How I Began My Journey Healing With Herbs
From age 11 to 20, I took various forms of medications and bled off and on. I remember being 14 and leaving class for the bathroom at least 6 times a day. One day, the bleeding intensified. My mom saw my pale face and brought me to the ER. This type of bleeding continued sporadically throughout my teens.
I finally gained some stability around age 18. My GI prescribed me an immunosuppressant that is often used in chemotherapy. I took the pills and they worked. They worked better than anything I had taken previously. But I couldnt stop getting infections. The first year I took them, I got an upper respiratory tract infection and coughed up blood. In the following years, I kept getting strep throat and horrible cases of the flu.
I was also old enough to do my own research. The side effects of the immunosuppressors alarmed me and included a dangerous form of lymphoma, bone loss, and possible liver damage.
After 3 years, a great surge of clarity and courage reminded me of how urgent it was to stop taking the immunosuppressant and begin healing with herbs and other holistic protocols. At age 21, I stopped taking medications for the first time in 10 years and began a journey healing with herbs and diet. I was no longer willing to harm the rest of my body with the medications in order to protect a single area: my colon.
Here are a few key things I realized during my transition to holistic healing:
How Does Alcohol Affect Crohns
Various triggers can cause Crohns flare-ups. Crohns is a chronic condition, meaning its with you for life. Since your digestive tract is ground zero for Crohns, living with this condition means careful management of your diet is essential. That includes managing your alcohol consumption.
Alcohol can affect Crohns symptoms the same way it affects pretty much everything else body-related. Those who find that alcohol triggers their flares might notice that consuming too much alcohol can cause problems or make existing symptoms worse.
Even small amounts of alcohol might set off flares in some people, while others might find that they can drink as much as they like without seeing Crohns symptoms.
People might also react differently to different tipples one person might not have the faintest whiff of a flare-up if they drink vodka but may spend hours doubled over in pain after a beer. For the next person, it may be the opposite.
You May Like: Total Wine Ft Myers Hours
How Can Meal Replacement Shakes Be Used With Ibd
Your doctor may recommend considering meal replacement shakes during flare-ups, as is the case with some MyCrohnsAndColitisTeam members: In a Crohns disease flare, wrote one member, my doctor stopped all solid foods to rest my bowels. I was put on Vital nutritional shakes. It was tough. I was also supplemented with Ensure.
Meal replacement shakes may also be recommended to help manage the following IBD-related issues.
Recommended Reading: Venous Leg Ulcer Dressing Treatment
Commercial Meal Replacement Shakes And Protein Powders
Commercial meal replacement shakes are intended to provide a person with important nutrients and boost their calorie intake. Commercial protein powders may be helpful if you have a hard time getting enough protein from the food you eat. One MyCrohnsAndColitisTeam commenter said, Boost and Premier protein meal replacement shakes have often been the only things that will stay in my tummy, along with oatmeal.
Can Surgery Affect Nutritional Status

Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Don’t Miss: What To Eat With Gastric Ulcer
Do I Need To Follow A Specific Diet If I Have Ulcerative Colitis
There is no specific diet for ulcerative colitis and you will only make short term modifications to your diet to preserve or promote your nutritional status or to improve symptoms. It is important to note that dietary changes can only help to improve symptoms and will not reduce inflammation in your bowel.
Youre Avoiding Certain Healthy Foods
It can be hard to eat a healthy diet or anything at all if youre experiencing abdominal pain, cramps, or nausea. But if youre not eating the right foods, you could be at risk of nutrient deficiencies, malnutrition, and unwanted weight loss.
While theres no one meal plan that works for everyone, many people find they can tolerate low-fiber fruits , lean proteins, cooked veggies, and grains like sourdough and oatmeal. A doctor or dietitian who specializes in IBD can help you develop a personalized meal plan.
Read Also: Vitamin E And Ulcerative Colitis
You Need An Adjustment Of Your Meds
Antibiotics for an infection outside of your gut could aggravate UC symptoms. Let your doctor know if you start to experience diarrhea after starting antibiotics, since a switch in the type of drug might be needed.
Your doctor may also suggest taking an antidiarrheal medication or a probiotic, which may help reduce diarrhea.
What Is Uc Again And Why Does Diet Matter
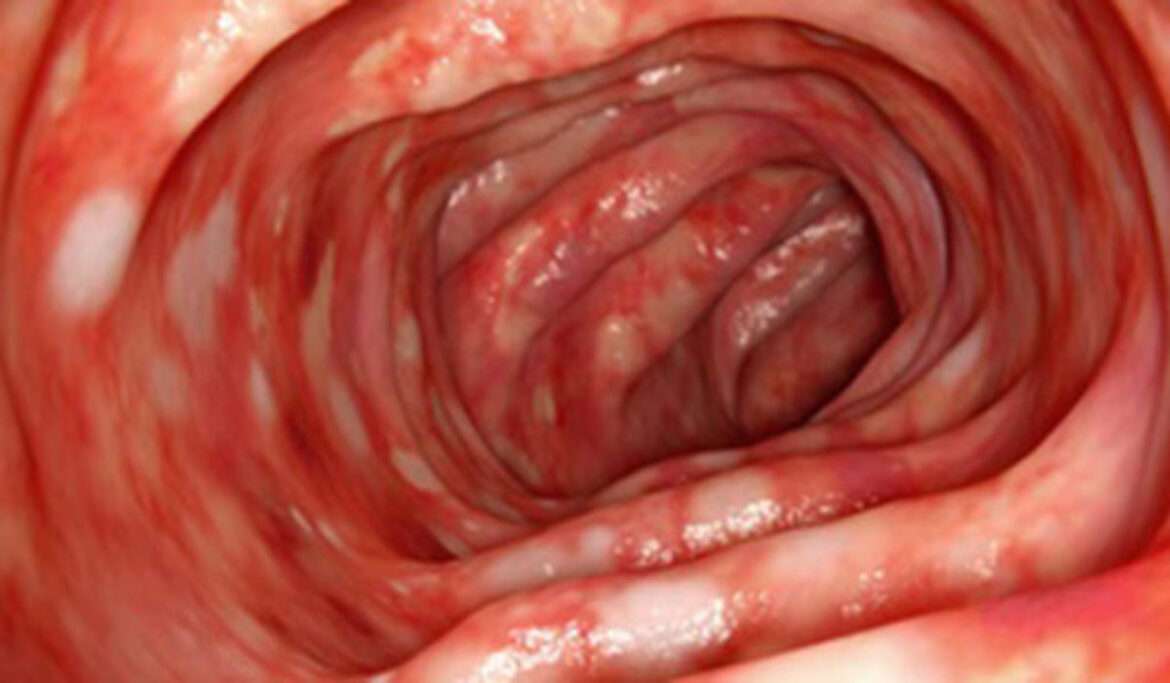
If youre reading about UC and diet, you probably have some of the basics already down but just in case this is all new to you: Ulcerative colitis causes chronic inflammation in the colon and rectum, triggering frequent and urgent diarrhea, bloody stools, and abdominal pain and cramping.
Its not just a poop problem though. It can lead to nutrient deficiencies, actual malnutrition, and weight loss along with body-wide inflammation, which can spur joint pain, fatigue, and more. And these are all issues that can be influenced for better or worse by what you eat .
Whats tricky, though, is that theres no specific ulcerative colitis diet.
In fact, there isnt even a set list of trigger foods that applies to every single person with UC.
Just like everyones specific set of UC symptoms is unique, so too are their problem foods. So, what the heck are you supposed to do with that? Find yourself a guide, thats what.
The best way to figure out how to make your diet work for your UC is to seek the advice of a registered dietitian. Ask your gastroenterologist if they can refer you to an R.D. they trust.
In the meantime, get up to speed on which foods do commonly worsen symptoms in people with UC, along with what goes into a healthy diet in general. While you cant manage UC with diet alone, arming yourself with this knowledge can be a key piece of the puzzle.
Read Also: Can You Drink Alcohol If You Have Ulcerative Colitis
Read Also: Can Diet Help Ulcerative Colitis
Hummus With Pita Chips
This chickpea-based dip packs in a lot of plant-based protein, iron, and folate. Chickpeas are usually well tolerated during ulcerative colitis flares, even though theyre a good source of fiber.
Hummus is also high in healthy unsaturated fat. The right types of dietary fat can help you gain back any weight you might have lost during an ulcerative colitis flare.
You should also avoid high fiber whole-wheat chips if youre in the middle of a flare. Use pretzels or pita chips for dipping instead.
These versatile legumes are loaded with protein, folate, iron, and a type of soluble fiber called raffinose. Bacteria produce the fatty acid butyrate in your digestive tract when they break down this fiber.
Butyrate helps bring down inflammation in the colon. Research suggests that people with inflammatory bowel diseases , like ulcerative colitis, may not produce as much of this gut-healthy fatty acid.
To make this crunchy treat, toss one can of chickpeas in 2 teaspoons of olive oil. Dust with a little bit of garlic powder.
Place the coated chickpeas on an oiled cookie sheet. Brown them in the oven at 350°F for about 45 minutes.
rich in potassium . People with irritable bowel disorders, like ulcerative colitis, are often deficient in this mineral.
Blend one cup of low fat milk with one cup of yogurt, a ripe banana, and ice. Choose a dairy-free alternative if youre sensitive to lactose. Youll get a filling and nutritious snack that you can take with you on the go.
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
Read Also: What Does An Ulcer Look Like
Also Check: Remicade Infusion For Ulcerative Colitis
Diagnosing Back Pain In Ulcerative Colitis
Diagnosing back pain as a symptom of ulcerative colitis can be tricky. Back pain can be attributed to a number of causes, including injury and strain. Because of the other potential causes, some people may not think to mention their backaches when seeking care for their UC. Whats more, back pain may develop years before UC does, making it more challenging to note the connection between the two.
If your doctor suspects that your UC has led to axial arthritis or ankylosing spondylitis, they will likely ask you to come in for a physical exam and tests. During this exam, they may test the range of motion in your spine and gauge your ability to take a deep breath. The doctor may also try to pinpoint the location of your pain by moving your legs or pressing on certain areas of your pelvis.
Radiographic tests are also commonly used to diagnose axial spondyloarthritis. Your doctor may use an X-ray to check for damage to your bones or joints. If no inflammatory damage is visible on the X-ray, your doctor may also order an MRI scan to get a more detailed view of your soft tissue and bones. An MRI scan can be particularly helpful, as it can allow doctors to catch and start treating your axial arthritis or AS before damage becomes extensive.
Also Check: Budesonide Vs Prednisone For Ulcerative Colitis
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Read Also: Is Burping A Sign Of An Ulcer
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Make Sure Youre Getting Enough Probiotics And Prebiotics
Whether you take probiotics tablets, eat fermented vegetables or other fermented products, or take kefir, I personally try to intake something with probiotics and prebiotics at least a few times a week. My personal favourite is a kefir smoothie its an excellent combination of probiotics and prebiotics! Learn more about how to choose the right probiotics here.
Don’t Miss: How To Get Rid Of Tongue Ulcers
Do Patients Living With Ulcerative Colitis Adhere To Healthy Eating Guidelines A Cross
Published online by Cambridge University Press: 24 September 2014
- Michelle Walton
- Affiliation:Department of Sport, Health and Nutrition, Leeds Trinity University, Brownberrie Lane, Horsforth, Leeds LS18 5HD, UK
- Ieva Alaunyte*
- School of Health Sciences, Liverpool Hope University, Hope Park, Liverpool L16 9JD, UK
- *
Common Mistakes That Can Make Ulcerative Colitis Worse
Too much stress and not enough fluids are just a couple of things that can worsen your UC. Find out what else makes the list.
When youre in the midst of an ulcerative colitis flare, its easy to blame last night’s spicy dinner or this mornings extra-large cup of coffee. But even though there are plenty of well-known dietary and lifestyle triggers, flares can sometimes be unpredictable.
While theres no foolproof way to prevent a flare-up, there are certain steps you can take to minimize your symptoms and reach remission faster.
Here are 10 common mistakes you might be making correct them, and you may start feeling better, faster.
Also Check: Do Stomach Ulcers Cause Gas
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, thesymptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Study Design And Participants
In the present cross-sectional study, the diet adequacy and food avoidance habits of UC patients in the UK were investigated. The study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the ethics committee of a UK Higher Education Institution. Written informed consent was obtained from all participants.
A total of ninety-seven UC patients were recruited across the UK from the National Association for Colitis and Crohn’s Disease registers by e-mail, posts in UC forums and social media sites. The inclusion criteria were as follows: aged 1865 years and no history of UC-related surgery.
Initially, four participants participated in a pilot study to ensure that the questionnaire and 24 h dietary recalls were readable and not distressing.
You May Like: Ulcerative Colitis And Anxiety Attacks
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohn’s Disease and ulcerative colitis.
Liquid Supplements for Crohn’s Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Youre Not Avoiding Trigger Foods

Theres no food or food group that causes or cures ulcerative colitis, Yun explains. But many people with UC say that certain foods either bring on symptoms or make them worse.
During a flare-up, your doctor may recommend adjustments to your diet. This can mean avoiding foods that trigger symptoms such as bloating, diarrhea, or cramping. For example, dairy products can be particularly irritating for people who have both UC and lactose intolerance.
Aside from dairy, common trigger foods include beans, whole grains, nuts, seeds, some raw fruits and vegetables, high-fat foods, sugary foods, and sugar alcohols. If youre trying an elimination diet to determine which of these foods you need to avoid, keep a food diary, and always work with a healthcare practitioner to ensure youre getting all the nutrients you need.
Don’t Miss: What Happens With Ulcerative Colitis