Monitoring Considerations For Recommendations 24
The panel suggests that along with maintaining a good standard of DFU care, dressings should be monitored and changed when soiled or when strikethrough is observed, and not placed on wounds for periods exceeding the manufacturerâs recommendations for use. Otherwise, the panel encourage the inclusion and capture of different dressing types in High Risk Foot Service database monitoring systems to benchmark the different dressing typesâ efficacy on local DFU healing.
What Are Neurotrophic Ulcers
Neurotrophic ulcers occur primarily in people with diabetes, although they can affect anyone who has impaired sensation in their feet. They can be found anywhere on your feet, but they usually develop on the parts of your feet and toes that are most sensitive to weight .
Neurotrophic ulcers dont cause pain. But they can be serious if they arent treated promptly or they dont respond to treatment.
A neurotrophic ulcer might be the following colors:
- Any combination of those colors.
The thin borders of the ulcers are punched out, meaning that theyre taller than the surrounding tissues.
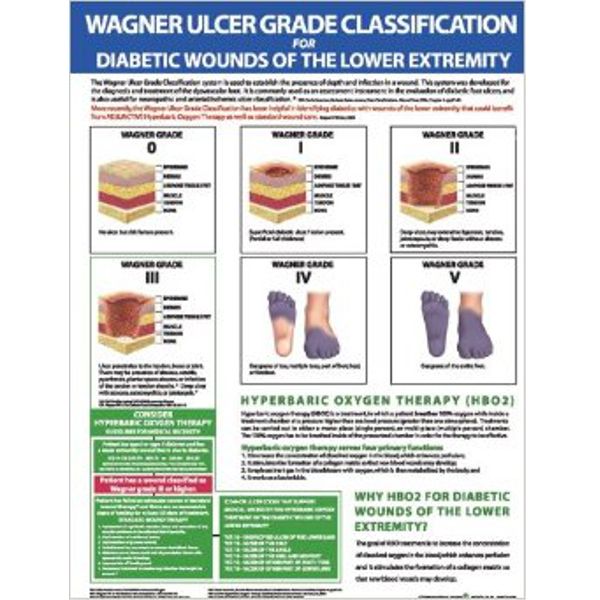
Diabetic Lower Extremity Wounds
There is one diabetic related amputation performed every 20 seconds with over 2,500 limbs being lost per day due to infection and a poorly controlled disease process.1 25% of those with diabetes will have a lifetime risk of developing a lower extremity wound with more than 50% of those becoming infected requiring hospitalization.2 Once an individual has had a lower extremity wound they carry a 68% risk of reamputation over 5 years unless one changes their habits and life styles.3 All of this can be prevented with a team approach towards care and a focus on prevention.4
A diabetic foot ulcer is an open sore or wound that is commonly located on the bottom of the foot. Diabetes is currently the leading cause of all non-traumatic lower extremity amputations in the United States.
Also Check: Manuka Honey For Leg Ulcers
How To Treat Ulcers
If you do get an ulcer or notice a change in your skin that youâre not sure about, tell your doctor right away. Youâll likely get a procedure called debridement, which removes unhealthy tissue from the wound to spur healing.
Your doctor will also work with you to try to keep your sore or ulcer from getting infected and becoming bigger. Some of the steps they may recommend include:
Clean your ulcer daily. Use soap and water, unless your doctor recommends another cleanser. Donât use hydrogen peroxide or soak your wound in a bath or whirlpool, because this could reduce healing and may boost your odds of infection.
Keep your ulcer bandaged or covered with a wound dressing. While you may have heard that itâs important to âair outâ wounds, experts now know that not covering a wound actually increases the odds of infection and slows healing.
Keep pressure off your ulcer, especially if itâs on your foot. This may mean you need to use crutches, special footwear, a brace, or other devices. Reducing pressure and irritation helps ulcers heal faster.
Use the topical medications your doctor recommends. These may be saline, growth factors, and/or skin substitutes.
Keep your blood sugar under control. In addition to reducing your risk of ulcers, tight blood sugar control helps your body heal existing ulcers.
What Are Foot Ulcers
A foot ulcer is an open sore on the foot.
A foot ulcer can be a shallow red crater that involves only the surface skin. A foot ulcer also can be very deep. A deep foot ulcer may be a crater that extends through the full thickness of the skin. It may involve tendons, bones and other deep structures.
People with diabetes and people with poor circulation are more likely to develop foot ulcers. It can be difficult to heal a foot ulcer. In people with these conditions, even a small foot ulcer can become infected if it does not heal quickly.
If an infection occurs in an ulcer and is not treated right away, it can develop into:
- A spreading infection of the skin and underlying fat
- A bone infection
- Gangrene. Gangrene is an area of dead, darkened body tissue caused by poor blood flow.
Among people with diabetes, most severe foot infections that ultimately require some part of the toe, foot or lower leg to be amputated start as a foot ulcer.
Foot ulcers are especially common in people who have one or more of the following health problems:
- Peripheral neuropathy. This is nerve damage in the feet or lower legs. Diabetes is the most common cause of peripheral neuropathy. When nerves in the feet are damaged, they can no longer warn about pain or discomfort. When this happens, tight-fitting shoes can trigger a foot ulcer by rubbing on a part of the foot that has become numb.
In addition to diabetes, other medical conditions that increase the risk of foot ulcers include:
Read Also: Is There A Test For Ulcerative Colitis
Advanced Therapies For Diabetic Foot Ulcers
Physicians of individuals with diabetic foot ulcers may have difficult decisions to make if wounds do not heal. Many of these patients have a significant cardiac risk and health care practitioners need to make complicated decisions about whether to perform invasive procedures like angiography. Other options can be:
- Covering the wound with cultured human cells.
- Heterogenetic dressings or grafts with recombinant growth factors.
- Hyperbaric oxygen therapy.
Proper Dressing Infection Control And Offloading
Its essential to use the proper types of wound dressing, infection control, and offloading to prevent your diabetic wound from regressing during or after treatment.
The best wound dressing maintains a healthy amount of moisture on the foot to create a favorable environment for the wound. It must be changed at least once or twice per day, depending on the stage and severity of the ulcer. Wound dressing helps control infection, as do antibiotics.
Offloading is also a very important but often overlooked component of diabetic foot ulcer treatment. When you offload, you remove pressure from your injured foot and give new, healthy cells the opportunity to thrive. Crushes, knee scooters, and wheelchairs all accomplish offloading.
Don’t Miss: Gastric Ulcer Treatment In Horses
Help To Prevent The Formation Of Diabetes Foot Ulcers
Different assessment methods are available to detect diabetic peripheral neuropathy:
- Doppler ultrasound
Up to
of diabetic foot-related amputations can be prevented with a holistic approach.
Up to 85 percent of diabetic foot-related amputations can be prevented with a holistic approach that includes:
- Optimal diabetes control
- Restoration of pulsatile blood flow
Improving Extremity Blood Flow
Without adequate blood flow to the bottom of the foot, diabetic wounds will never heal. We may recommend non-invasive vascular tests to determine your base-line blood flow into your lower extremities. If there are any questions of blockages or abnormal values, we will refer you to a vascular specialist who can assist with getting optimal blood flow to the areas in the foot/ankle that need it the most.
You May Like: How Do You Get Mouth Ulcers
Diagnosis And Treatment Of Diabetic Foot Ulcers
The primary goal in diabetic foot ulcer treatment is healing the wound as soon as possible. The faster the healing, the less chance exists for infection and amputation. There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Removing dead skin and tissue, called debridement
- Applying medications and/or dressings to the ulcer
- Prevention of infection
- Removing the pressure off the area, called off-loading
- You may be asked to wear special footgear such as a brace, castings, etc.
- Managing blood sugar levels and other health problems
- Adequate circulation
Not all ulcers are considered infected however, if your physician diagnoses an infection, a diabetic foot ulcer treatment program of antibiotics, wound care, and possibly hospitalization may be required.
Symptoms Of Diabetic Ulcers
Look for signs of bleeding or infection on or around the persons feet. Blood or discharge, an infectious odor, or sections with yellow discoloration can reveal that an infection has taken hold. If any areas have turned black, that indicates gangrene, or tissue death. The same rules apply if the infection is present in a different location, such as the hands, legs, or anywhere on the skin.
Also Check: Does Stomach Ulcer Cause Chest Pain
How Does Hbot Help Your Diabetic Wounds Heal
Oxygen can only make its way through the blood within red blood cells. Since the circulation problems associated with diabetes slow the movement of red blood cells, important tissues become deprived of oxygen.
Without enough oxygen, cells struggle to produce the energy they need to block bacteria, synthesize new collagen, or regenerate and repair after injury. This is why diabetic wound healing slows until it comes to a full stop. Inhaling the concentrated flow of oxygen provided through regular HBOT treatments makes it possible to overcome oxygen deficiencies and stimulate a more effective healing process.
Treatment Of Active Infection
Wound infection is a known predictor of poor wound healing and amputation. The appropriate recognition of infection and treatment with antibiotics in diabetic foot infection is imperative to improve outcomes. Conversely, inappropriately treating with antibiotics, often in the setting of fear of missing an infection, to reduce bacterial burden or prophylaxis is associated with several adverse effects, including antibacterial resistance. The IDSA has outlined specific guidelines for the treatment of diabetic foot infections. The IDSA recommends treatment of wounds with at least two signs or symptoms of inflammation or purulent secretion. It is recommended that, before antibiotic therapy, a deep tissue culture via biopsy or curettage after debridement be obtained. Swab specimens should be avoided, especially in inadequately debrided wounds. Antibiotic therapy should be targeted to aerobic Gram-positive cocci in mild to moderate infections. Severe infections should be treated with broad-spectrum empiric antibiotics pending cultures. IDSA recommends 1- to 2-week antibiotic course for mild infections and 23 weeks for moderate to severe infections, but antibiotics can usually be discontinued once clinical signs and symptoms of infections have resolved. To avoid antibacterial resistance and other adverse outcome of therapy, it is best practice that treatment of clinical diabetic foot infections be completed with narrow=spectrum antibiotics for the shortest duration possible.922
You May Like: Carnivore Diet For Ulcerative Colitis
Caring For Wounds And Foot Ulcers In Diabetic Patients
The Centers for Disease Control and Prevention reports that there are 30.3 million people living with diabetes in the United States. Diabetes comes with many serious complications, including chronic wounds, nerve damage and foot ulcers.
The American Podiatric Medical Association reports that 15 percent of diabetic patients will develop a foot ulcer. Further, diabetes is the leading cause of nontraumatic, lower-extremity amputations in the U.S. caused by infected wounds and foot ulcers that cannot heal. While difficult to treat, foot ulcers often can be prevented.
Controlling risk factors and monitoring the skin daily is key to minimizing the negative effects of diabetes, said Nancy Estocado, Advanced Wound Care Clinical Coordinator at Sunrise Hospital and Medical Center. For anyone with diabetes, understanding how to prevent and properly address wounds especially foot ulcers is integral to living a healthy life.
Preventing Diabetic Foot Ulcers
There are several ways to prevent a foot ulcer. In addition to daily checks of your feet for any signs of an ulcer or other abnormality, the following can be done to help with prevention:
- Never walk barefoot, and always wear socks to protect your feet
- Wear shoes that fit properly and do not rub
- Keep your blood sugar under control and monitored
- Eat a healthy diet
- Avoid alcohol and tobacco products
- Seek immediate medical attention if you have a foot wound that is not healing
You May Like: Diet Plan For Someone With Ulcerative Colitis
Diabetic Foot Ulcer Management
After practicing standard care practices, the best Diabetic Leg Ulcers specialist in Oxnard can then decide whether it is suitable to practice an advanced treatment. Treatment choices will differ according to the patient and the wounds requirements.
Growth Factors
Becaplermin 0.01% is the recombinant human platelet-derived growth factor licensed by the Food and Drug Administration and adopted in cases of full-thickness lower-extremity diabetic ulcers by sufficient blood flow. It is a topical agent that stimulates and strengthens the wound treatment process.
Medical trial data confirmed that becaplermin benefits in reducing the danger of amputation, plus more than one-third DFUs treated in the existing group with regular RH PDGF-BB Vs. The Placebo limitation group. At week 20.1, Becaplermin has been confirmed to contribute a 43% greater healing rate for neuropathic ulcers than a placebo gel.
Collagen Products
Many collagen dressings happen to be derived from a mixture of sources, like porcine, bovine, equine, plus avian. Collagen-based dressings come in pads, particles, gels, and paste types based on the company selling them. DFUs are identified to come with a continued inflammatory response plus extracellular matrix irregularity. Collagen dressing companies support and formulate a scaffolding model that controls extracellular components, consequently moving chronic injuries toward closure.
Tissue-Based and Cellular Products
What To Expect At Home
Diabetes can damage the nerves and blood vessels in your feet. This damage can cause numbness and reduce feeling in your feet. As a result, your feet are more likely to get injured and may not heal well if they are injured. If you get a blister, you may not notice and it may get worse.
If you have developed an ulcer, follow your health care provider’s instructions on how to treat the ulcer. Also follow instructions on how to take care of your feet to prevent ulcers in the future. Use the information below as a reminder.
You May Like: How To Treat Ulcerative Colitis At Home
Subgroup Considerations For Recommendations 78
Geographical remote people
Surgical procedures on DFU and the use of NPWT thereafter are likely to be instituted in a large tertiary or regional hospital or community settings, which may not be in close proximity to people living in geographically remote areas. Continuation of NPWT upon discharge also relies upon the availability of competent staff as well as access to NPWT equipment, which again may be unavailable in geographically remote areas. When implementing NPWT in surgically treated DFUs in people from geographically remote areas, health professionals should consider the access to NPWT equipment and availability of competent staff to facilitate NPWT treatment. The panel also recommends discussion of the potential desirable and undesirable effects with patients so an informed decision can be made. Staff in geographically remote areas may also consider undertaking training to overcome any skill gap, including in provision of post-hospital discharge NPWT with portable devices or NPWT single use dressings.
Aboriginal and Torres Strait Islander people
Other subgroup considerations.
The panel is unaware of any subgroups for which NPWT would be unacceptable.
When You Need More Treatment
If your wound doesnât heal in about a month or becomes an infection that spreads to the bone, you may need other treatments. These can include surgery and hyperbolic oxygen therapy, which involves breathing pure oxygen in a special room in order to help your body heal.
If your ulcer develops gangrene and your tissue dies, your doctor may have to amputate that area of your body.
Don’t Miss: What To Drink With Stomach Ulcer
Implementation Considerations For Recommendations 24
Recommendation 2
In the absence of evidence supporting superiority of one dressing product over another for healing DFUs, dressing selection is paramount as part of a good standard of DFU care. The panel suggests that a good standard of DFU care includes a comprehensive DFU assessment, appropriate debridement, appropriate wound dressings, antimicrobial management if infected, revascularisation considerations if ischaemic and the best available offloading device provided for the patient .
Recommendation 3
Please refer to Recommendation 2 for similar implementation considerations, as well as the panelâs definition of a good standard of wound care for DFU.
Recommendation 4
How Can I Tell If Im Getting An Ulcer On My Foot Or Toe

When an ulcer is starting to develop on your foot or toe, you might notice changes in your skin like:
As the ulcer gets worse, it can get wider, and longer and deeper sometimes down to the bone. In advanced stages you might see:
- A halo around the center of the wound that feels harder than the skin around it.
- Drainage , which is a sign that you might have an infection.
- A brown discoloration.
Don’t Miss: Extra Virgin Olive Oil And Ulcerative Colitis
Keeping Your Feet Healthy
Patients with diabetes must be diligent about wound prevention. The first step is properly managing the diabetes itself which includes maintaining a balanced diet and exercise routine, keeping blood glucose levels in the recommended range, avoiding alcohol and tobacco, and addressing any co-occurring disorder such as cardiovascular disease or obesity.
The next step is to commit to daily skin inspections, and especially your feet when sensation is impaired, Estocado said. This inspection should be thorough, and include the sole, sides and in between the toes. Even the smallest blister or scrape can escalate for diabetic patients, so call your doctor at the first discovery of any abnormality.
How Do Diabetic Foot Ulcers Form
One of the most common complications of diabetes is neuropathy, or nerve damage. Neuropathy often damages the nerves in the hands and feet, which can prevent people with diabetes from feeling a small scrape, cut, or blister when it first occurs.
Though an injury to the foot can start out as a small scrape, having diabetes affects the bodys ability to heal even these small injuries. This is due to a combination of factors including:
-
Existing foot deformities
-
High blood glucose levels
This can lead to the formation of what is known as a complex or chronic wound. The most common complex wounds affecting people with diabetes are DFUs, which can increase the risk of amputation.
Generally when people talk about complex wounds, it means a wound that has a hard time closing on its own, said Dr. Nikolai Sopko, chief scientific officer at PolarityTE, the developer of SkinTE, a treatment for foot wounds that may be more effective than current treatments for healing open wounds. A clinical trial is now recruiting participants who have developed a DFU to investigate SkinTE .
A diabetic foot ulcer essentially starts out as a blister, but you cant feel that it hurts because the nerves are impaired, he said. Diabetes can also impair to the foot, so on top of developing a that you cant feel, your skin doesnt have all the blood it needs to enact a repair response.
Also Check: Can Ulcerative Colitis Cause Fever