and colonoscopies are done to check the bowels. Biopsies are sometimes taken to look at cells in the lining of the intestines. Blood tests are used to spot nutritional shortfalls and anemia, a common side effect of ulcerative colitis. Stool sample tests can detect infections in the intestines.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Don’t Miss: Is Colitis And Ulcerative Colitis The Same Thing
Ulcerative Colitis And Medicinal Cannabis
HomeNewsArticles and publicationsUlcerative colitis and medicinal cannabis
Many studies point to the medical potential of the cannabis plant. Among other things, its ingredients are said to have a pain-relieving and anti-inflammatory effect, which could be beneficial in the chronic disease ulcerative colitis.
Like Crohns disease, ulcerative colitis is a chronic inflammatory bowel disease . While ulcerative colitis only inflames the rectum and in some cases the colon, Crohns disease affects the entire digestive tract.
Another distinguishing feature of the two diseases is that the center of inflammation in ulcerative colitis is usually limited to the intestinal mucosa . In contrast, in Crohns disease the source can spread to all layers of the intestinal wall.
Ulcerative Colitis: What You Need To Know
- Ulcerative colitis is similar to Crohns disease. An experienced gastroenterologist will be able to diagnose you accurately.
- Diarrhea, often with blood, is the main symptom of ulcerative colitis.
- Monitoring the frequency and severity of attacks can help diagnose ulcerative colitis.
- Many patients respond well to a course of medication. If medication does not provide relief, surgery is another treatment option.
Ulcerative colitis has many similarities to Crohns disease, another inflammatory bowel disease. They can be difficult to tell apart, although there are differences in the symptoms and the physiology of the disease.
Also Check: I Think I Have An Ulcer What Should I Do
Are There Any Medical Procedures For Uc
Surgery is recommended for severe UC that doesnt respond to therapy or those with life-threatening complications. If you have surgery to correct UC, there are two options to allow waste removal from your body. With an ileostomy, a surgeon creates an opening in your abdominal wall and diverts the small intestines through this hole. An external bag attached to the outside of your abdomen collects waste. An ileo-anal pouch may be surgically constructed at the end of your small intestines and attached to your anus, allowing for more natural waste removal.
Ulcerative Colitis Find The Correct Physician
Basically visit a specialist, is my regular physician still responsible for my care?
Yes. For those who have UC, your doctor will normally have referred you to definitely a gastroenterologist , who:
Made diagnosing and began yourself on treatment, keeping the PCP accustomed to your care
Came back you to definitely your PCPs care once treatment introduced your signs and symptoms in check
Remains open to assist with your care in case your UC signs and symptoms worsen or else you develop UC-related complications
The end result is, your PCP should remain most of your partner in health while dealing with your gastroenterologist if signs and symptoms get free from control. Make sure to speak to your physician in the first manifestation of changes.
What are a few things I ought to look into selecting the best physician for me personally?
Selecting a physician is definitely an individual decision. This is also true whenever you or someone you love has ulcerative colitis , by which painful and frequently socially embarrassing signs and symptoms appear and disappear with distressing unpredictability. Inside your day-to-day existence with this particular chronic rollercoaster disease, your physician can offer not just the therapy youll need but the steady reassurance that both of you, not your UC, have been in control.
Here are a few guidelines for selecting the best physician to deal with your UC.
Level of comfort counts. Think about:
Also Check: How To Cure Gastritis And Ulcers Naturally
Treatment Options For Crohn’s And Colitis
Our team of experts offers broad-based knowledge in every area of IBD treatment, including innovative immune-suppressing drug therapy. And, we can offer patients treatment options only available in large centers such as ours.
The type of treatment varies from patient to patient. We determine treatment based on symptoms, severity and other characteristics of the disease and then customize to fit your individual needs. IBD treatments include:
How Often Should I See A Doctor For Follow
As you may have guessed, those with UC will need more frequent colonoscopies than the average person, says Dr. Lin. A healthy adult should get a colonoscopy every 10 years starting at age 50, according to the Centers for Disease Control and Prevention, But if youve had UC for at least eight years, youll need a colonoscopy every one to two years to screen for colorectal cancer.
Ask your doctor about how often you should receive other follow-up care, including blood work. This schedule will morph over time as your condition changes for example, if youre in remission, youll likely need less frequent doctors visits.
You May Like: How Do You Cure Ulcerative Colitis
Complementary Treatments And Therapies
You may consider these approaches in addition to what your doctor prescribes. But itâs important to talk to your medical team about any and all of them because some, like supplements, can interfere with treatments from your doctor. Letâs take a look at a few:
Mind-body therapies:Stress and anxiety are well-known triggers for many people with ulcerative colitis, so it is not surprising that mind-body relaxation techniques could help. These techniques help nurture a healthy connection between your mind and body as well as between you and the outside world. In some cases, they encourage behavior changes in your everyday life. They may be worthwhile if only to lessen anxiety and depression linked to UC and improve quality of life. In addition, there is some evidence that yoga, meditation, and gut-centered hypnotherapy could help with some physical symptoms or flare-ups of UC. Some of the techniques, like cognitive behavioral therapy and patient support groups, have been so successful that they have slowly become a part of mainstream treatment for IBD.
Keep in mind that the FDA doesn’t regulate supplements, so claims on packaging may not be accurate. Thatâs yet another reason why itâs important to talk to your doctor before you start taking any supplements for your UC.
What Should I Ask My Doctor

If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Don’t Miss: Best Grain For Horses With Ulcers
Colitis And Crohn’s Disease Center
The UCSF Colitis and Crohn’s Disease Center provides comprehensive care for people with inflammatory bowel disease , including Crohn’s disease, ulcerative colitis, microscopic or collagenous colitis, and related illnesses. Advances in the understanding of IBD are rapidly expanding the therapeutic options for patients with these conditions. Our specialists are dedicated to providing every patient with high-quality care, and they’re at the forefront of research to develop new IBD treatments and find a cure. They also educate other doctors across the country on innovative treatment options, with a mission to expand patient access to the best care.
Our team of experts includes adult and pediatric gastroenterologists, surgeons, radiologists, pathologists, immunologists, nutritionists, psychologists, ostomy nurses and social workers. Team members work closely together and meet regularly to develop personalized treatment plans for all patients. Our goal is to improve our patients’ quality of life and get them back to doing the things they love.
Find The Right Partners
UC is a chronic condition, meaning that youâre going to have it for a long time — probably the rest of your life. You want to form a good and lasting partnership with a care team you feel comfortable with. Your primary care doctor can refer you to a gastroenterologist or IBD program, but you can also get referrals from friends , online support groups, or through the Crohnâs and Colitis Foundation database.
Good partners for your UC journey can include more than just your care team. Look for guidance from other people with UC. You can find them through in-person or online support groups.
âWe often pair patients up with a mentor, someone else who has gone through the same surgery or undergone a similar course of treatment,â Dalal says. âThey can provide a different perspective than a provider can. This is a very good resource, especially when youâre faced with a big decision like undergoing surgery.â
Ask about support groups or mentor programs at your hospital, or find local support through the Crohnâs and Colitis Foundation.
Also Check: How To Cure Peptic Ulcer Disease
How Do Doctors Treat Symptoms And Complications Of Ulcerative Colitis
Doctors may recommend or prescribe other treatments for symptoms or complications of ulcerative colitis. Talk with your doctor before taking any over-the-counter medicines.
To treat mild pain, doctors may recommend acetaminophen instead of nonsteroidal anti-inflammatory drugs . People with ulcerative colitis should avoid taking NSAIDs for pain because these medicines can make symptoms worse.
To prevent or slow loss of bone mass and osteoporosis, doctors may recommend calcium and vitamin D supplements or medicines, if needed. For safety reasons, talk with your doctor before using dietary supplements or any other complementary or alternative medicines or practices.
Doctors most often treat severe complications in a hospital. Doctors may give
- antibiotics, if severe ulcerative colitis or complications lead to infection
Diagnosing Inflammatory Bowel Disease
To diagnose Crohns disease or colitis, we start with a comprehensive examination and collecting a thorough history. A number of tests are needed to confirm diagnosis. They may include:
- Colonoscopy and flexible sigmoidoscopy: Used for initial diagnosis, both use a thin, flexible tube with camera to examine different areas, including the colon, small intestine and large intestine to see any ulcers, bleeding and inflammation.
- Upper endoscopy: Uses a thin, flexible tube with camera inserted through the mouth, following the tract to the stomach and upper small intestine to look for bleeding, ulcers and inflammation.
- Capsule endoscopy: A capsule containing a camera is swallowed by the patient to take pictures along the digestive tract not easily reachable by other procedures .
- Laboratory tests: Blood work plus stool samples to check for bacteria and intestinal bleeding.
- CT interography and MR interography: Specialized radiology tests that evaluate the small intestine, an area of the gastrointestinal tract that is beyond the reach of colonoscopy and upper endoscopy, but is often where Crohns disease is present.
- Imaging tests: Collaborating with experts in Radiology for imaging and interpreting gastrointestinal abnormalities, including abdominal x-rays, barium enema, computed tomography , fistulogram and MRI.
You May Like: Ulcerative Colitis Loss Of Appetite
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
You May Like: What To Eat If You Have Peptic Ulcer
How To Treat Ulcerative Colitis
Surgery for ulcerative colitis involves removing the colon and rectum. Often a new rectum is constructed from small intestine and the patient will not require a permanent ostomy bag. This surgery is frequently done in a minimally invasive fashion, using a laparoscopic or robotic approach and small incisions to lessen discomfort and hasten recovery. The surgeons at Piedmont Colorectal Associates have extensive experience in treating ulcerative colitis and can help to decide the best approach for each patient.
Ulcerative Colitis: Treatment And Therapy
The cause of the inflammatory bowel disease ulcerative colitis is not yet known. Therefore, the goal of treatment is to alleviate the symptoms as well as to prolong the symptom-free phases.
Various drugs are used for this purpose: 5-aminosalicylic acid is an anti-inflammatory agent that is prescribed in the form of the precursor mesalazine as tablets, suppositories, foams or enemas. Corticosteroids also have an anti-inflammatory effect and are used either as suppositories, enemas or tablets. Both medications containing the active ingredient mesalazine and cortisone can cause severe side effects. Cortisone in particular can cause long-term side effects.
In severe cases or when cortisone is not effective, some patients receive immunosuppressants . This can have a positive effect on the course of the disease. However, TNF antibodies , which inhibit the inflammatory messenger TNF, can also be considered. When taking immunosuppressants and TNF antibodies, severe side effects such as susceptibility to infections can also occur, and poisoning is also possible.
Which drugs are used in treatment always depends on various factors, such as the extent of the symptoms and how far the inflammation has spread in the intestine, among other factors.
In addition to drug therapy, it is important for those affected to ensure a varied and balanced diet and to avoid hard-to-digest food components and hot spices during an acute episode.
Read Also: Is Ulcerative Colitis An Inflammatory Bowel Disease